Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Superior vena cava (SVC) syndrome is usually caused by a neoplastic process, predominantly primary lung carcinoma, with a disproportionate number of patients having small cell histology; non-Hodgkin lymphoma and metastatic tumors are the next most common.
SVC syndrome can be iatrogenic; it is increasingly seen as a complication of a central venous catheter, pacemaker leads, or cardiac surgery.
The junction of the brachiocephalic veins forms the thin-walled, low-pressure SVC, which is subjected to obstruction from a variety of mediastinal components, or an intravascular process.
External compression often precedes direct tumor invasion or thrombus formation.
The SVC has an extensive collateral network.
Usual symptoms are head fullness, dyspnea, cough, and chest pain, typically with insidious onset over weeks.
More severe symptoms are infrequent, and life-threatening neurologic symptoms are rare.
Diagnosis is based on clinical findings such as dilated chest veins and facial edema.
A chest radiograph typically shows mediastinal widening; a mass is often seen in the region of the SVC.
Contrast-enhanced computed tomography scanning identifies the mass and collateral flow and is the most helpful study to guide treatment.
Venography with small dose of contrast material can be safely accomplished to define the exact location of caval obstruction and routes of collateral flow.
Treatment of an identified mass before histologic diagnosis is rarely justified unless prior diagnosis is established.
Methods used to define histology are sputum cytology, thoracentesis, endobronchial ultrasound with and without bronchoscopy, lymph node biopsy, percutaneous biopsy, and video-assisted mediastinoscopy or thoracotomy; these techniques are considered quite safe.
Radiation therapy with or without chemotherapy is a preferred treatment in most malignant causes of SVC obstruction.
Chemotherapy would be the initial treatment of choice if a definitive diagnosis of chemotherapy-sensitive malignancies such as lymphoma, small cell lung cancer, or germ cell tumor has been made.
The radiation therapy fractionation schedule depends on tumor histology, stage, prognosis, the patient's general condition, and whether the obstruction is acute or subacute.
Percutaneously placed, self-expanding intravascular stents provide an option or adjunct to other procedures in the palliative treatment of patients (usually with malignant disease).
Angioplasty alone or in combination of self-expanding intravascular stents, and bypass surgery, is used for treatment of benign SVC obstruction.
Obstruction of the superior vena cava (SVC) may occur as an acute or subacute process producing a syndrome with characteristic features, including facial edema and plethora, dilation of chest wall and neck veins, mild to moderate respiratory difficulty, and, less commonly, conjunctival edema, central nervous system complaints such as headache, visual disturbances and signs of altered states of consciousness. The first recorded description of SVC obstruction occurred in 1757 when William Hunter described the entity in a patient with a syphilitic aortic aneurysm. For nearly two centuries thereafter, nonmalignant processes such as syphilitic aortitis and chronic mediastinitis due to tuberculosis were the predominant etiologies of SVC obstruction. However, in the postantibiotic era, cancer became the leading cause of SVC obstruction. In recent years, the percentage of SVC obstruction cases caused by nonmalignant processes has again risen, largely driven by the increased number of intravascular devices and associated thrombi. Although SVC obstruction was once considered a medical emergency, it is now well established that patients with SVC obstruction rarely experience immediate, life-threatening complications. Consequently, in cases in which a diagnosis is not known, it is appropriate to first proceed with a diagnostic test or biopsy to establish the underlying etiology because optimal management is dependent on it.
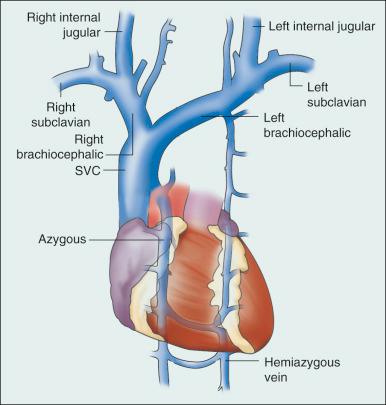
The SVC is formed by the junction of the brachiocephalic veins, which in turn are formed by the union of the internal jugular and subclavian veins. Thus, the SVC represents the major drainage system of venous blood from the head, neck, arms, and upper thorax. The right and left brachiocephalic veins join at about the level of the sternal angle to form the SVC. The SVC descends on the right side of the ascending aorta and empties into the right atrium, with its distal 2 cm lying within the pericardial sac ( Fig. 53.1 ).
Because of its mediastinal location and surrounding rigid structures, including the sternum, trachea, pulmonary artery, right mainstem bronchus, and numerous lymph nodes, the SVC is particularly vulnerable to obstruction. Despite being a relatively large vessel, its thin vascular walls and low intravascular pressure contribute to the ease with which it can be obstructed. SVC obstruction can be caused by external compression due to tumor or by lymph nodes enlarged by inflammation or metastases ( Fig. 53.2 ). SVC obstruction also can be caused by direct tumor invasion or by an intraluminal thrombus. Secondary thrombus is reported to occur in up to 50% of cases and may contribute to the lack of response to appropriate therapeutic maneuvers.
