Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Both the glenoid labrum and the long head of the biceps play a significant role in normal shoulder function. Lesions of either structure can cause significant shoulder pathology, pain, and dysfunction. Problems with the biceps and labrum are commonly seen in overhead athletes, specifically pitchers. Significant controversy exists regarding diagnosis and appropriate management of lesions of the superior labrum–biceps complex. Treatment can vary from simple rest to rehabilitation and finally surgical intervention. This chapter discusses the surgical management of complex lesions of the superior labrum–long head of the biceps complex.
Lesions of the labrum can be either debrided or repaired, depending on the tear pattern, patient age, and presence or absence of concomitant injuries. The long head of the biceps tendon can undergo tenotomy or tenodesis, or in the case of a superior labrum anterior posterior (SLAP) lesion, it can be repaired down with the biceps/labral anchor.
Onset: Did the pain begin traumatically, or was the onset insidious over a long period of time? Patients with biceps/labral pathology will often describe an insidious onset of pain or an acute traction injury to the shoulder. The overhead athlete may notice an issue with velocity or control (sometimes referred to as “dead arm” syndrome), or a swimmer may notice slower lap times.
Timing: When does the shoulder bother the patient? Is it with overhead activities (e.g., lifting)? Overhead athletes with biceps/labral pathology will often complain of pain during the late cocking/early acceleration phases of the pitch cycle. These overhead athletes may also complain of pain during the deceleration phase of throwing as the biceps acts to decelerate the arm after ball release. Clicking and/or popping may or may not be present.
What is the main complaint? Patients with biceps/labral pathology will often have a primary complaint of pain. Pain associated with the long head of the biceps commonly occurs over the anterior aspect of the shoulder, often with extension of symptoms into the biceps muscle belly. Pain from superior labral pathology more commonly occurs in the posterior-superior aspect of the shoulder.
Prior treatments/surgeries: One should always inquire about prior treatments or previous surgeries that the patient may have undergone, either for the biceps/labral complex or for other shoulder issues.
Concomitant injuries: Injuries to the biceps labral complex can often occur with other shoulder injuries, including rotator cuff tears, so a thorough history regarding the shoulder, elbow, hand, and wrist should be obtained as well.
Patient age: Patients over 40 years old can have normal aging and degenerative changes in their shoulder that may mimic superior labral tears.
Inspection: Modesty should be maintained, but the patient should be gowned such that the entire shoulder girdle, arm, and scapula are visible. When viewing the patient from behind, the examiner should look for any shoulder asymmetry, muscle wasting, or bruising. Selective muscle wasting of the infraspinatus could indicate a spinoglenoid notch cyst secondary to a superior labral tear ( Fig. 42.1 ).

Palpation: The examiner should palpate the acromioclavicular joint and biceps groove to assess for tenderness to palpation. The biceps can be palpated by gripping the shoulder from behind with the arm in neutral to slight external rotation. In this position, the bicipital groove is palpable, and direct tenderness can be elicited ( Fig. 42.2 ).

Range-of-motion (ROM) testing, both active and passive, should be performed in all planes. The examiner should focus on side-to-side differences. Deficits in glenohumeral internal rotation combined with total ROM loss with the arm at 90 degrees of abduction can predispose overhead athletes to shoulder and elbow injuries. Patients with biceps/labral complex issues often have a normal ROM. However, these patients often complain of pain when the shoulder is placed in positions of internal impingement (external rotation of the shoulder with the arm abducted) ( Fig. 42.3 ).

