Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The results of conventional surgical therapy (e.g., deafferentation) for chronic benign pain syndromes are poor. The results of so-called neuromodulation therapy, neurostimulation, and infusion techniques are continually improving, however, particularly in benign pain syndrome, which has typically been the most challenging to treat. Surgical experience with central deafferentation (e.g., cordotomy) suggested that patients with neoplastic pain achieved satisfactory pain relief more frequently than those with benign pain. This is hardly surprising, as the effects of neural plasticity in patients with a longer lifespan should tend to confound the results of surgical interruption. This was borne out in studies of cordotomy or dorsal rhizotomy. A distinct characteristic of refractory benign pain is that it appears to follow lesions of the nervous system. This is in contrast to malignant pain, which is thought to be nociceptive.
Surgical intervention for chronic benign pain of lumbar origin is associated with high complication rates. The principles of such intervention, however, appear to be based on reasonable principles; these can be appreciated only with a basic understanding of neuropathologic mechanisms.
The immediate effect of injury is to activate receptors in specific nerve fiber types. These include large myelinated Aβ fibers, small myelinated Aδ fibers, and small unmyelinated C fibers. The interaction of these afferents, primarily though not exclusively through the substantia gelatinosa, forms the basis for the gate control theory of pain. The cell bodies of primary nociceptive neurons are located in the dorsal root ganglion, with afferent synapses in layer I or V. Layer I cells are nociceptor specific and somewhat less discriminatory. Layer V cells respond to many inputs, mainly repetitive nociceptive stimuli and nociceptive input. The primary nociceptive neurons synapse on rostrally projecting second-order neurons in the dorsal horn, the theoretical target of the “gate.” After postinjury discharge, the next normal event would be for the fibers to return to rest. In the face of persisting injury, however, repeated firings are provoked; some receptors become more sensitive to subsequent stimulation and can, in fact, fire spontaneously. This sensitization can arise from direct change in the structure of the nociceptor or as a response to substances released in its milieu. As damaged tissue heals with scar formation, granulation tissue containing nerve sprouts and capillaries invades the area. This further changes the local environment and the sensitivity thresholds of the nerve endings. Such changes have relevance in the healing of surgical wounds such as those from laminectomy or spinal fusion; during healing, there may be significant pain problems generated by the wound itself. As would be expected from the nature of neuropathic pain, patients may note localized burning dysesthesias or even allodynia.
The compressed root is susceptible to such damage and all its ensuing consequences. Such roots are further subject to chemical irritation from the inflammatory process and to the resulting edema and ischemia. The end results of these pathologic processes are neural scar formation and demyelination.
The physiologic responses to nerve damage are complex and variable. Devor broadly classifies these into three groups. The first, sensitization of the nociceptor endings, is characterized by a reduced threshold for activation. In such a state, nonnoxious stimuli may become capable of producing pain. Second, the nociceptive fibers themselves become a source of pain when they are activated at abnormal locations along their course; this is the phenomenon of ectopic electrogenesis. Third, pain could result from abnormal central processing of afferent impulses. In the setting of chronic spinal pain syndromes, the first two possibilities are most pertinent, with true central pain syndromes being uncommon.
Chemical and mechanical stimuli can invoke or modify repetitive discharge in the damaged nerve. Epinephrine and norepinephrine can both activate afferent fiber endings in neuromas; these responses are thought to be mediated by α-adrenergic receptors. Sympathetic activity can produce abnormal sensation through neural transmitter release that stimulates afferent nerve sprouts possessing ectopic adrenergic chemosensitivity. The abnormal sensations produced by these mechanisms may explain causalgia and other sympathetic dystrophies along with the potential benefit of sympathectomy for such disorders.
