Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A list of vesiculobullous diseases appears in section 1.147. Some subepidermal diseases can appear to be intraepidermal when they have re-epithelialized. Usually, the blister will have a smooth base in that case. The following diseases may sometimes produce subepidermal blisters, but are not discussed in this chapter.
Erythema multiforme (3.2)
Porphyria (8.1)
Lichen planus (2.11)
Amyloidosis (8.4)
Mastocytosis (24.17)
Lupus erythematosus (17.6)
Lichen sclerosus (9.5)
Graft-versus-host disease (17.3)
(see Fig. 6.1A–D )
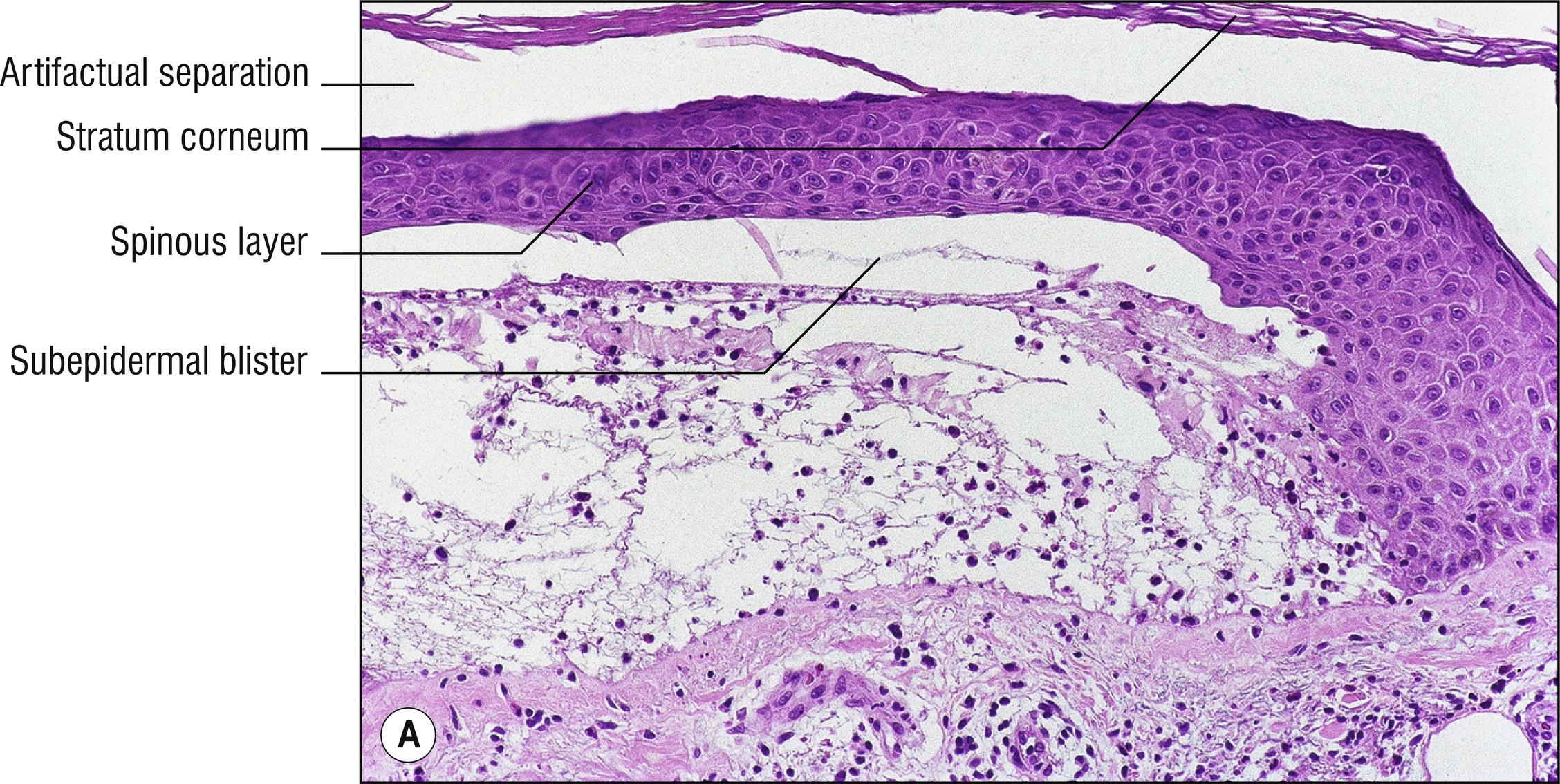
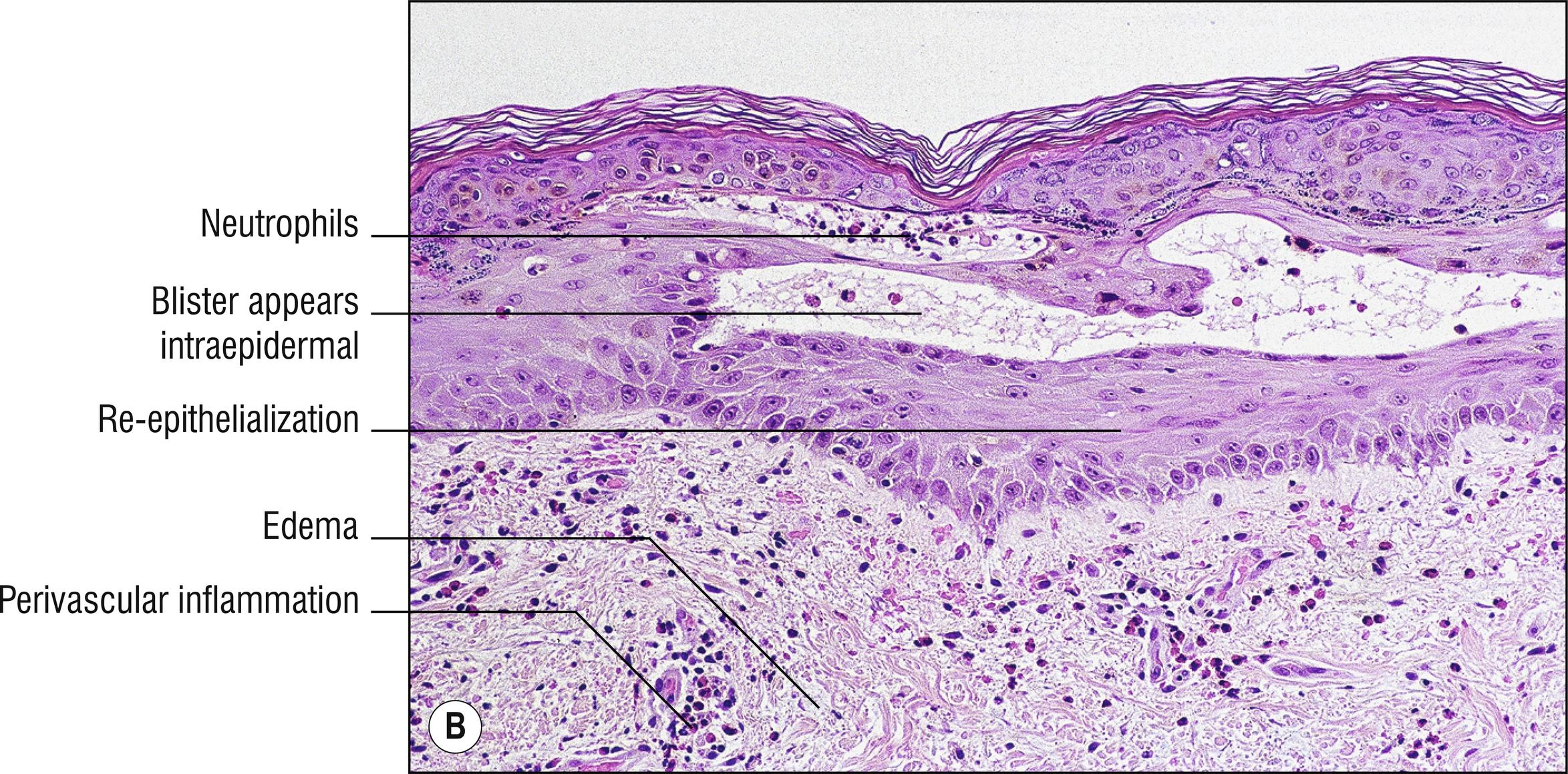

Somewhat common, autoimmune disorder mostly of the elderly , with pruritic (1.114) urticarial plaques leading to tense bullae . Antibodies are directed most commonly toward BP2 antigen (180 kD, type XVII collagen, most commonly the NC16a portion), commercially available as ELISA test from serum. BP1 antigen (230 kD) is less commonly the target, so sometimes it is recommended to screen patients first for BP2. Mouth and mucous membranes uncommonly involved, compared with pemphigus vulgaris.
