Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tracheal Resection for Locally Advanced Carcinoma of the Thyroid Gland.
Invasive thyroid cancer is defined as a disease that extends outside of the thyroid gland or outside the capsule of metastatic nodes to involve adjacent structures. Several decades ago, the problem of invasive disease was more prevalent, as patients tended to seek medical care later in the course of their illnesses—when symptoms brought them to the attention of physicians. In the contemporary era, the increase in the prevalence of thyroid cancer in general is largely, but not exclusively, due to detection of the disease at an earlier stage. This evolution has affected thyroid cancer care because clinicians who treat thyroid cancer often are lulled into complacency as to the complexity of the required surgery; they are not prepared to manage a more extensive disease that only becomes evident during the proposed surgical intervention that is not comprehensive enough for the appropriate management of the true invasive disease process. As such, clinicians also do not inform patients about the potential extent of the surgery required to achieve clear margins.
Invasion of the central compartment’s visceral and neurologic structures has been reported in a number of articles dating to the publication by Frazell et al. in 1958. The incidence of invasive thyroid cancer in a number of thyroid cancer series ranges from as low as 1% to as high as 23%. The incidence of invasive disease may be affected by referrals to a particular center, as well as the era covered in the given series. In addition, the incidence of invasive disease can be affected by whether the series includes only well-differentiated thyroid cancer or poorly differentiated and anaplastic varieties as well. The central compartment’s visceral structures that may be involved include primarily the larynx, trachea, and esophagus. The neurologic structures include the superior and recurrent laryngeal nerves. Caudal extension of disease or metastatic nodes may lead to vascular involvement of the great vessels and extension to the mediastinum.
This chapter explores the management of invasive thyroid cancer involving the larynx, trachea, and esophagus. In virtually every series on invasive thyroid disease, the recurrent laryngeal nerve (RLN) is the most commonly involved central compartment structure. The incidence of RLN involvement was reported by Breaux et al. to occur in 47% of patients in their series. The incidence varied in other series by Fujimoto (56%); McConahey (38%); McCaffrey (47%); Nishida (59%); and Nakao (61%). Several authors group laryngeal and tracheal involvement together; therefore the true incidence of laryngeal involvement can be gleaned from only a handful of series. Incidence ranges from 0% reported by Nakao et al. to as high as 34% in the series by Breaux et al. Tracheal invasion is far more common (37% to 60%) than laryngeal invasion, likely due to the proximity of the thyroid gland to the anterior and lateral tracheal walls. Esophageal invasion is also less frequent than tracheal invasion, with an incidence from 9% to 31%, with true transmural extension to involve esophageal mucosa on the lower end of that spectrum and outer muscular wall invasion on the higher end.
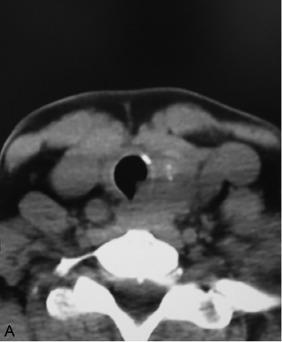
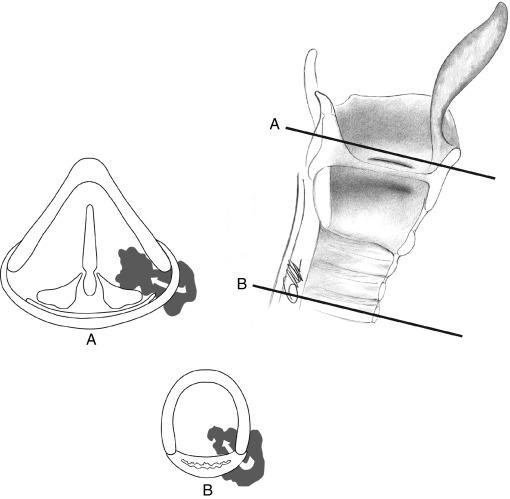
It is important to state at the outset that invasive thyroid cancer typically involves multiple structures within the central compartment, more often than it involves a single one. For example, in a given patient, disease may include the overlying strap muscles as well as the trachea and the esophagus ( Figure 37.1 ).