The phenomenon of ectopic electrogenesis, which occurs in neuromas, can also develop in axons that have become demyelinated but remain in continuity. This issue relates directly to chronic low back and leg pain, in which a neuroma would not be expected to form, but in which demyelination of nerve roots is a known complication. Such demyelinated roots may exhibit either hyposensitivity or hypersensitivity. Spontaneous discharge has been shown to occur at sites of peripheral demyelination. These discharge patterns are similar to those found in neuromas. Consequently, nerves with regions of demyelination can demonstrate ectopic electrogenesis, which transfers nociceptor-like information into the central nervous system. Rhythmic firing, a characteristic of cell behavior not elicited until a certain threshold level of generation current is reached, can be provoked in demyelinated regions by mechanical stimuli. This threshold characteristic is important because many injured nerves appear to be poised near the rhythmic firing threshold. As a consequence, brief or weakened stimuli can set off a prolonged discharge that may persist beyond removal of the stimulus. In experimental preparations, tetanic stimulation produces this so-called after-discharge, which is followed by a period of prolonged electrical silence. It is evident that this could have implications for pain relief from neuromodulation, such as spinal cord stimulation (SCS).
The dorsal root ganglion is mechanically quite sensitive in its normal state. Some discharge occurs spontaneously even at baseline. Postdischarge, stimulation is common. This baseline excitability is heightened after peripheral nerve injury. In this instance, the dorsal root ganglion contributes ectopic barrages above and beyond those generated by the region of peripheral injury. The state of excitability of the dorsal root ganglion is thus of clinical importance in root compromise. In the chronically injured root, deafferentation in the form of ganglionectomy would, theoretically, remove this focus of irritability.
Damage to a peripheral nerve causes changes central to the lesion that may not be reversed by treating the original injury. As noted earlier, these central changes include heightened sensitivity of the dorsal root ganglion to mechanical distortion and to neurotransmitters. Axons central to a nerve lesion also diminish their conduction velocity. Cells in the dorsal root ganglion may degenerate, with consequent degeneration of central axons. This leads to substantial loss of afferent fibers, leading to deafferentation, which is another mechanism of pain. Additionally, the central terminals of C fibers change in response to peripheral nerve injury. The result is a failure of feedback mechanisms that produces prolonged depolarization and inhibition. Peripheral nerve section is thus followed by a reduction in inhibition of afferent fibers. The cord “responds” to diminished input (deafferentation) by diminishing inhibitions to the remaining input. The spinal cord itself thus becomes a location for continuing provocation of pain through mechanisms of chronic afferent barrage accompanied by reduced inhibition. Not surprisingly, many central ablative procedures, such as cordotomy, have been proposed as treatments for chronic pain syndromes. However, the role of these more central procedures in the treatment of chronic spinal pain syndromes is limited.
Variability in anatomy also creates additional levels of precision and uncertainty. Recently, Solmaz et al. in a cadaveric study noted that there were an average of 4.8 ± 1.3 fibers consistent with intradural communication between dorsal rootlets of spinal nerves. The number of these intradural communications varied based on the level of the spine. All spanned one level, with the highest frequency in the cervical and thoracic areas. No cadaver had fewer than three, with some as high as seven. Clearly, such anatomic variation would compromise the results of any deafferentation procedure related to the dorsal rootlets.
Finally, the individual motion segment is richly innervated and thus capable of generating postinjury pain in the absence of frank neural compression. Many of the procedures to be discussed are intended for the treatment of continued extremity pain caused by persistent neurogenic dysfunction; such procedures are usually unsuccessful in dealing with disorders of the motion segment per se. Thus, entities such as posttraumatic lumbar strain, postdecompressive segmental instability, and persistent discogenic pain are not well served by deafferentation procedures. Additionally, reversible sources of neural compression producing continued sciatica—such as disc herniation, lateral recess, or central or foraminal stenosis—must be meticulously excluded before the consideration of any of these procedures. Indeed, the most effective way to deal with the “failed back” (failed back surgery syndrome [FBSS]) is to avoid creating it by judicious treatment and surgery. Given the historical and current rates of spine surgery, in the settings of favorable natural history of many degenerative syndromes, it is unlikely that the incidence of FBSS will decrease.
