Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Feeding and swallowing problems are commonly encountered issues in pediatric otolaryngology. The incidence of feeding disorders has been estimated at 25% to 45%; the incidence of swallowing disorders is unknown but is increasing with improved life expectancy of premature babies. Oropharyngeal dysphagia has been estimated to affect up to 85% of children with underlying neurologic disorders. Dysphagia is the result of a problem during one or more of the phases of swallowing: the oral phase, the pharyngeal phase, or the esophageal phase. Of particular concern in children with dysphagia is the presence of aspiration, which can lead to pulmonary complications such as chronic cough or aspiration pneumonia. Pediatric dysphagia is multifactorial in nature, and these children benefit from being evaluated in a multidisciplinary manner. Services involved in the care and management of these children include Neurology, Pulmonology, Gastroenterology, and Otolaryngology.
An important part of the complete evaluation for children with dysphagia and suspected aspiration typically includes consultation with an Otolaryngologist. Laryngoscopic examination allows for assessment of any anatomic abnormalities that may contribute to dysphagia. Although the majority of cases of pediatric dysphagia are neurologic in nature, there are patients who have certain anatomic abnormalities that may predispose them to aspiration. Patients with posterior laryngeal cleft are a particular subset who may benefit from surgical intervention.
Historically, the incidence of laryngeal cleft has been estimated at approximately 1:10,000 to 1:20,000 newborns. In recent years, however, with increased awareness of milder forms of laryngeal cleft, including mild type 1 cleft such as low interarytenoid height, this entity is being diagnosed more frequently. The most commonly used classification system remains that described by Benjamin and Inglis in 1989. Type 1 clefts are limited to the interarytenoid region and have also been referred to historically as “occult clefts.” They are believed to be caused by issues that involve interarytenoid muscular development or lack of normal arytenoid cartilage development that may involve the cuneiform or corniculate cartilage. Type 2 clefts involve the upper portion of the cricoid cartilage, type 3 clefts extend through the entire height of the cricoid cartilage, and type 4 clefts extend into the thoracic trachea. Patients with more severe type 3 and 4 clefts typically present in the first few days of life with significant aspiration or recurrent apneic/hypoxic episodes, whereas patients with milder clefts typically have much milder symptoms, resulting in a delay in diagnosis.
Surgery is the mainstay of treatment for patients with laryngeal cleft. Historically, open approaches via thyrotomy, cricothyrotomy, tracheofissure, and lateral pharyngotomy have been described. With advances in endoscopic instrumentation over the past several decades, an endoscopic approach is generally favored when it is feasible, is widely used for type 1 and 2 clefts, and has even been described for certain type 3 and 4 clefts.
Injection augmentation of the interarytenoid region for aspiration in mild posterior laryngeal cleft was first described in 1995 and has been widely used for type 1 clefts since that time. The advantage of injection augmentation for milder clefts is that it can provide a significantly less invasive means of treatment for these patients, also provides clarification of the cleft contribution to the child’s dysphagia, and can help guide further management including a possible formal repair.
For children with severe and intractable aspiration despite maximal management of comorbid conditions, laryngotracheal separation provides a last-resort management option.
Dysphagia and aspiration are commonly encountered problems in pediatric otolaryngology, and a multidisciplinary approach should be employed in the evaluation and management of these patients.
Laryngeal cleft is a surgically correctable entity, and surgical management should be considered in symptomatic patients.
Surgical management of laryngeal clefts ranges from injection laryngoplasty in mild or uncertain cases, to endoscopic repair in types 1 to 3 and some type 4 clefts, to open repair for more extensive clefts or revision cases.
Injection laryngoplasty could be used to help diagnose a type 1 laryngeal cleft when injection is performed with a temporary substance.
Laryngotracheal separation may be considered as a last resort for children with intractable aspiration despite maximal management of any comorbid conditions.
Feeding history
What type of diet is the patient currently on?
Is there coughing and choking with feeds? What types of consistencies cause coughing and choking?
Have any dietary modifications been tried? Did this help?
Any difficulty breathing or noisy breathing with feeds?
Is the patient gaining weight adequately?
Any reflux symptoms? Frequent spit up/burps? Excessive vomiting? Nocturnal cough?
Respiratory history
Any cyanotic or apneic episodes?
History of pneumonia? Bronchiolitis?
Any history of chronic cough or recurrent croup?
Any stridor?
Neonatal history
History of prematurity?
Did the child require admission to the neonatal intensive care unit (NICU)?
Any need for respiratory support, including supplemental oxygen, positive pressure support, or intubation?
Past medical history
Cardiac or pulmonary disease?
Past surgical history
Intubation for any surgical procedures?
History of cardiac procedures?
Medications
Reflux medications?
General appearance
Any abnormal or syndromic features?
Opitz syndrome: Laryngeal malformations, pinna abnormalities, cleft lip and palate, hypertelorism, genitourinary abnormalities, other malformations of the ventral midline
Pallister-Hall syndrome: Laryngeal cleft, bifid epiglottis, genitourinary malformations, neurologic malformations, and syndactyly
CHARGE syndrome: Coloboma, heart defects, choanal atresia, growth and mental retardation, genitourinary malformations, and ear malformations
VACTERL association: Vertebral, anal, cardiac, tracheoesophageal, ear, renal, and limb malformations
Does the child appear malnourished/failure to thrive?