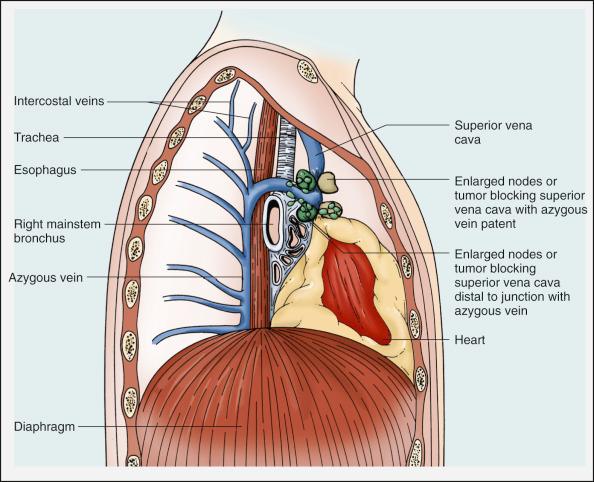
The azygous vein represents an important collateral system of the SVC and is formed by the junction of the right subcostal and right ascending lumbar veins. Additional routes of collateral flow include the mammary, vertebral, lateral thoracic, paraspinous, and esophageal vessels. The azygous vein ascends through the posterior and superior mediastinum, arches over the hilum of the right lung, and ends in the SVC. Fortunately, extensive anastomoses are formed between the SVC, azygous, and vertebral systems, providing multiple routes of collateral blood flow. Therefore, an obstruction of the SVC above the orifice of the azygous vein is better tolerated than is blockage below this level because blood can be diverted through chest-wall veins into the thoracic and iliac veins and enter the heart by way of the inferior vena cava (IVC) and azygous systems. Blood from the head and neck also can return to the heart via the vertebral plexus. If the SVC is obstructed between the azygous vein and the heart, the only route of blood return is via the IVC.
In the latter part of the 20th century, cancer was by far the leading cause of SVC obstruction accounting for approximately 90% of cases, with bronchogenic carcinoma and non-Hodgkin lymphoma (NHL) accounting for up to 85% of cases of malignancy-associated SVC obstruction. The two most frequent lung cancer histologic types associated with SVC obstruction are small cell (SCLC) and squamous cell carcinoma. Although lung cancer is the leading cause of SVC obstruction, the incidence of this syndrome in patients with lung cancer is relatively low overall (2% to 4%). SVC obstruction occurs more commonly in patients with SCLC (≈10% of patients) than non–small cell lung cancer (NSCLC) (≈2%). However, the higher incidence of NSCLC makes it the most common etiology of malignancy-associated SVC obstruction, accounting for 50% of such cases, with SCLC accounting for 25% cases. SVC obstruction may be the initial presentation of a previously undiagnosed malignancy in 60% of cases.
NHL is the second most common cause of SVC obstruction. In one series of 915 patients with NHL, 36 (3.9%) presented with SVC obstruction. Among subtypes of NHL, the incidence of SVC obstruction was highest in patients with lymphoblastic lymphoma (21%) and diffuse large cell lymphoma (7%). Primary mediastinal lymphoma is another aggressive NHL characterized by the development of a mediastinal mass, and in one report, 57% had clinical SVC obstruction and 80% had radiologic evidence of SVC compromise at presentation. More rarely, thymic neoplasms and primary mediastinal germ cell tumors can cause SVC obstruction. Metastatic cancers account for approximately 5% to 10% of SVC obstructions. In approximate order of frequency, the most common primary tumor sites are breast cancer, germ cell malignancies, and gastrointestinal cancers. Virtually any cancer capable of metastasizing to the mediastinum can result in SVC obstruction.
Nonmalignant causes of SVC obstruction now account for approximately one-third of cases. An increasingly common benign cause of SVC obstruction is central venous catheter–induced thrombosis, which may occur with cardiac pacemakers, tunneled dialysis catheters, LaVeen shunts, hyperalimentation lines, and Swan-Ganz catheters, as well as those used for chemotherapy administration. SVC obstruction seems to be more common when the tip of the catheter is placed in the upper part of the SVC. Although it has been the subject of many randomized trials, no convincing evidence supports the routine use of thromboprophylaxis in patients with central venous catheters, as demonstrated by a systemic review and meta-analysis reviewing outcomes with heparin or warfarin; the role for newer anticoagulants is less well defined. Additional rare benign causes of SVC obstruction include chronic mediastinitis as a result of histoplasmosis, retrosternal goiters, Nocardia infection, postradiation local vascular fibrosis, and congestive heart failure.
In children, SVC obstruction is most frequently related to iatrogenic causes resulting from cardiovascular surgery for congenital heart disease or ventriculoatrial shunts for hydrocephalus. The most common malignant causes of SVC obstruction in children are NHL, acute lymphoblastic leukemia, Hodgkin disease, neuroblastomas, and yolk sac tumors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here