The surgery for chronic pain in this setting has revolved around two concepts: deafferentation and enhancement of presynaptic inhibition. In the first case, the theoretical goal is diminution of the conduction of painful stimuli centrally by interrupting appropriate afferent pathways. Precise determination of these pathways can be difficult because of neuroplasticity, central mechanisms of continuing pain generation, and anatomic variation. In the second approach, enhancement of presynaptic inhibition, the goal is to achieve functional deafferentation by either chemical or physiologic means. Again, neuroplasticity complicates this approach.
Modulatory therapies that are germane to the concept of inhibition are nerve and cord stimulation and subarachnoid implants. Destructive therapies are essentially deafferentation procedures: rhizotomy and ganglionectomy. More central ablative procedures have no place in the current treatment of failed lumbar surgery syndromes. For example, the dorsal root entry zone lesion, produced by electrocoagulation, has been reported to yield a success rate of 54% to 82% in brachial plexus avulsion, 50% in neurogenic pain from spinal cord injury, and nearly 60% in cases of postherpetic neuralgia, or complex regional pain syndrome. However, in benign pain syndromes or arachnoiditis, dismal results have been reported. Cordotomy has been extensively studied in cases of neoplastic pain and can be of major benefit in this instance; some recent reports noted a 90% rate of pain relief in microendoscopically guided percutaneous procedures. The procedure, in which the anterolateral pathways of the spinal cord are divided, thus interrupting pain and temperature transmission, has also been investigated for cases of lower cord or cauda equina injury. Porter and colleagues reported a 62% rate of significant pain relief in follow-up ranging from 8 to 20 years. White and Sweet cited a 60% rate of pain relief in patients with cord injuries and in four of seven with cauda equina damage. A recent review suggested that dorsal root entry zone, midline myelotomy, and anterolateral cordotomies, while continuing to be included in residency and fellowship training, should be “rarely used,” particularly in benign pain syndromes, due to variability in results and the significant nature and frequency of complications (urinary incontinence, sexual dysfunction, and leg weakness). Additionally, genitourinary dysfunction rates of 8% to 92% have been reported.
Little attention in the recent literature has been focused on the use of rhizotomy as a treatment for chronic backache and sciatica. It has been widely investigated in other areas, however. As noted previously, results in tumor patients are generally superior to those achieved in chronic benign pain patients. In a comprehensive review, Barrash and Leavens analyzed dorsal rhizotomy for relief of tumor pain. Promising results of rhizotomy were noted in cases of central neoplasms as well as neoplasms involving the breast, colon, head and neck, lung, and rectal and urogenital systems. The problem of trigeminal neuralgia has been widely addressed as well. van Loveren and colleagues reviewed their experience of 1000 patients with trigeminal neuralgia, comparing the techniques of percutaneous stereotactic rhizotomy and posterior fossa exploration. Of the 700 treated by percutaneous stereotactic rhizotomy, excellent or good results regarding pain relief were achieved in 125 patients treated with microsurgical vascular decompression or partial sensory rhizotomy. These favorable results were corroborated by the report of Bederson and Wilson in 252 patients. Additionally, glycerol rhizotomy for trigeminal neuralgia has been investigated. In general, good or excellent results are reported in 70% to 72% of the cases using this technique. Outcomes of intradural rhizotomy for neuropathic pain syndromes may be less favorable over time, however. A recent retrospective study of 55 patients treated by intradural cervical dorsal root rhizotomy for refractory occipital neuralgia reported a functional improvement of 57% at follow-up of 14 years. Interestingly, this is less than the rate reported for full pain relief (64%).
Selective dorsal rhizotomy for spasticity in children with cerebral palsy, although controversial, has also been recommended. Cahan and colleagues and Kundi and colleagues emphasized the safety of the procedure, citing preservation of cortical somatosensory evoked responses. Good results have also been reported by others. Intraspinal rhizotomy has been reported to diminish spasticity in patients with myelomeningocele. Sacral rhizotomy in the treatment of hypertonic neurogenic bladder has also been investigated, as has control of spasticity resulting from posttraumatic paraplegia. Percutaneous radiofrequency rhizotomy resulted in improvement of spasticity in 24 of 25 patients in the series of Kasdon and Lathi. In Turnbull's series, percutaneous rhizotomy improved lower extremity spasm in paraparetic patients who were not hospitalized.