Head and neck examination
Any masses or pits on neck?
Any other midline anomalies such as cleft palate or submucous cleft palate?
Respiratory examination
Respiratory distress/stridor
Retractions/nasal alar flaring
Respiratory rate
Flexible laryngoscopy
Evaluate both choanae for patency.
Evaluate supraglottis for any significant reflux changes or laryngomalacia.
Examine for any evidence of deep interarytenoid notch or laryngeal cleft, although this is difficult to see on fiberoptic examination alone.
Fiberoptic endoscopic evaluation of swallowing
A flexible endoscope is advanced through the nose and the larynx is visualized while the patient is feeding.
Advantages: Allows for evaluation of anatomy and vocal cord mobility, presence of any premature spillage or presence of residue in the hypopharynx following swallow, and presence of supraglottic laryngeal penetration or laryngeal aspiration
Disadvantages: Some discomfort to patient, and some patients may not cooperate with swallowing. Unable to assess the pharyngeal phase of swallow due to white-out. Rarely, may cause laryngospasm or vasovagal reaction
Modified barium swallow study
Fluoroscopy is performed during feeding of foods mixed with barium contrast material.
Advantages: No significant discomfort, tolerated well by most children. Allows evaluation of pharyngeal phase of swallowing
Disadvantages: Requires exposure to radiation. Unable to directly visualize laryngeal anatomy
Posterior pattern of aspiration is suggestive of laryngeal cleft.
Chest radiograph
For evaluation of aspiration pneumonia when suspected
Diagnostic direct laryngoscopy/bronchoscopy
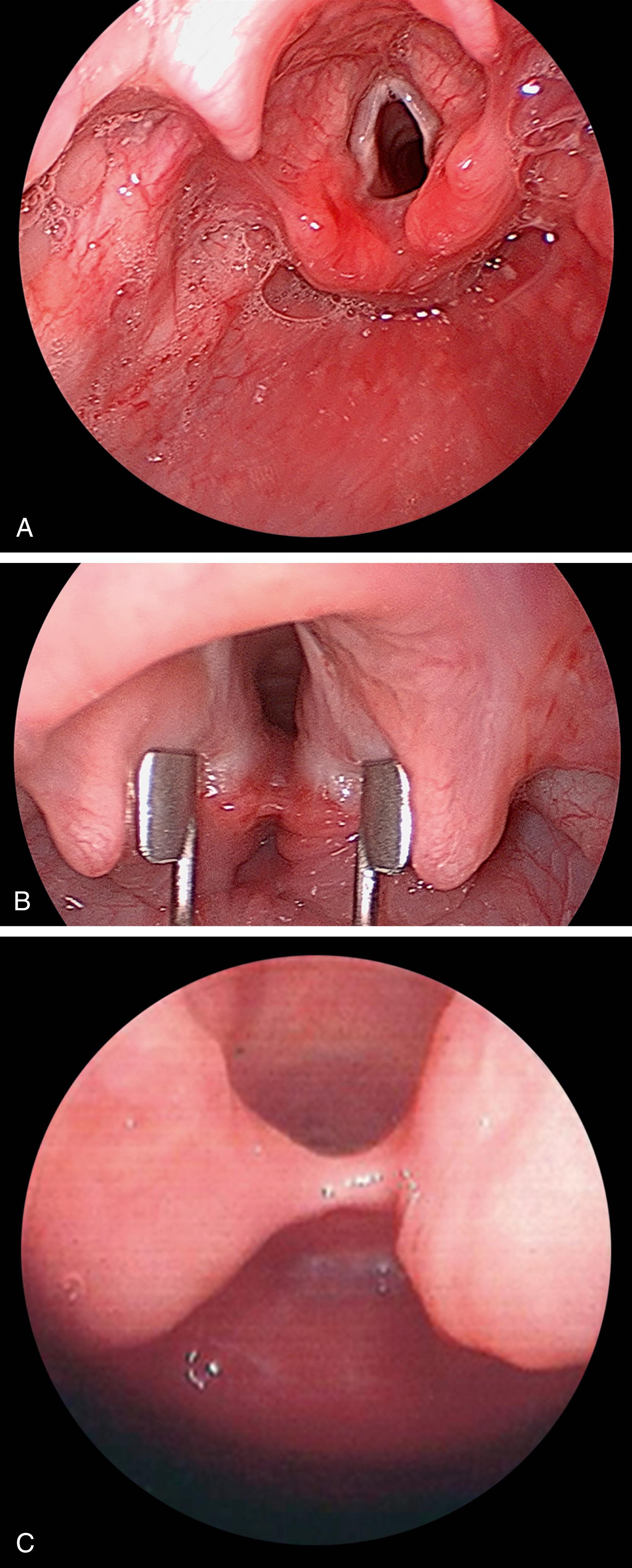
Palpate and visualize interarytenoid area ( Fig. 195.1 ) for evidence of type 1, type 2, and type 3 laryngeal clefts on direct laryngoscopy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here