Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
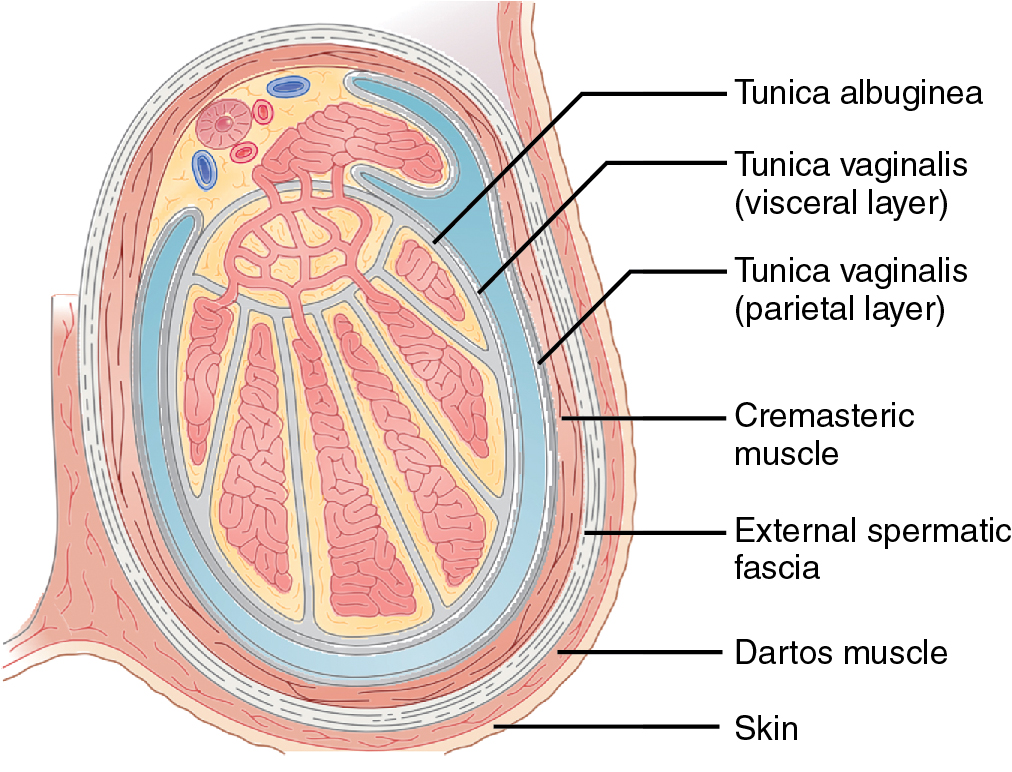
The testes, the principal male reproductive organs, are located within the scrotal sac, and surrounded by a thick layer of fibrous capsule and the tunica albuginea ( Fig. 30.1 ).
The tunica albuginea forms a capsule that covers the testis. The testis is then further covered by a reflected fold of the processes vaginalis that becomes the visceral layer of the tunica vaginalis, with the remainder of the peritoneal sac forming the parietal layer of the tunica vaginalis.
The visceral layer of the tunica vaginalis covers the inelastic tunica albuginea. The parietal layer of the tunica vaginalis covers the anterior and lateral parts of the testes.
The epididymis consists of three segments: the head (globus major), the body, and the tail (globus minor). The epididymis leaves a ‘bare area’ to which the mesentery of the testis is attached.
Most primary testicular neoplasms are of germ cell origin and have many histological subtypes, but it is of primary importance to make the distinction between two basic tumor types: seminomas and nonseminomatous germ cell tumors.
Ultrasonography (US) is the mainstay of scrotal imaging. It plays an important role in localization of masses (intratesticular or extratesticular) because extratesticular solid masses are most likely benign. US is also helpful for active surveillance of low-risk small testicular lesions.
Color Doppler imaging allows visualization of intratesticular blood flow, which is either reduced or absent in torsion, and the vascularity in solid masses. Technical factors, including equipment and operator experience, may limit the quality of the study. Techniques, including power Doppler imaging and the use of contrast agents, may improve detection of intratesticular flow.
Magnetic resonance imaging (MRI) can characterize testicular lesions but is not indicated for primary screening.
The normal testis demonstrates homogeneously intermediate signal on T1-weighted images and hyperintense signal on T2-weighted images compared with skeletal muscle ( Fig. 30.2 ).