Taken in concert with the results presented for the disorders reviewed earlier, the outcome of rhizotomy for chronic lumbar pain syndromes is particularly grim. In the case of chronic pain patients, preservation of function is essential and the surgeon does not have the latitude to interrupt multiple roots, as is the case in many of the situations reviewed earlier. Additionally, the precise interpretation of pain reduction, which is necessarily subjective, complicates the evaluation of results of rhizotomy or ganglionectomy for chronic benign pain.
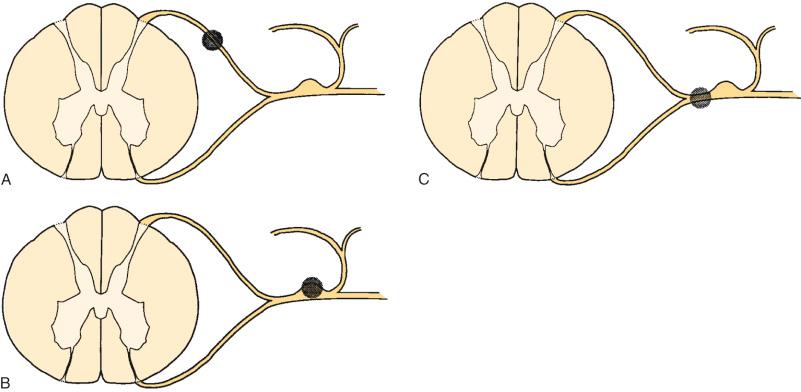
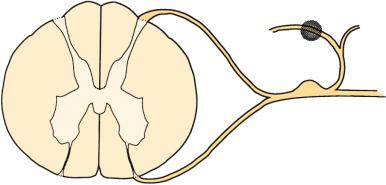
Sectioning of the spinal nerves or excision of dorsal root ganglia can be accomplished at multiple levels. Rhizotomy may be performed by intradural section of the dorsal root, extradural section of the dorsal root, or extradural section of the mixed root ( Fig. 112.1 ). Additionally, the median branch of the posterior primary ramus may be interrupted, although this is usually by a percutaneous technique, such as radiofrequency ablation ( Fig. 112.2 ).
Sensory rhizotomy for the relief of chronic pain was first carried out by Abbe in 1888 but had been nearly abandoned by 1925 because of the relatively high failure rate and the subsequent interest in cordotomy. Rhizotomy may be performed at this level to include selective sensory fibers or it may take the form of a complete rhizotomy. Characteristically, both ablative procedures are performed proximal to the ganglion.
The goal of rhizotomy or ganglionectomy is denervation of the area in which pain is felt. It has frequently been assumed that root section should remove pain that is peripheral and circumscribed because the afferent territory of a few adjacent nerves presumably completely delineates the pain for that region. Long-term results of rhizotomy fail to support this, however. In addition, results of selective sensory rhizotomy may be compromised because of the presence of denervation hypersensitivity, intersegmental cross-linking, and overlapping dermatomes and the presence of afferent unmyelinated axons in the ventral roots. Intraoperative stimulation of these roots has been shown to provoke pain. If these ventral afferents comprise a significant portion of the ventral root, dorsal sensory rhizotomy may be providing insufficient deafferentation to interrupt pertinent sensory pathways.