Each muscle of the rotator cuff should be tested in isolation. Patients with biceps/labral complex pathology often do not have significant rotator cuff weakness, with the exception of infraspinatus weakness in a long-standing spinoglenoid notch cyst.
Biceps-specific tests: The Speed and Yergason tests can sometimes be positive in patients with SLAP tears or long head of the biceps pathology. The Speed test is performed with the shoulder in 90 degrees of forward elevation, elbow extended, and arm fully supinated. A downward force is then placed on the forearm with resistance given by the patient. A positive test reproduces pain. The Yergason test is performed with the forearm pronated and the elbow flexed to 90 degrees. The patient actively supinates the wrist while the examiner resists, with pain into the biceps region defined as a positive test.
Instability tests including the anterior apprehension test as well as the relocation test should be performed to rule out shoulder instability. However, results of these are typically normal in patients with SLAP tears.
Many tests have been described to diagnose superior labral tears. These include the O’Brien, crank, anterior slide, dynamic labral shear, and pain provocation tests, among others. Unfortunately, the sensitivity and specificity of these tests has been shown to be quite low, with the sensitivity and specificity of many tests being below 70%. The O’Brien or active compression test is one of the most commonly used physical exam maneuvers used to diagnose a SLAP tear. This test is performed with the shoulder in 90 degrees of forward elevation and 10–15 degrees of adduction. A downward force is placed on the wrist with the forearm in full pronation with thumb pointing down, followed by a downward force with the forearm in full supination and the thumb pointing up. Pain with the thumb pointing down that is decreased when the thumb is pointing up indicates a positive test result ( Fig. 42.4 ).

The dynamic labral shear test (O’Driscoll test) is performed with the patient’s elbow flexed to 90 degrees and the arm at the side. The arm is abducted to 90 degrees and externally rotated to 90 degrees. The arm is then abducted from 90 to 120 degrees. Pain or a click, most commonly in the posterior-superior shoulder, during this movement indicates a positive test result.
A complete shoulder series of radiographs, including anteroposterior, scapular-Y, and axillary views, should be obtained in patients with shoulder complaints. These images are often normal in patients with SLAP tears, but they are useful to rule out other sources of shoulder pain ( Fig. 42.5 ).

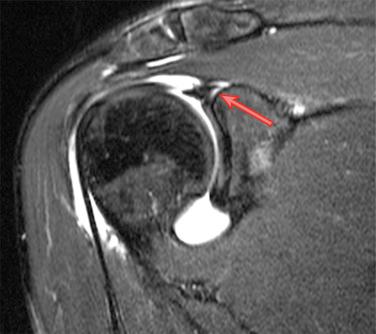
The preferred imaging modality in patients with suspected SLAP tears is magnetic resonance imaging (MRI) ( Fig. 42.6 ).
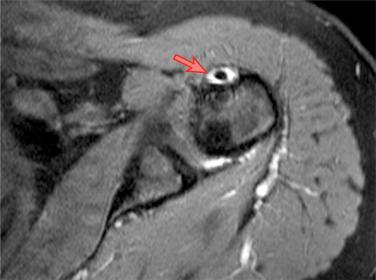
Unfortunately, MRI has a tendency to overdiagnose SLAP tears, with studies quoting the positive predictive value as low as 24% in patients who had an MRI followed by shoulder arthroscopy.
It does appear that magnetic resonance arthrography (MRA) improves the accuracy of diagnosing SLAP tears compared with MRI. However, use of MRA in overhead athletes is often indicated to assess for associated problems such as undersurface rotator cuff tears. The addition of an abduction and external rotation series may be helpful to assess for signs of internal impingement in a provocative position.
Typical MRI findings of SLAP tears include increased signal within the superior labrum and contrast extension under the superior labrum/biceps anchor. A sublabral cyst is also indicative of a superior labral tear (extension into the spinoglenoid notch can compress the suprascapular nerve) ( Fig. 42.7 ).
Computed tomographic arthrography can be performed in patients who cannot undergo an MRI, although MRA is the preferred imaging modality.
Despite advances in imaging studies, the gold standard for diagnosing a superior labral tear is arthroscopic evaluation.
Nonoperative treatment: Because results of SLAP repairs are not reliable, avoiding surgery, especially in the overhead athlete, should be attempted before surgery is considered.
Physical therapy should focus on alleviating posterior capsular tightness (sleeper stretch) and any glenohumeral internal rotation deficit, strengthening the rotator cuff, and correcting any existing scapular dyskinesia. Restoration of normal core strength is also imperative to allow a stable base for throwing.
Following appropriate clinical examination, typically 12 weeks of nonoperative care, including avoidance of throwing and physical therapy, to correct any of the above-noted abnormalities is recommended prior to surgical intervention.
There is no current evidence to suggest a positive role for platelet-rich plasma in the treatment of SLAP tears.
Operative intervention is recommended in the symptomatic patient in whom nonoperative treatment has failed. Principles of surgical management include diagnostic arthroscopy, identification of pathology, debridement or repair of the labral lesion, identification and treatment of alternative pathology such as partial-thickness rotator cuff tear, and evaluation of long head of the biceps with consideration for tenotomy or tenodesis.
Early operative intervention may be warranted in patients with spinoglenoid notch cysts causing neurologic compromise.
Rotator interval: anterosuperior triangular space of the rotator cuff between the subscapularis and supraspinatus tendons. The space contains the long head of the biceps tendon, the coracohumeral ligament, the superior glenohumeral ligament, and the glenohumeral capsule ( Fig. 42.8 ).

