Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chronic kidney disease (CKD) is a growing worldwide public health problem, characterized by increasing prevalence, high cost, and poor outcomes. The poor outcomes include progression of kidney disease leading to kidney failure, increased risk for acute kidney injury (AKI), cardiovascular disease (CVD), and mortality, as well as a wide variety of other complications.
In 2002, the Kidney Disease Outcomes Quality Initiative (KDOQI) of the National Kidney Foundation (NKF) sponsored guidelines for the definition, classification, evaluation, and risk stratification of CKD. The purpose of these guidelines was to create uniform terminology to improve communications among all involved in the care and management of patients with CKD, including patients, physicians, researchers, and policy makers. The guidelines were adopted with minor modification by Kidney Disease: Improving Global Outcomes (KDIGO) in 2005. In response to controversy and accumulation of new data, KDIGO sponsored a Controversies Conference in 2009, followed by an update of the guidelines in 2012, which maintained the definition of CKD but modified the classification. Subsequent reviews by national and international guideline workgroups have endorsed maintaining the CKD definition but expressed reservations about some aspects of the classification. The goals of this chapter are to describe the conceptual model for CKD, the revised 2012 KDIGO guideline recommendations for the definition and stages of CKD, and the associated prevalence and clinical action plan, along with commentary by other national and international guideline workgroups. We also provide an overview of detection, evaluation, predicting prognosis, and management, with comments on the role of nephrologists in the care of these patients.
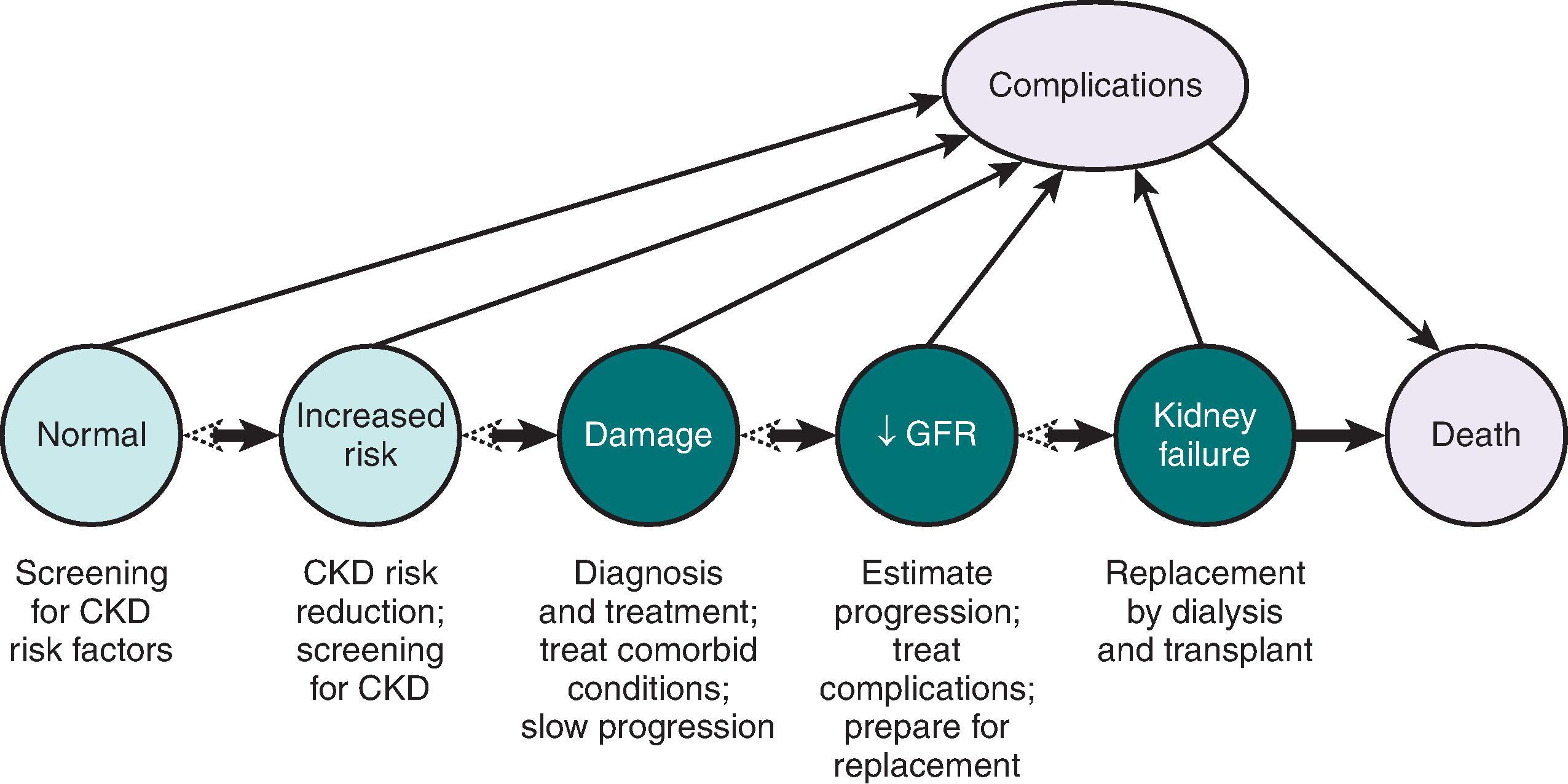
Fig. 51.1 shows a conceptual model for CKD, and Table 51.1 outlines the outcomes. This model describes the natural history of CKD, beginning with antecedent conditions associated with increased risk for developing kidney disease, followed by the stages of CKD (kidney damage, decreased glomerular filtration rate [GFR], and kidney failure), and associated complications.
| Outcomes of Chronic Kidney Disease | KIDNEY DISEASE CHARACTERISTICS | ||
| Glomerular Filtration Rate | Albuminuria | Cause | |
| Kidney Outcomes | |||
| CKD progression (GFR decline and worsening albuminuria) | + | +++ | +++ |
| AKI | +++ | + | + |
| Chronic kidney failure | +++ | + | +++ |
| Complications (Current and Future) | |||
| CVD and mortality | +++ | +++ | ++ |
| Systemic drug toxicity | +++ | + | + |
| Metabolic/endocrine (anemia, bone and mineral disorders, malnutrition, and neuropathy) | +++ | + | + |