In this chapter, we discuss signs and symptoms, mechanism for invasion, diagnosis of invasive disease, and surgical management of invasion of the larynx, trachea, and esophagus. As noted previously, combined visceral invasion is the norm rather than the exception. The role of postoperative 131 I and external beam radiotherapy (EBRT) will be discussed in subsequent chapters (see Chapter 49 , External Beam Radiotherapy for Thyroid Malignancy).
As noted earlier, a patient with invasive thyroid cancer is often asymptomatic. A patient may take the unsuspecting surgeon by surprise when the thyroid gland or paratracheal lymph nodes are mobilized away from the laryngotracheal complex.
One can identify five types of patients who may be recognized preoperatively as being at increased risk of having invasive thyroid cancer:
The patient with suspicious or biopsy-proven disease and an abnormal physical examination (PE) finding, such as vocal cord dysfunction, subglottic or tracheal mass, or asymmetry of the pyriform sinuses due to submucosal tumor extension in that location.
The patient with suspicious or biopsy-proven disease and such symptoms as dysphagia, dyspnea, hemoptysis, or a change in voice.
The patient who has biopsy-proven systemic metastasis.
The patient with recurrent thyroid cancer after a prior therapy.
The patient with biopsy-proven disease and preoperative cross-sectional imaging that demonstrates invasion of the visceral structures or extranodal extension from a metastatic lymph node.
All of the aforementioned patients should undergo more detailed imaging of the neck and mediastinum to better define the extent of their primary tumors. Even when cross-sectional imaging fails to show intraluminal extension by thyroid cancer, a surgeon may find involvement of the cartilaginous structure during the operation. Initial findings include a palpable neck mass (98% to 100%); hoarseness (18% to 22%); dysphagia (25%); hemoptysis (11% to 25%); or dyspnea (5% to 33%). Patients with transmural tumor extension most likely experience symptomatic hemorrhaging or impending airway obstruction. From 20% to 70% of patients with invasive thyroid carcinoma may have vocal cord paralysis. However, Randolph et al. voiced a word of caution when they reported that only one third of patients with vocal cord paralysis had voice changes. Therefore the sensitivity of voice changes as a marker for vocal cord paralysis was surprisingly low at only 33%.
Physical findings that may suggest invasion include a fixed cervical mass, a mass overlying the thyroid cartilage, or frank adherence or invasion of cervical skin. Because of the low sensitivity of voice changes as a marker for invasion, all patients must undergo either indirect or fiberoptic laryngoscopy to assess for true vocal cord paralysis or paresis, blood, pooling of secretions, submucosal changes, or distinct intramural invasion into the larynx, trachea, or hypopharynx. Office-based tracheoscopy and esophagoscopy may be performed to document the extent of invasion, to allow better surgical planning, and to provide for a more comprehensive discussion with the patient ( Figure 37.2 ).