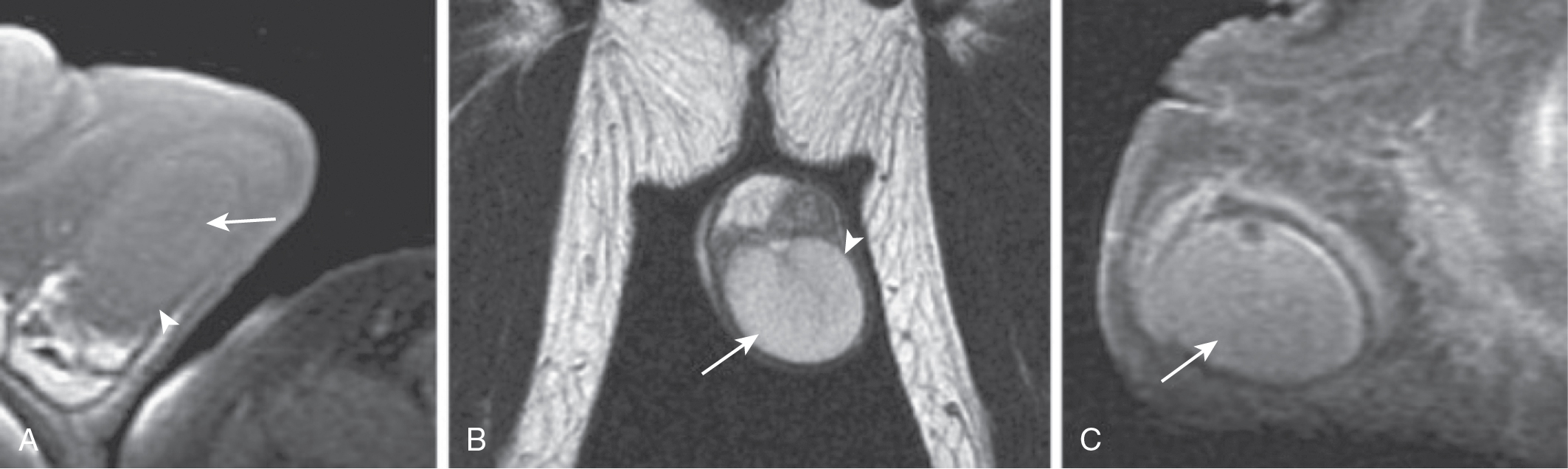
The mediastinum testis shows isointense T1-weighted and hypointense T2-weighted signal compare with the testicular parenchyma.
The tunica albuginea surrounding the testis appears hypointense on both T1-weighted and T2-weighted images.
The epididymis is somewhat heterogeneous with isointense T1-weighted signal and hypointense T2-weighted signal compared with the testis.
The scrotal sac is hypointense on both T1-weighted and T2-weighted images.
On dynamic contrast enhanced (DCE) T1-weighted imaging, the testis shows homogeneous enhancement, while the epididymis appears relatively hyperintense.
DCE MRI can differentiate segmental testicular infarction, testicular torsion, and testicular necrosis.
Computed tomography (CT) is usually not indicated for primary diagnosis or screening but is reserved for testicular cancer staging by screening for retroperitoneal lymphadenopathy.
US is the modality of choice for evaluation of a palpable testicular mass. The key is to determine if the palpable lesion is intratesticular or extratesticular. All intratesticular masses are considered malignant until proven otherwise, whereas most extratesticular masses are benign.
MRI may be helpful as a problem-solving tool when testicular ultrasonography is indeterminate.
Appropriate patient positioning is essential for imaging of the scrotum. The penis is dorsiflexed against the anterior abdominal wall and is taped in place to prevent motion.
Standard anatomic sequences.
Axial, sagittal, coronal localizer.
Axial, coronal, sagittal T2-weighted fast spin echo (FSE): small (16-cm) field-of-view (FOV) and thin-section (4-mm) nonfat-suppressed FSE T2-weighted sequences with relatively high resolution (matrix of 256 × 192 or higher).
Axial T1-weighted spin echo.
Additional sequences for trauma, inflammation, or tumor.
Axial diffusion weighted imaging.
Axial T2-weighted fat-suppressed FSE or short T1 inversion recovery.