| Infections, cognitive impairment, frailty | ++ | ++ | ++ |
Risk factors for the development of CKD include exposure to factors that cause kidney disease, such as hypertension, diabetes, autoimmune diseases, and kidney stones, and characteristics that increase susceptibility to kidney disease, such as older age, minority racial and ethnic status, and reduced nephron mass. The mechanisms underlying increased susceptibility have not been completely described or proven. For example, minority race or ethnicity may imply an underlying genetic tendency or it may be a marker for lack of access to healthcare. Susceptibility factors may explain why a family history of kidney disease, regardless of the cause, places an individual at increased risk for development of kidney disease.
The horizontal arrows in Fig. 51.1 indicate transitions among kidney outcomes. The arrows pointing from left to right emphasize the progressive nature of CKD. However, the rate of progression is variable, and not all CKD progresses; thus, not all patients with CKD develop kidney failure. Early stages of kidney disease may be reversible with treatment, as shown as dashed arrowheads pointing from right to left, and even individuals with kidney failure can revert to earlier stages through kidney transplantation. Studies suggest that CKD is a risk factor for development of AKI and that episodes of AKI may increase the risk for progression of CKD. The earlier stages and the risk factors for progression to later stages can be identified, permitting improvements in outcome by prevention, earlier detection, and initiation of therapies that can slow progression and prevent the development of kidney failure.
The diagonal arrows emphasize complications of CKD other than kidney outcomes. It is well accepted that both decreased GFR and albuminuria are associated with an independent risk of CVD and all-cause mortality. Metabolic and endocrine complications of decreased GFR, including anemia, bone and mineral disorders, malnutrition, and neuropathy, collectively comprising the uremic syndrome, have long been recognized as consequences of kidney failure, but these abnormalities may appear with lesser reduction in GFR. Similarly, nephrotic syndrome occurs in patients with marked albuminuria, but hyperlipidemia and hypercoagulability may be observed with lesser increases in albuminuria. Other complications include threats to patient safety from systemic toxicity from drugs and procedures, as well as an increased risk of infections and impaired cognitive and physical function. Strategies for prevention, early detection, and treatment of CKD complications may prolong survival and improve quality of life, even if there is no effect on kidney disease progression.