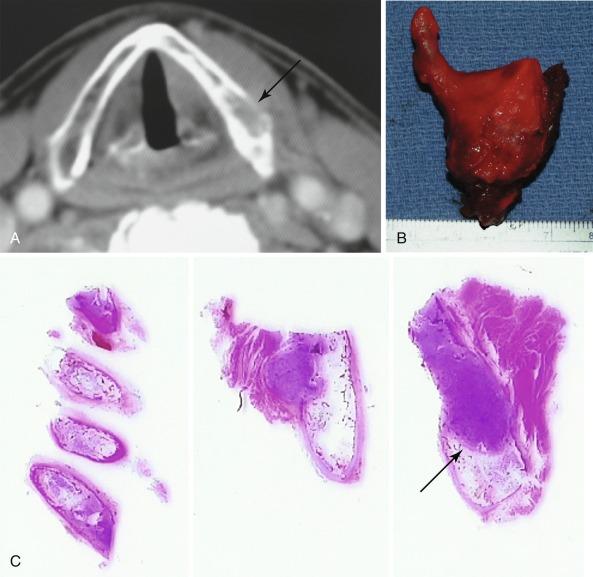
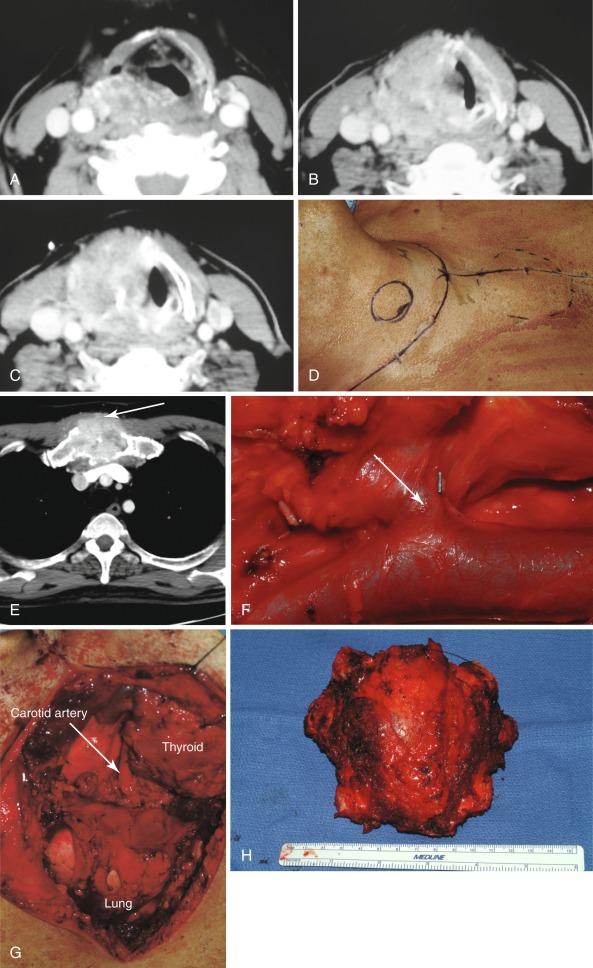
It is important to realize that not everything visualized intraluminally in a patient with thyroid cancer represents invasive disease. The authors have presented their experience with several cases mistaken for invasive thyroid disease. The disease entities included in that series were a benign, intratracheal thyroid rest in a patient with thyroid cancer; a benign tracheal stenosis adjacent to a benign thyroid nodule; a collision tumor of the larynx and thyroid, involving papillary thyroid cancer (PTC) and a primary squamous cell cancer of the larynx; a large schwannoma of the recurrent laryngeal nerve with severe tracheal compression; and chondrosarcoma of the trachea and the larynx. In addition to these noted exceptions, even rare primary thyroid histologies can exhibit invasive behavior ( Figure 37.3 ). The majority of patients with an intraluminal mass in the setting of biopsy-proven thyroid cancer have invasive disease; however, the surgeon should maintain a level of awareness of these other entities to ensure that the extent of the planned surgery is appropriate for the patient’s actual disease process.