Spinoglenoid notch: portion of the scapula between the scapular spine and scapular body bound by the transverse scapular ligament through which the suprascapular nerve passes before it innervates the infraspinatus muscle.
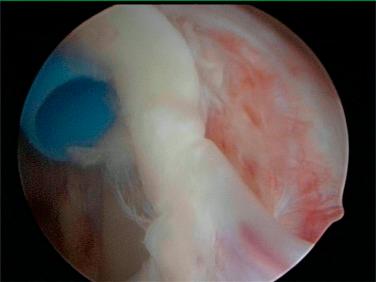
Buford complex: labral variant with an absent superior labrum from 1 to 3 o’clock and a “cordlike” middle glenohumeral ligament that originates from the superior labrum at the base of the biceps tendon and inserts on the humerus. This should not be confused with a labral tear ( Fig. 42.9 ; Video 42.1 ).
Sublabral foramen: an anterosuperior labral variant in which the labrum is separated from the glenoid. This is a normal variant and does not indicate a labral tear.
The long head of the biceps tendon has been shown to have increased activity in shoulders with increased anterior instability, indicating that the biceps may act as a secondary glenohumeral stabilizer.
The glenoid labrum is composed of fibrocartilaginous tissue, and the superior labrum serves as the anchor for the biceps tendon, the weak point involved in the SLAP lesion.
The labrum receives its blood supply from the suprascapular, circumflex scapular, and posterior humeral circumflex arteries. The anterior-superior labrum receives the least blood flow. No blood supply to the labrum comes from arteries via the glenoid bone. The vascular penetration of the arteries into the labrum is limited to the peripheral attachment of the joint capsule to the labrum.
Neurologic structures that lie near the glenohumeral joint include the suprascapular nerve (motor to supraspinatus and infraspinatus), axillary nerve (motor to deltoid and teres minor), and the musculocutaneous nerve (motor to biceps, coracobrachialis, and medial brachialis). The suprascapular nerve is found within 1 cm of the glenoid rim. It travels through the quadrangular space before it branches into anterior, posterior, and articular branches. The axillary nerve runs near the inferior capsule, commonly anterior to the subscapularis along the inferior border. The musculocutaneous nerve pierces the strap muscles approximately 3–8 cm distal to the tip of the coracoid.
A consistent history (pain in the late cocking/early acceleration phase of throwing) or single-event trauma of traction injury or fall onto outstretched hand, physical examination (positive O’Brien test), MRI findings (labral damage), and arthroscopic evidence of a SLAP tear with no alternative explanation for the patient’s complaints are an indication for surgical intervention.
Persistent pain despite proper nonoperative treatment with rest; therapy; and, in overhead athletes, a graduated throwing program.
One important aspect of determining the type of surgery to perform is the type of SLAP tear.
The historical classification system for SLAP tears was that of Snyder, in which four types were described. Recent studies have expanded the original classification to 10 subtypes. However, interobserver reliability in classifying SLAP tears is suboptimal. The four classic types of SLAP tears are as follows:
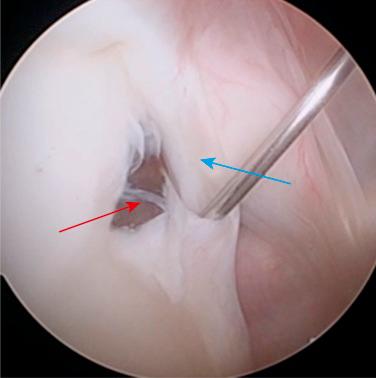
Type I: intact superior labral and biceps anchor attachments with superior labral fraying and minimal degeneration; this can be treated with a gentle debridement.
Type II: detachment of the superior labrum and biceps from the glenoid; this is the most common and clinically relevant type of SLAP tear and is commonly treated with repair or biceps tenodesis.
Type III: intact biceps anchor with a bucket handle tear of the labrum; this is commonly treated with debridement ( Fig. 42.10 ).