The 2012 KDIGO guideline update defines CKD as abnormalities of kidney structure or function, present for longer than 3 months, with implications for health. Criteria for CKD include either kidney damage or GFR of less than 60 mL/min/1.73 m 2 of body surface area lasting for longer than 3 months (90 days; Table 51.2 ). Of note, CKD can be diagnosed without knowledge of its cause.
| Criteria for Chronic Kidney Disease * | |
| Markers of kidney damage | Albuminuria >30 mg/day Urine sediment abnormalities Electrolyte and other abnormalities caused by tubular disorders Pathologic abnormalities Imaging abnormalities History of kidney transplantation |
| Decreased GFR | GFR <60 mL/min/1.73 m 2 |
* Either of the listed items for more than 3 months. CKD, Chronic kidney disease; GFR, glomerular filtration rate.
Kidney damage can be within the parenchyma, large blood vessels, or collecting systems, and is usually inferred from markers rather than direct examination of kidney tissue. The markers of kidney damage often provide a clue to the likely site of damage within the kidney and, in association with other clinical findings, the cause of kidney disease. Because most kidney diseases in North America are caused by diabetes or hypertension, persistent albuminuria is the principal marker. Other markers of damage include abnormalities in urine sediment (e.g., blood cells, tubular cells, or casts), abnormal findings on imaging studies (e.g., hydronephrosis, asymmetry in kidney size, polycystic kidney disease, stones, small echogenic kidneys), and abnormalities in blood and urine chemistry measurements (related to altered tubular function, such as renal tubular acidosis). A history of kidney transplantation is also defined as a marker of kidney damage, and patients with a functioning transplant are considered to have CKD, irrespective of the presence of other markers of kidney damage or the level of GFR.
Decreased GFR for more than 3 months, specifically GFR less than 60 mL/min/1.73 m 2 , represents CKD, irrespective of age. The level of GFR is usually accepted as the best overall index of kidney function in health and disease. GFR less than 60 mL/min/1.73 m 2 represents the loss of half or more of the young adult level of normal kidney function, and it is associated with an increased prevalence of systemic complications. The normal level of GFR varies according to age, sex, and body size. Normal GFR is approximately 120 to 130 mL/min/1.73 m 2 in a young adult and declines with age by approximately 1 mL/min/1.73 m 2 per/yearafter the third decade. More than 25% of individuals aged 70 years and older have GFR of less than 60 mL/min/1.73 m 2 ; whether this results from normal aging or the high prevalence of systemic vascular diseases that cause kidney disease remains controversial. Whatever its cause, GFR less than 60 mL/min/1.73 m 2 in the elderly is an independent predictor of adverse outcomes such as death and CVD.
Kidney failure is defined either as a GFR less than 15 mL/min/1.73 m 2 or initiation of kidney replacement therapy (dialysis or transplantation). A number of terms refer to a severe decrease in kidney function, which is not synonymous with kidney failure. Uremia is defined as severely elevated concentrations within the blood of urea, creatinine, and other nitrogenous end products of amino acid and protein metabolism that are normally excreted in the urine. The uremic syndrome, the terminal clinical manifestation of kidney failure, is the constellation of symptoms, physical signs, and abnormal findings on diagnostic studies that result from the failure of the kidneys to maintain adequate function. End-stage kidney disease (ESKD) generally refers to kidney failure treated by dialysis or transplantation, regardless of the level of kidney function, and is used administratively in the United States and elsewhere. The availability of dialysis and transplantation for the treatment of kidney failure varies around the world, and not all patients with kidney failure choose to receive kidney replacement therapy. Therefore, populations defined as having ESKD might not include patients with kidney failure who are not treated with dialysis or transplantation, and the term kidney failure with replacement therapy (KFRT) has been suggested as an alternative to ESKD.