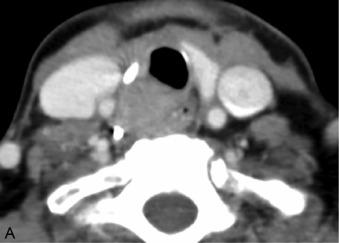
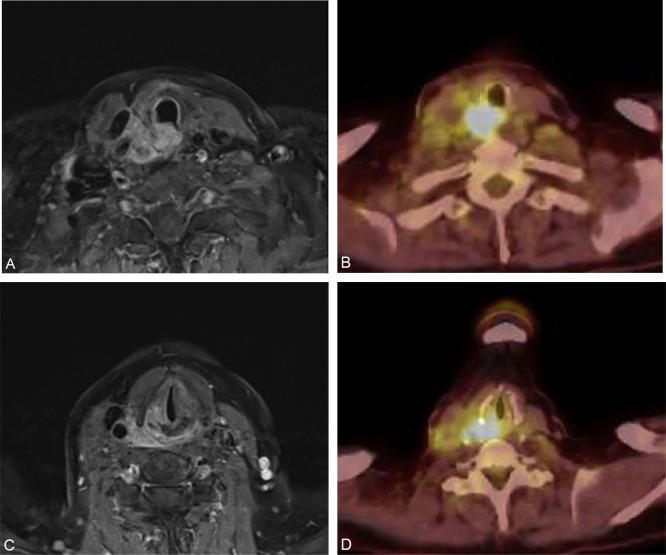
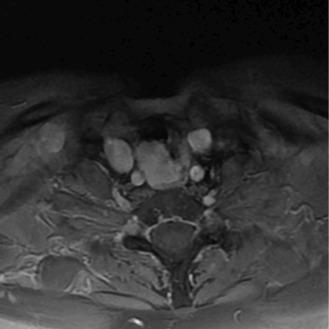
Imaging modalities have become an integral part of the diagnosis and staging of thyroid cancer. Ultrasonography (US) is widely accepted as the first-line imaging tool. In skilled hands, high-resolution ultrasound is very sensitive and specific in detecting suspicious nodules in the thyroid and metastatic lymph nodes in the lateral neck. However, its role in evaluating extrathyroidal extension involving the trachea, larynx, and esophagus is limited. Several reports vary significantly regarding the sensitivity of US in detecting tracheal invasion, but no data exist as to the utility of US in laryngeal involvement. It may be of help in detecting tracheal invasion in 40% to 90% of individuals; however, this is highly operator dependent, and cross-sectional imaging is generally more important. Computed tomography (CT) has a higher sensitivity in detecting central and mediastinal lymph node metastases, as well as evaluating the anatomic extent of extrathyroidal extension. The use of CT with iodine contrast may delay postoperative therapy with radioactive iodine, but lack of contrast CT may impede its overall sensitivity. The American Thyroid Association (ATA) recommends waiting 1 month after an iodine-contrasted CT to allow urinary levels of iodine to return to baseline before giving radioactive iodine. No evidence exists to suggest that waiting to give radioactive iodine for 1 month postoperatively negatively effects survival outcomes. Many patients with recurrent disease are in fact iodine nonavid. In some instances, magnetic resonance imaging (MRI) has proven useful in evaluating the scope of extrathyroidal extension to surrounding structures.
No data currently exist to suggest a role for fluorodeoxyglucose-positron emission tomography (FDG-PET) or FDG-PET/computed tomography (CT) imaging in the evaluation of visceral extension of thyroid cancer, but it may have a role in the evaluation of distant metastatic disease, especially in 131 I-negative patients. Patients with findings suspicious for thyroid cancer should undergo an initial US examination, including fine-needle aspiration biopsy to confirm the diagnosis. If these patients have further clinical or ultrasound findings suspicious for extrathyroidal or mediastinal extension, a CT or MRI should then be performed. Finally, studies of angiography with balloon occlusion may be required in patients with extensive extrathyroidal disease involving the great vessels to clarify further surgical planning.