One of the central problems in planning surgery for persistent limb pain is the precise delineation of the involved roots. Many authors have attempted to select patients on the basis of their response to individual nerve root sheath blockade as guided by electrophysiologic evidence of chronic radiculopathy and neurologic examination. Onofrio and Campa reported their results in 286 cases of rhizotomy, 58 of which were lumbar. Only six of the 45 undergoing S1 rhizotomies reported long-term pain relief. Three of 13 patients who underwent lumbar rhizotomies had clinically successful results. These results were obtained despite consideration of dermatomal overlap and the use of selective nerve root blockade to plan the surgery. Loeser reported similar results with a 14% success rate at 10 years. Arachnoiditis in the setting of failed disc surgery seemed to be correlated with poor results, and preoperative nerve root blocks provided little diagnostic or prognostic information. Loeser offered several reasons for these results, including incomplete root sectioning, inadequate numbers of roots divided, and a higher threshold of fibers in adjacent nerves, which may begin to produce chronic pain syndromes after the effects of local anesthetics from root blocks have worn off. He also speculated that central alterations may be important. Additionally, the utility of “diagnostic” nerve root blocks must be questioned. The selective root sheath injection appears to be nonspecific in not only a dermatomal sense but in a central and peripheral sense as well: several authors have reported on the ability of distal blocks to produce temporary relief. Jain believed that selective extradural sensory rhizotomy was not successful in the setting of arachnoiditis. Other authors have reported similarly discouraging results.
In a compendium of results from multiple sources, Dubuisson noted a 74% rate of immediate success following rhizotomy at L4, L5, and S1, which dropped to 33% 3 months after surgery. These results are corroborated by the reports of others. White, in reviewing a series of sensory rhizotomies for 10 patients with failed lumbar surgery, noted 80% good to excellent results. However, follow-up was variable, ranging from 4 months to 11 years, and no temporal specifics were reported. He did, however, agree that there was little pain relief when arachnoiditis was present. Wetzel and colleagues reported poor outcomes (14% success) in patients undergoing selective sensory rhizotomy at a mean follow-up of 2 years. All patients had undergone previously unsuccessful lumbar surgery.
Thus, it is difficult to recommend rhizotomy for the treatment of chronic benign lower extremity pain. Seemingly, the most reliable indication for rhizotomy is pain caused by deafferentation itself. Tasker and colleagues reviewed 168 patients. The pain was divided into two groups: spontaneous and hyperpathic. In the latter, pain is induced by normally nonnoxious stimulation within adjacent areas of increased somatosensory thresholds. Overall, the pain in this group was nearly always causalgic or dysesthetic in quality and was associated with sensory loss. This was dramatically ameliorated by intravenous sodium thiopental, but not by morphine, and was usually relieved by proximal local anesthetic blockade. Various deafferentation procedures were reviewed, including rhizotomy, neurectomy, cordectomy, and cordotomy; each of these ablative procedures failed to relieve most patients of deafferentation pain. Hyperpathia, which occurred in incompletely deafferented areas, however, was partially relieved by surgical completion of the deafferentation, although the authors noted that pain may persist at the periphery of the sensory loss.
Sectioning of the dorsal root ganglion has been shown to provide the best results in terms of pain relief when performed for benign truncal neuralgias. The results of ganglionectomy (see Fig. 112.1 ) at the caudal lumbar roots in cases of failed lumbar surgery are as disappointing as those reported for rhizotomy. At this time, meaningful differentiation between rhizotomy and ganglionectomy as distinct therapeutic tools in this setting is impossible.
The patient is placed in a prone position under general anesthesia, and hemilaminectomy and partial facetectomy are used to expose the involved root. The root sheath is clearly identified and opened longitudinally for 8 to 10 mm proximal to the dorsal root ganglia. The dural septum, which separates dorsal and ventral roots, is identified, and a small nerve hook is passed between root filaments. Osgood and colleagues noted that several distinct root fascicles are usually present. With electrocautery at a low setting, electrical stimulation is used to distinguish between motor and sensory fibers. As Bertrand has noted, however, caution must be used in relying on this test exclusively because chronically damaged roots may exhibit a higher threshold for motor excitation response than normal roots. Thus, a wake-up test may be required. There are currently no reports in the literature on the use of somatosenory or motor evoked potentials to supplant this. When appropriate sensory fibers are identified, they can be sectioned with electrocautery or a microsurgical blade. Currently, there are no reliably described microsurgical or endosurgical techniques for rhizotomy or ganlionectomy in the particular instance of chronic benign lumbar pain syndromes, although endoscopic techniques have been described for facet rhizotomy.