Type IV: extension of the bucket-handle labral tear into the biceps tendon causing a split biceps tendon. Treatment depends on severity of damage to the biceps tendon (the more severe the damage to the biceps and labrum is, the more often a biceps tenodesis will be performed over a SLAP repair) ( Fig. 42.11 ).
The more recently described SLAP tears are as follows:
Type V: Bankart lesion combined with a SLAP tear
Type VI: SLAP tear and an unstable labral flap
Type VII: SLAP tear that extends to the origin of the middle glenohumeral ligament
However, choosing between a labral repair and biceps tenodesis is a decision that must be made between the physician and patient, and it is one that should be based on arthroscopic findings, activity level, and patient age.
The following patient factors should drive the surgeon toward a biceps tenodesis over a SLAP repair: age >35–40 years, significant biceps pathology (groove pain, diffuse anterior irritation on arthroscopic examination), degenerative changes to the labrum, rotator cuff pathology, and glenohumeral arthritis.
SLAP repairs should be considered in those patients with a traumatic history, positive provocative exam maneuvers, and positive MRI findings indicating a SLAP tear in the absence of significant alternative pathology.
The authors prefer an open subpectoral biceps tenodesis using an all-suture anchor. A tenodesis screw can also be used with good, reliable results.
SLAP repairs can be performed with the patient in the lateral decubitus or beach chair position ( Fig. 42.12 ).

The authors prefer a lateral decubitus position ( Fig. 42.13 ).

General anesthesia with or without an interscalene block, or with an interscalene block with conscious sedation, can be used.
Prior to prepping and draping, the shoulder is taken through an ROM exam, and the stability of the glenohumeral joint is assessed.
The shoulder is then sterilely prepped and draped.
Proper positioning is critical because poor positioning will lead to poor visualization and will greatly increase the difficulty of the case.
All bony prominences should be well padded with placement of an axillary roll.
Check all equipment prior to beginning the case (shaver, burr, implants, etc).
Avoid excessive traction on the arm.
Dynamic examination at the start of the case with the arm out of traction allows for evaluation of internal impingement or peel-back findings.
Percutaneous portals from the lateral edge of the acromion allow appropriate anchor placement in the superior and posterior-superior glenoid rim.
At the completion of the arthroscopic portion of the case, if biceps tenodesis is indicated, the bean bag can be partially deflated, allowing the patient to be rolled back to a partial supine position with the arm outstretched on a Mayo stand to allow access to subpectoral tenodesis incision site.
Insufficient traction
Ensure that the head is properly secured to avoid problems during the case.
Rotate the bed to allow surgeon to stand at the head of the table with easy access to front and back of shoulder.
The surgeon must work with the anesthesia team to ensure that hypotensive anesthesia is maintained to facilitate visualization.
Make sure there is sufficient room to introduce the arthroscope and have all degrees of freedom posteriorly to avoid hitting the bed during the procedure.
Appropriate portal placement is critical to facilitate repair.
Procedures should be performed expeditiously to avoid extensive shoulder swelling.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here