Many parameters are important prognostic features in patients with well-differentiated thyroid cancer, including patient age, tumor size, histology, and distant metastases. (See Chapter 24 , Dynamic Risk Group Analysis and Staging for Differentiated Thyroid Cancer.) Among the various staging systems proposed for differentiated thyroid cancer, the presence of extrathyroidal extension (ETE) is one of the few that is universally accepted. In the eighth edition of the American Joint Committee on Cancer Staging Manual , extrathyroidal extension is divided between gross extension invading only strap muscles and more extensive invasion of the subcutaneous soft tissue; the larynx or trachea; esophagus; and RLN (T4). The incidence of ETE rises as the primary tumor increases in size. However, even micropapillary thyroid cancers, less than a centimeter in size, can extend outside the thyroid capsule in as much as 21% of cases. The presence of ETE has been associated with an increased incidence of both recurrence and death resulting from disease. Breaux and Guillamondegui reported on the institutional experience at the MD Anderson Cancer Center and noted an increased incidence of mortality from disease in invasive cancers greater than 4 cm in diameter. In addition, if more than four structures were involved by invasive disease, there were no survivors.
It is apparent that ETE is a product of both the biologic aggressiveness of the tumor and its location within the gland. Tumors that are subcapsular in location have a much greater likelihood of extending beyond the thyroid parenchyma. The issue of how to define ETE has come into question in a publication by Mete et al. The anatomy of the thyroid capsule is poorly understood, and these authors discuss thoroughly the contemporary view of the outer layer of the thyroid gland. The authors concluded that the thyroid gland does not have a true capsule but rather a discontinuous layer of fibroadipose tissue that constitutes a pseudocapsule. Also, they point out that the region of the isthmus is unique because of the direct continuity of the thyroid parenchyma with the subcutaneous fat; also, normal skeletal muscle fibers lay in close proximity to gland parenchyma in this area. As a result, the classification of a tumor as exhibiting ETE must be interpreted carefully. The mere presence of thyroid cancer in direct continuity with subcutaneous tissue or muscle, particularly for a tumor in the isthmus, may not constitute ETE. It is therefore evident that differences in incidence as well as the prognostic significance of ETE may be greatly affected by these ambiguous anatomic details. Marked ETE, leading to upstaging to pT4, is more readily identified and less controversial.
The presence of extranodal extension (ENE) in a lymph node affects the prognosis, and it is a cause of invasion of the RLN from paratracheal nodes involved by metastatic disease exhibiting this feature. Yamashita et al. reported the effect of ENE on prognosis, which leads to an increased risk of distant disease as well as the risk of dying from disease. Leboulleux et al. further identified the number of lymph nodes (LNs) with ENE as being an important predictor of recurrent cancer. In that series, the authors found that the presence of fewer than three such LNs corresponded to a 10-year recurrence rate of 2%, whereas more than three LNs with ENE led to a 10-year recurrence rate of 38%. Finally, Ito identified that both minimal ENE and extensive ENE were associated with a worse cause-specific survival rate than those patients without extranodal extension identified on pathology.
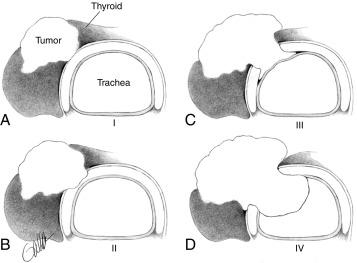
Further classification of invasive thyroid cancer involving the trachea was delineated by Shin et al., who divided the disease into four stages. Stage 1 tracheal invasion involves tumor abutment of the outer perichondrium, but without invasion through the outer perichondrium. Stage 2 invasion involves cartilage erosion without transmural extension. In stage 3 invasion, the tumor invades through the cartilage but not through the mucosa. Finally, stage 4 disease is both transcartilaginous and transmucosal ( Figure 37.4 ). In addition, the stage of invasion had prognostic significance. There was a clear distinction between those patients with stages 1, 2, and 3 disease in which none of the patients died of disease within the first 5 years after surgery, whereas 5 of 11 patients with stage 4 invasion succumbed during that time interval. Although it seems apparent that the biologic aggressiveness of thyroid cancer leading to the various stages reported by Shin with regard to the trachea should apply to the larynx or esophagus, there has been no such classification of the depth of invasion of these structures by thyroid cancer.