Full-FOV T2-weighted imaging through the pelvis in cases of known or suspected infection or malignancy.
Axial postcontrast T1-weighted three-dimensional (3D) fat-suppressed spoiled gradient recalled echo (GRE).
Axial T1-weighted dual-echo spoiled GRE (in-phase and out-of-phase).
Axial pre- and postcontrast T1-weighted fat-suppressed 3D spoiled GRE.
US is a convenient tool to diagnose cryptorchidism, but has low sensitivity and specificity in determining the presence and localization of the undescended testes ( Fig. 30.3 ).
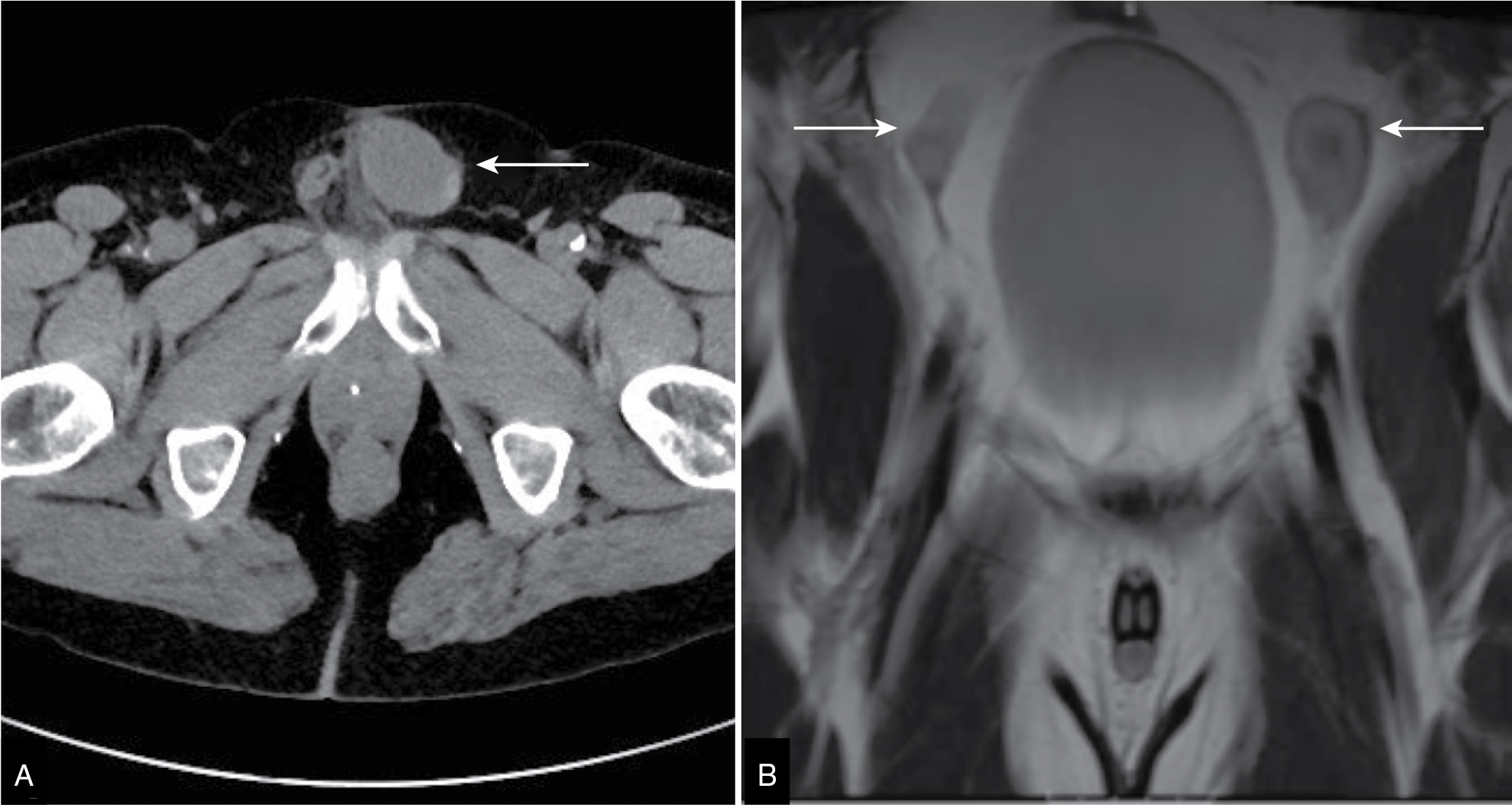
Both CT and MRI are able to localize the undescended testes because of their broad field of view.