Eosinophilic spongiosis (1.36) sometimes, especially in early non-blistered red plaques
Subepidermal blister
Viable roof over blister, necrotic only in old blisters
Perivascular lymphocytes (1.109) and eosinophils (eosinophils sometimes numerous); sometimes very sparse infiltrate (cell-poor pemphigoid). If numerous eosinophils are found in the dermis in an elderly patient, even without blistering, the diagnosis of pemphigoid is highly likely
Superficial dermal edema (1.30)
Microabscesses of neutrophils and eosinophils in the dermal papillae sometimes, as in dermatitis herpetiformis (6.5)
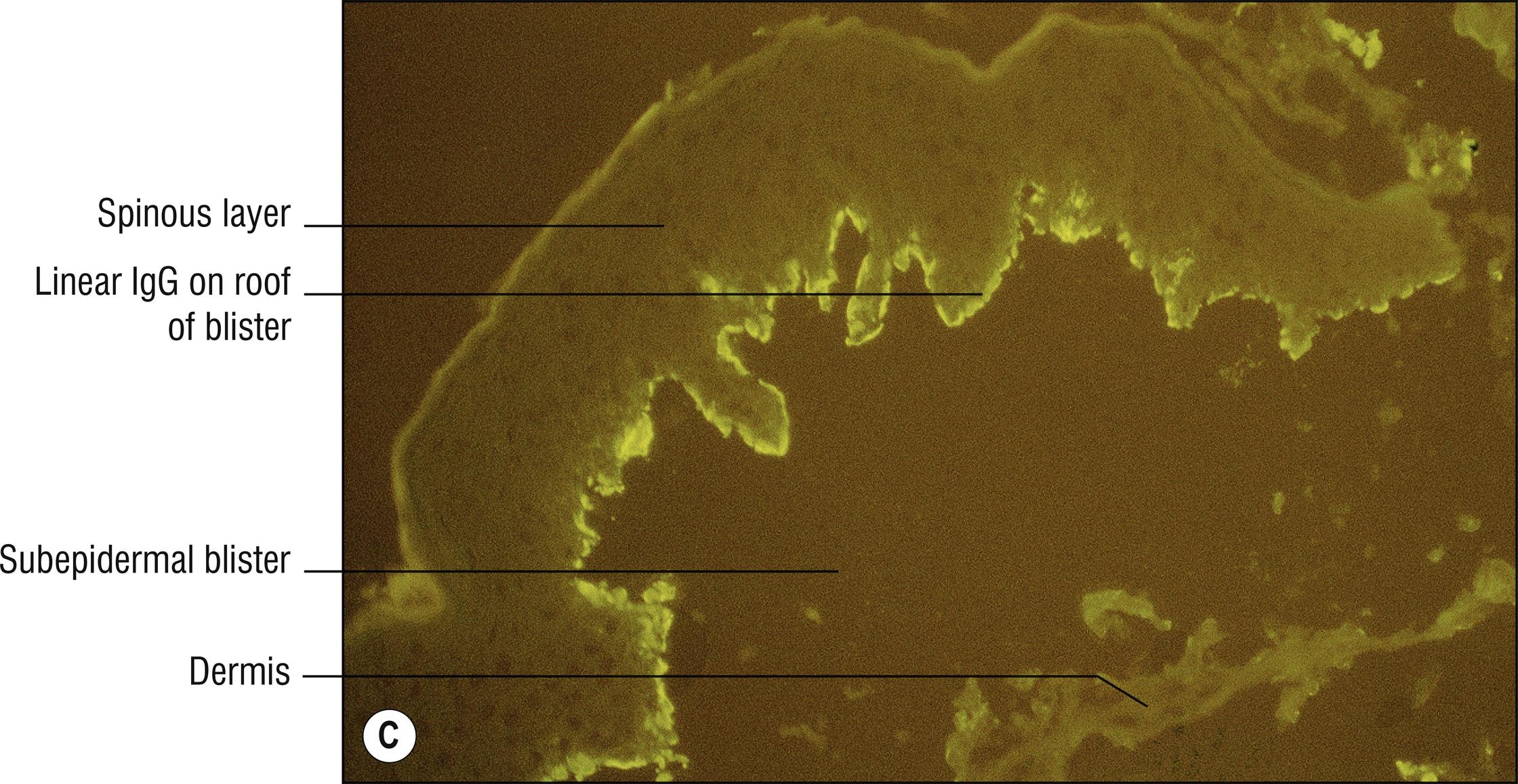
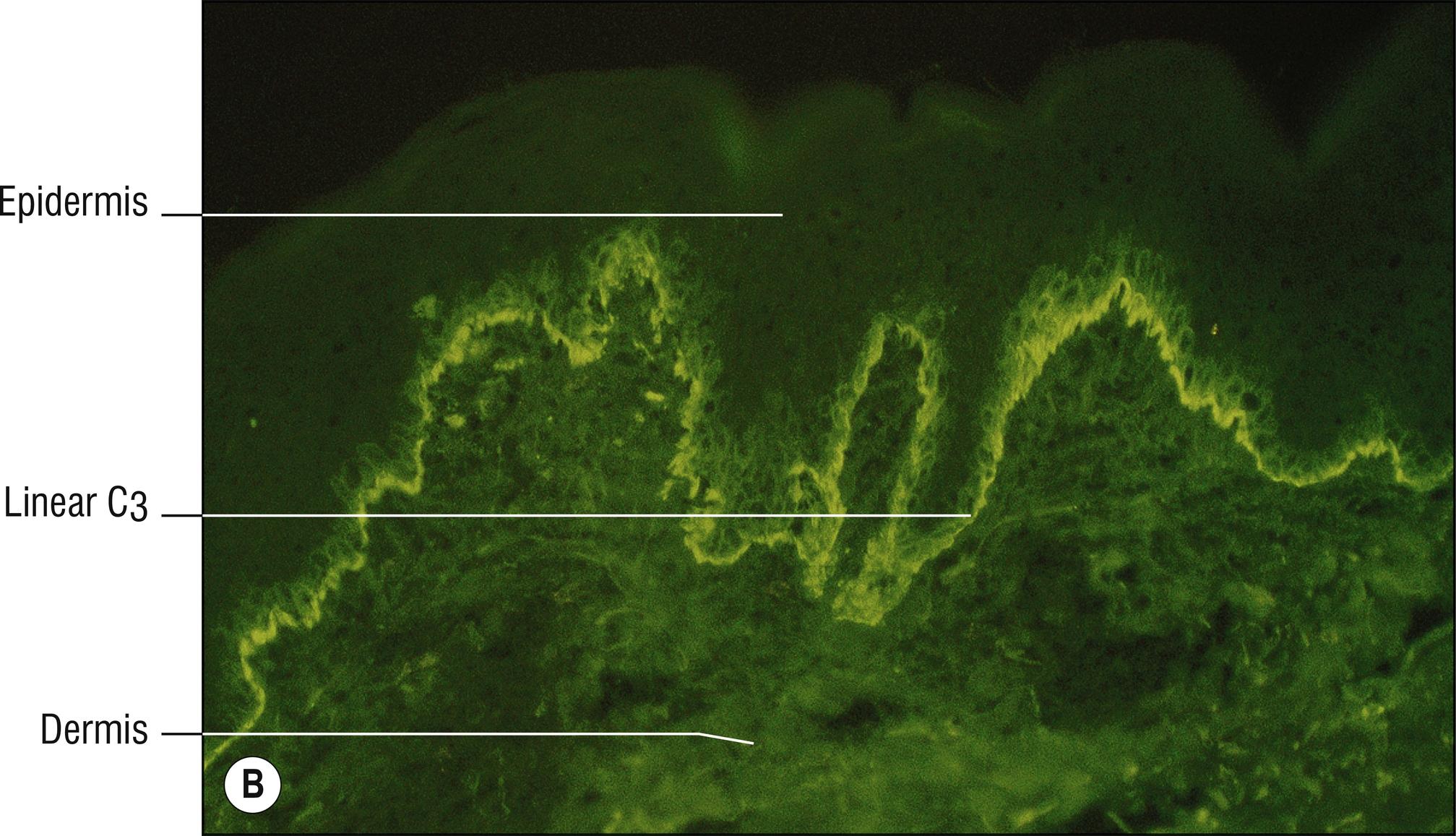
Direct immunofluorescence of perilesional skin reveals linear IgG (usually IgG4) and complement deposits at the basement membrane zone in the lamina lucida (usually on the roof of blister, including salt-split skin preparations, but there are exceptions). Sometimes complement is seen in the absence of IgG.