There are three avenues for invasive thyroid cancer to affect the larynx. The first and most common is invasion of the RLN directly by the primary tumor or by a metastatic paratracheal lymph node. The second is by direct invasion of the larynx from the primary tumor with extension through the cricoid, the thyroid ala, or the paraglottic space around the posterior aspect of the thyroid cartilage. The last route of invasion is through a metastasis to the cartilage, which happens infrequently ( Figure 37.5 ).
McCaffrey et al. studied cases of invasive thyroid cancer treated at the Mayo Clinic from 1940 to 1990 and identified four routes of invasion of the laryngotracheal complex. In the first route, the disease extended from the superior pole around the posterior border of the thyroid ala to involve the paraglottic space. The second route entailed invasion of the trachea by a metastatic lymph node. For the third route, the authors described direct invasion of the thyroid ala by disease in the superior pole. Finally, the fourth route spread through direct invasion of the cricoid or trachea from a primary tumor in the isthmus ( Figure 37.6 ). The whole organ serial section of a patient with invasive papillary thyroid cancer necessitating a total laryngectomy demonstrates most of these pathways for disease spread into the laryngotracheal complex ( Figure 37.7 ).
Dralle et al. classified their series of invasive thyroid cancer cases into six different varieties representing different sites of disease involvement. The site of involvement had implications for the extent of required laryngotracheal resection and reconstruction. As is typical of most cases of laryngeal invasion by thyroid cancer, the tracheal complex as well as the esophagus often become involved. Type 1 invasion involved a limited area of the lateral aspect of the cricoid cartilage and the first tracheal ring. The recurrent laryngeal nerve is typically also involved in type 1. Type 2 is similar to type 1 but is located more inferior in the trachea away from the larynx. The type 3 pattern included a larger portion of the laryngotracheal junction than Type 1 or type 2 more than 2 cm of longitudinal involvement or over a third of the circumference requiring resection. With regard to reconstruction, types 1 and 2 differed from type 3 primarily because type 1 and type 2 may be amenable to a patch repair with a sternocleidomastoid muscle flap, as opposed to type 3, which required a laryngotracheal resection and end-to-end repair. Type 4 is similar to type 3 with more than 2 cm of longitudinal involvement or over one third of circumferential involvement, but it is more inferior, only involving the trachea. Finally, type 5 invasion involves a much more significant portion of the laryngeal complex so that the opportunity for performing a partial laryngectomy with repair is not possible; a total laryngectomy is the only oncologically sound option. Type 6 invasion also requires a total laryngectomy, but it includes the esophagus or the hypopharynx.
An additional route of laryngotracheal as well as esophageal invasion not previously described in McCaffrey’s and Dralle’s series travels via the tracheoesophageal common party wall. Invasive thyroid malignancies near the tracheoesophageal groove or more superiorly near the cricothyroid articulation may spread along the thin connective tissue layer between the adventitia of the esophageal musculature posteriorly and the trachealis muscle anteriorly. Once access to the tracheoesophageal party wall is gained, the only anatomic barriers to intraluminal tumor spread is the thin smooth muscle of the trachealis and the relatively thicker muscular wall of the esophagus. Figure 37.8 demonstrates a case of common party wall invasion with intraluminal extension into the trachea and superior extension into the cricothyroid articulation.
This route of invasion may be even more important in the context of recurrent disease. The most challenging area of dissection during initial thyroidectomy is in the apex of the tracheoesophageal groove near the cricothyroid articulation because of the proximity of the RLN, which consistently enters the larynx in this area. Even primary tumors without significant extrathyroidal extension can be incompletely excised in this area during the initial resection in an effort to avoid significant dissection and compromising of the RLN. It is presumed that this is the likely etiology of recurrent disease in this region, which is at a high risk for invasion via the common party wall ( Figure 37.9 ).