Facet denervation is not nerve root surgery in the same sense that open rhizotomy is; rather, the theory behind this procedure involves destruction of the median branch of the posterior primary afferent nerve that supplies the facet joint (see Fig. 112.2 ). The median branch of the posterior primary ramus descends through a notch at the base of the transverse process and is covered by a ligament at the anteroinferior border of the facet joint at this level. This ligament is a continuation of the intertransverse membrane; it is here that several small twigs are given off to the facet joint. These twigs then enter the facet joint capsule. Each posterior primary ramus supplies at least two facet joints, and each facet joint receives innervation from at least two spinal levels. Clinical features of facet joint syndrome have been described by several investigators. Mooney and Roberson are generally credited with one of the earliest descriptions. Subsequent authors have attempted to improve the sensitivity and specificity of diagnosis and investigate diagnostic maneuvers, specifically response to facet blockade as selection criteria for facet rhizotomy or even fusion. Saal, in reviewing current diagnostic techniques, noted that the capacity of diagnostic facet blocks to correlate specifically with findings of the history and physical examination is limited. Although a variety of signs and symptoms have been described as being associated with facet-mediated pain, these signs or symptoms are not specific enough to delineate a patient population suffering from facet-mediated pain per se. Several studies have noted that the prevalence of facet pain among patients with chronic back pain is relatively low when measured by facet injection; however, the anesthetic response to a single uncontrolled block is as high as 50%, an unacceptably high false-positive rate. It is generally felt that the gold standard by which facet joint blockade is judged is the appropriateness of the pain relief response based on duration of effect appropriate to the agent used for blockade and sustained relief by subsequent facet rhizotomy. This has been demonstrated in the cervical spine. In a study by Lord and colleagues, patients experiencing neck pain from whiplash, who responded to facet blocks, were randomized into active and sham groups for radiofrequency lesioning. The median duration of pain relief in the active group was significantly greater than that in the sham group. No patients who failed to respond to blockade were included in the study.
Rees is generally credited with performing the first facet rhizotomies. These were done percutaneously with a knife and reportedly resulted in immediate relief of symptoms in 998 of the 1000 patients who had facet pain in concert with the “intervertebral disc syndrome.” Shealy performed the procedure in North America but had an unusually high frequency of wound hematomas. This led to the adoption of a radiofrequency probe. Success rates as high as 90% were initially reported in previously nonoperated patients. That pain relief achieved by the interruption of afferent impulses of the facet joint has been suggested by the anecdotal reports of many authors who have noted immediate relief of pain in patients undergoing lumbar fusion.
Candidates for facet rhizotomy are those patients with back pain caused by facet dysfunction who have failed to respond to conservative therapy. The key diagnostic maneuver is thought to be the facet block. This involves percutaneous insertion of a needle into the joint, under fluoroscopic guidance, followed by joint injection with lidocaine (Xylocaine) combined with steroids or contrast agents. Patients in whom this procedure yields temporary relief may be candidates for facet rhizotomy.