Localized Brunsting–Perry cicatricial pemphigoid (6.2): lesions are localized to a specific site on the skin, such as the scalp, with scarring and fewer eosinophils. Routine biopsy often nonspecific, with scarring and no obvious blister, but direct immunofluorescence is almost always positive, as in bullous pemphigoid. Indirect immunofluorescence from serum not sensitive (20%). Serum ELISA for BP180 antigen NC16a is 60% sensitive but also found in ordinary bullous pemphigoid. Serum ELISA for BP180 antigen C-terminal is newer test, more specific for cicatrical pemphigoid.
Pemphigoid gestationis (6.3): very similar disease, occurs in pregnancy by definition.
Lichen planus pemphigoides: pemphigoid with a band of lymphocytes resembling lichen planus (2.11).
Pemphigoid nodularis: Prurigo nodularis features (2.3) related to scratching itchy lesions of pemphigoid, often without blistering.
Early lesions without blisters may resemble urticaria or other diseases with eosinophils in the dermis (1.36). Elderly patients with numerous eosinophils in their dermis, even without blistering, usually have pemphigoid rather than a drug reaction or other dermatosis with eosinophils.
Other diseases with subepidermal blisters should be considered (1.147), especially those with eosinophils, those with neutrophils, and those that sometimes are cell poor. Only epidermolysis bullosa acquisita (EBA) (6.6), cicatricial pemphigoid (6.2), and pemphigoid gestationis (6.3) have an immunofluorescence pattern similar to pemphigoid. Pemphigoid and pemphigoid gestationis deposits occur within the lamina lucida, while EBA deposits occur in the superficial dermis. With indirect immunofluorescence using salt-split skin preparations, which produce separation through the lamina lucida, and with biopsies from the edge of blisters, bullous pemphigoid fluorescence is usually found on the roof of the blister, while in EBA fluorescence is found on the floor of the blister.
Rare autoimmune scarring erosions, ulcers , and blisters of mucosal surfaces (mucosal pemphigoid), especially the eyes (1.41) and mouth (1.82). The term mucous membrane pemphigoid is preferred by some over “cicatricial pemphigoid” because of the confusion with the Brunsting–Perry type. This probably is a heterogeneous group of disorders, and autoantigens vary, usually localizing to the lamina densa, with the blister in the lamina lucida.
Subepidermal blister seen in some cases, but squamous metaplasia is often all that is found
Viable or eroded roof over the blister
Perivascular lymphocytes (1.109) with variable eosinophils (1.36), neutrophils (1.89), or plasma cells (1.111, if on mucous membrane)
Direct immunofluorescence is identical to bullous pemphigoid (6.1); indirect immunofluorescence from serum is less sensitive
Localized Brunsting–Perry cicatricial pemphigoid: blistering, eroded, and scarring plaques limited to localized areas of the skin instead of mucous membranes.
Anti-epiligrin mucous membrane pemphigoid: antibodies are directed against alpha subunit of epiligrin (laminin-5), with 20%association with internal malignancy. Immunofluorescence positive on floor of blister instead of the roof. Serum ELISA for IgG against laminin-332 is 80% sensitive and 95% specific.
Other subepidermal blistering diseases should be considered (1.147), but bullous pemphigoid (6.1) resembles it most closely.
Lichen planus (2.11) and pemphigus vulgaris (5.4) often cause similar erosive lesions in the mouth.