As mentioned earlier, transmural mucosal involvement of the esophagus is rare, and the extent of involvement is usually limited to the muscular layer. The route of invasion typically involves direct spread from large or posteriorly based tumors or via the common party wall. Esophageal invasion is almost always accompanied by laryngotracheal complex and/or RLN involvement; it is almost never seen in isolation.
The overarching goal of surgical management of gross macroscopic invasive thyroid cancer involving the larynx, trachea, or esophagus is to prevent disease progression in the central compartment that would pose a threat to the patient’s airway and hypopharynx and esophagus. In addition, the surgeon should strive to alleviate existing disease-related symptoms because of involvement of these structures. This is best accomplished through resection with negative margins and reconstruction of the central visceral structures in a manner that achieves a stable airway and alimentary tract and restores the patient’s ability to speak.
Surgical approaches to invasive thyroid carcinoma range from limited procedures, such as shave resection, to total laryngopharyngectomy. The treating surgeon should be familiar with upper aerodigestive tract anatomy and the various surgical approaches available to achieve a cure while attempting to maintain function. The evaluation of the extent of disease entails a detailed PE with office-based or intraoperative esophagoscopy and bronchoscopy as well as appropriate imaging studies as previously described. Patients who are being considered for conservative laryngeal surgery should be evaluated carefully for underlying pulmonary disease because this may play a role in the decision-making process. In extreme cases, the extent of disease will require a multidisciplinary approach, including the assistance of vascular and thoracic surgical specialties.
Intraoperative frozen section pathology plays an important role in any surgical endeavor. In contrast to squamous cell carcinoma of the larynx, successful resection of well-differentiated thyroid carcinoma can be achieved with only a few millimeters of negative margins, and distant metastatic disease is not a contraindication for surgical management because patients with well-differentiated thyroid carcinoma may live many years with their underlying disease. However, it is important to consider the histology of the tumor because certain histologic subtypes, such as tall cell, Hürthle cell, and insular or hobnail variant, may behave more aggressively and respond not as well to nonsurgical modalities, thus requiring more extensive resection. The surgeon must remember that when thyroid cancer is behaving in a more aggressive manner, it may not be iodine avid; as a result, the complete surgical management of the disease process is very important for achieving the goals noted earlier. Achieving grossly negative margins is mandatory before reconstruction. However, frozen section pathology has its limitations when cartilage is involved. For example, elderly patients with ossified thyroid cartilage may not be able to have their cartilaginous margins cleared with frozen section pathology; they may require permanent section analysis. Patients must be informed that final pathology results may necessitate further surgery. As previously discussed, Shin et al. attempted to stage tracheal invasion as a guideline for the extent of surgery required. Controversy still remains as to the adequacy of shave resection with limited disease. However, multiple studies have shown that survival will be significantly improved by removal of macroscopic disease followed by adjuvant therapy.
When the depth and extent of laryngeal involvement are limited to the cartilage and overlying strap muscles, the surgeon may consider cartilage resection with preservation of the underlying soft tissue structures guided by principles similar to tracheal involvement. Usually, early disease involving the cartilage will be limited to one area, and cartilage resection will not impair function. Often, one of the greatest challenges facing the surgeon is determining the extent of the disease invasion. Preoperative cross-sectional imaging is often very helpful (see Figure 37.1 ). However, the larger problem occurs when the unsuspecting surgeon encounters cricoid or thyroid cartilage involvement without imaging available. In these situations, it may be hazardous to attempt a more limited resection. The mechanism of tumor invasion and extent of disease will dictate the feasibility of laryngeal preservation surgery. Basic principles of partial laryngeal surgery as well as standard techniques that have been well defined in the management of squamous cell cancer involving the larynx should be employed in the management of patients with invasive thyroid cancer. One functional RLN and at least one intact arytenoid with a functional cricoarytenoid complex must be preserved to allow adequate airway protection, a patent airway, and phonation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here