In the series of Shealy, a satisfactory clinical result was noted in 79% of patients who had not had previous surgery. In patients who had undergone previous laminectomy, the success rate fell to 41%, and in those who had undergone previous fusion, success was only 27%. Of the 82 patients McCulloch followed from 6 to 20 months after facet rhizotomy, only 50% had satisfactory results. Interestingly, three patients in this group required repeat surgery. Schaerer reported on 71 patients who underwent lumbar facet rhizotomy. There were five distinct subgroups in his review: (1) lumbar facet disease without disc involvement (discography negative), (2) lumbar facet involvement with disc involvement (discography positive), (3) lumbar facet disease with discopathy and root signs, (4) facet signs with osteoarthritis, and (5) postlaminectomy pain. At a mean follow-up of 13.7 months, patients were evaluated using a pain profile. Thirty-five of 71 patients had satisfactory results. The highest percentage of success was in the author's first group—those who had a “pure” facet syndrome (seven of 15 patients). No attempt was made to determine statistically significant differences in outcome between these groups. Florez and colleagues reported a series of 30 patients, achieving satisfactory results in 76%. Twenty-six of the patients were followed for 3 to 9 months. The best results were noted in patients without previous operations and those with shorter duration of symptoms. Oudenhoven reported 377 patients with “pseudoradicular” pain in whom a lumbar facet syndrome was diagnosed by facet blocks. At a mean follow-up of 26 months, 83% were judged to be clinical successes. The author noted that a unilateral facet rhizotomy did not control pain and reported that 22% of patients who were judged to be clinical successes noted some return of symptoms at 18 to 24 months postoperatively. None of the authors reported any significant complications with the procedure. Lord and colleagues reported on 19 patients who underwent cervical percutaneous neurotomy for neck pain of at least 3 months' duration following motor vehicle accidents. They found that results varied by level. Of the 10 patients who underwent C2–C3 rhizotomy, three obtained greater than 6 months of pain relief and one was pain free at the 4-month follow-up; the remaining six had return of symptoms over 3 weeks. Of the 10 who underwent more caudal neurotomies, seven obtained “clinically useful” pain relief. The authors noted that C2–C3 results may have been compromised by technical failure, including the relatively large diameter of the nerves and their variable course. In a recent level IV study, Duff et al. reported that 63.64% of the patients in their series were pain free at 1 year. All patients had a mean of 1 year of pain relief.
With the recent interest in minimally invasive procedures, several studies have reported results of endoscopic rhizotomy of the lumbar spine. Jentzsch et al. in a small series (four patients) reported that 75% had significant pain relief at 2 months. The sole study criterion was “chronic low back pain.” Leon et al. described a “360” technique of radiofrequency ablation of the medial branch of the posterior primary ramus and the internal joint capsule. In this level IV study of 73 patients, a mean decrease in 10 cm visual analog scale data from 7.3 to 1.7 with good to excellent outcomes was noted in 91.7 of the patients at 12 months.
One may be tempted to recommend this procedure after diagnosis of facet syndrome with facet arthrography and blockade. The current literature, however, does not substantiate the rates of clinical success (83%) reported earlier. North and colleagues retrospectively reviewed prognostic factors for facet rhizotomy and found that only 42% of those selected for rhizotomy by response to facet blockade had pain relief at 2 years postprocedure. Seventeen percent of those who experienced relief from blockade, but did not undergo rhizotomy, were improved. As noted previously, one randomized prospective study of rhizotomy for cervical pain noted a longer duration of relief in the active lesion group. The reported complication rates are low, and the apparent risk to the patient is minimal. There remain no convincing studies in the literature, however, suggesting that pain relief from the procedure is permanent.
The technique for this procedure is well described. It is recommended that it be performed in the operating room or radiology department. Local anesthetic is adequate; the patient should be in the supine position for cervical rhizotomy or the prone position for thoracic and lumbar rhizotomy. Image intensification is required. Fourteen-gauge needles are placed unilaterally in the region of the appropriate facet(s) and nerves. A 5-mm, bare-tipped probe is then positioned in the area of the facet and the 14-gauge needle is partially withdrawn, leaving only the probe in the space between the superior facet and the transverse process immediately adjacent to the superior facet. The depth of the probe is controlled by lateral image intensification. A stimulation frequency of 100 Hz and from 0.1 to approximately 3 V is used to localize the tip away from the anterior ramus, as noted by the absence of paresthesia in the ipsilateral extremity. Once the depth is appropriate, stimulation adjacent to the posterior primary ramus reproduces a pain pattern familiar to the patient and the lesioning is then performed. A temperature-controlled lesion is produced by setting the controls at 25 V and 100 mA for approximately 60 seconds at 80°C. During the final 20 seconds, the amperage is slowly increased to the point where the milliamperage starts to diminish and voltage rises. This takes the temperature to approximately 90°C. After this, the probe is withdrawn, the wound dressed, and the patient mobilized. Alternatively, an endoscopic approach may be used as described earlier. Whether or not the so-called “360” technique is superior in the long run to the conventional deafferentation techniques is at this point unknown.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here