(see Fig. 6.3A,B )
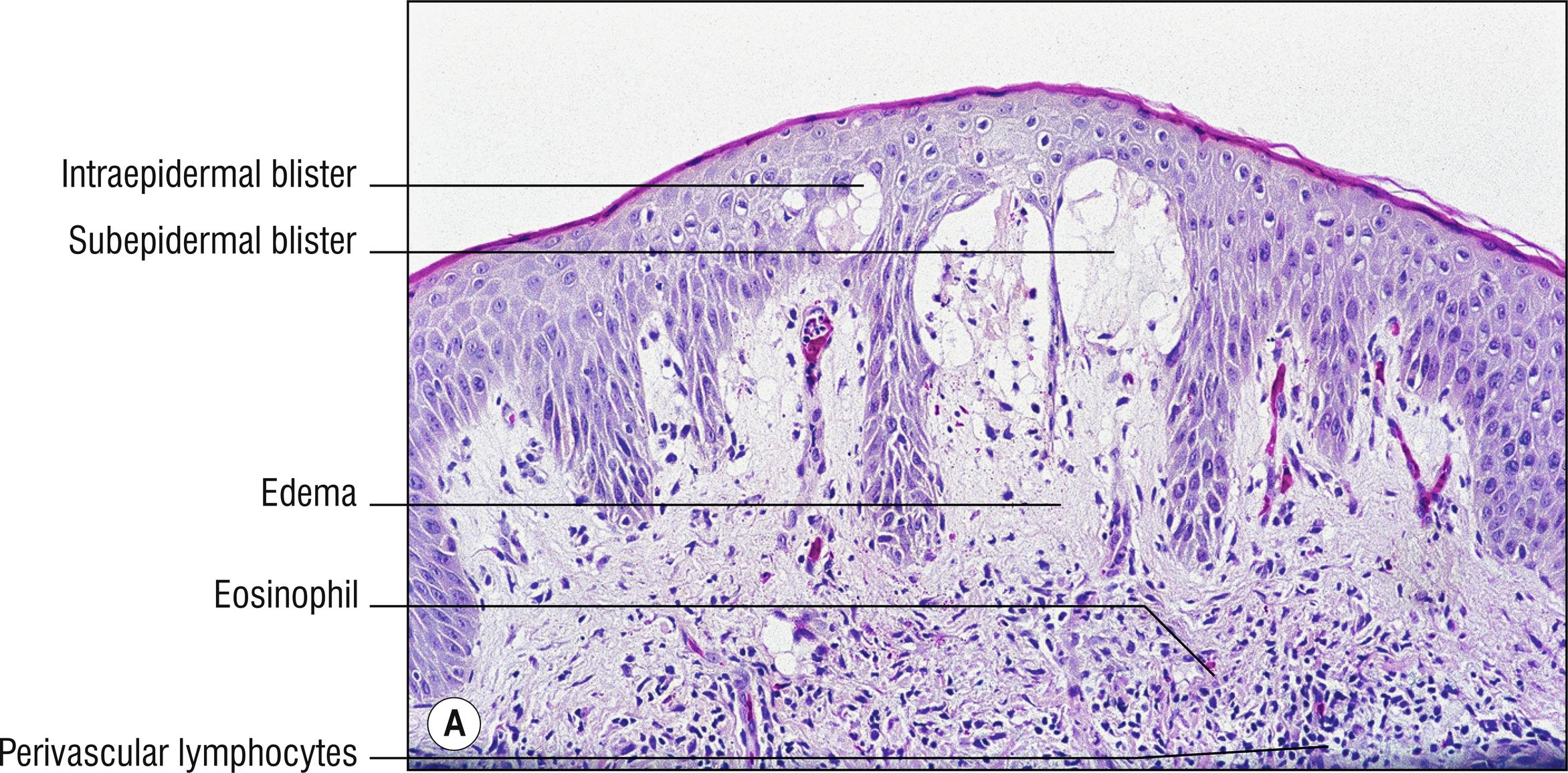
The misnomer “herpes” is unfortunate, as it has nothing to do with herpes virus. Rare autoimmune disease associated with HLA DR3 and DR4, antibodies directed to BP2 antigen (180 kD, in lamina lucida and hemidesmosome, best detected with serum ELISA testing rather than indirect immunofluorescence), vesicles , bullae, or urticarial plaques in the second or third trimester of pregnancy on trunk and extremities, often periumbilical (1.143), controversial increased fetal morbidity or mortality is thought to occur, usually resolves within a few weeks of delivery. About 5% of infants born to affected mothers have self-limited blisters.
Spongiosis (1.132), sometimes eosinophilic spongiosis (1.36) or intraepidermal vesicle
Necrotic keratinocytes sometimes (1.86), especially at basal layer
Marked papillary dermal edema (1.30), subepidermal blister in 70% of cases
Perivascular lymphocytes (1.109) with eosinophils (1.36)
Direct immunofluorescence is identical to bullous pemphigoid (see Section 6.1 ) except that IgG is present less often (40%) than complement alone (100%)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here