CT is excellent for detecting testes in the inguinal canal because of the contrast between the testis and surrounding soft tissues.
On MRI, the hypoplastic testes appear small in size and relatively low in T2-weighted signal.
Second most common testicular tumor in children less than 4 years old; usually appears as a well-defined complex mass with cystic changes.
Calcification may be seen within the lesion ( Fig. 30.4 ).
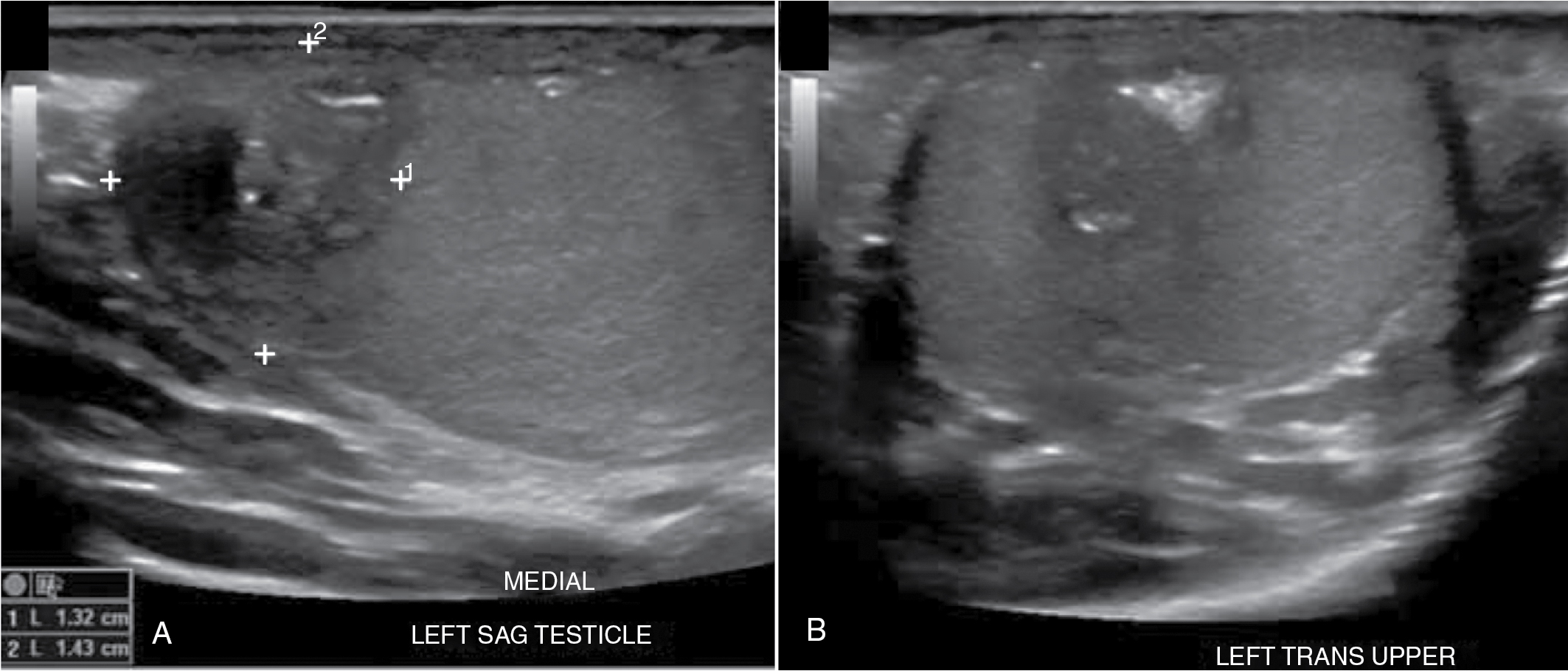
The MRI appearances of teratoma are not characteristic compared with other malignant testicular tumors.
May present with a “target” appearance with a low-signal intensity capsule.
The layers of keratinized material within the lesion are rich in water and lipid and appear as areas of high signal intensity on both T1-weighted and T2-weighted images.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here