The NKF-KDOQI classification system for stages of CKD was based on the severity of the disease defined only by the level of GFR. The KDIGO classification adds cause of the disease and level of albuminuria to the level of GFR (CGA classification). Because recent epidemiologic data demonstrate strong graded relationships of the level of albuminuria, as well as the level of GFR, with risks of kidney disease progression, CVD, and mortality, this more detailed classification relates more closely to prognosis (see Table 51.1 ). The cause of disease is generally classified according to the presence or absence of systemic diseases (secondary or primary) and the presumed location of the pathologic-anatomic lesions (glomerular, tubulointerstitial, vascular, cystic, or disease in the kidney transplant; Table 51.3 ). Categories for GFR and albuminuria levels are shown in Tables 51.4 and 51.5 . Fig. 51.2 shows the two-dimensional grid relating the risk of kidney outcomes and mortality to level of GFR and albuminuria. The green, yellow, orange, and red shaded categories represent patients at low, moderate, high, and very high risk of kidney outcomes and mortality, respectively.
| Examples of Systemic Diseases Affecting the Kidney | Examples of Primary Kidney Diseases | |
| Glomerular diseases | Diabetes, autoimmune diseases, systemic infections, drugs, neoplasia (including amyloidosis) | Diffuse, focal, or crescentric proliferative glomerulonephritis; focal and segmental glomerulosclerosis; idiopathic membranous nephropathy; minimal change disease |
| Tubulointerstitial diseases | Systemic infections, autoimmune diseases, sarcoidosis, drugs, urate, environmental toxins (lead, aristolochic acid), neoplasia (myeloma) | Urinary tract infections, stones, obstruction |
| Vascular diseases | Decreased perfusion (heart failure, liver disease, renal artery disease), atherosclerosis, hypertension, ischemia, cholesterol emboli, vasculitis, thrombotic microangiopathy, systemic sclerosis | ANCA-associated vasculitis; fibromuscular dysplasia |
| Cystic and congenital diseases | Polycystic kidney disease, Alport syndrome, Fabry disease, oxalosis | Renal dysplasia, medullary cystic disease |
| Diseases affecting the transplanted kidney | Recurrence of native kidney disease (diabetes, oxalosis, Fabry disease) | Chronic rejection; calcineurin inhibitor toxicity; BK virus nephropathy; recurrence of native kidney disease (glomerular disease) |
| Category | Glomerular Filtration Rate Levels (mL/min/1.73 m 2 ) | Terms | Clinical Action Plan |
| G1 a | >90 | Normal or high | Diagnose and treat the cause Treat comorbid conditions Evaluate for CKD risk factors Start measures to slow CKD progression Start measures to reduce CVD risk |
| G2 a | 60–89 | Mildly decreased b | Estimate progression |
| G3a | 45–59 | Mildly to moderately decreased | Adjust medication dosages as indicated |
| G3b | 30–44 | Moderately to severely decreased | Evaluate and treat complications |
| G4 | 15–29 | Severely decreased | Prepare for kidney replacement therapy (transplantation and/or dialysis) if appropriate |
| G5 | <15 | Kidney failure (add D if treated by dialysis) | Start kidney replacement therapy (if uremia present) or continue conservative management |
a GFR stages G1 or G2 without markers of kidney damage do not fulfill the criteria for CKD.
b Relative to young adult level. CKD, Chronic kidney disease; CVD, cardiovascular disease; GFR, glomerular filtration rate. Note: GFR in mL/min/1.73 m 2 may be converted to mL/s/1.73 m 2 by multiplying by 0.01667.
| Approximately Equivalent Albumin-To-Creatinine Ratio | |||||
| Category | Albumin Excretion Rate (mg/day) | Terms | Clinical Action Plan | ||
| (mg/mmol) | (mg/g) | ||||
| A1 | <30 | <3 | <30 | Normal to mildly increased | Diagnose and treat the cause Treat comorbid conditions Evaluate for CKD risk factors Start measures to slow CKD progression Start measures to reduce CVD risk |
| A2 | 30–299 | 3–30 | 30–299 | Moderately increased * | Treatment with renin-angiotensin system blockers and lower blood pressure goal if hypertensive |
| A3 | >300 | ≥30 | >300 | Severely increased | Treat nephrotic syndrome (if present) |
* Relative to young adult level. CKD, Chronic kidney disease; CVD, cardiovascular disease.
![Fig. 51.2, Prognosis and prevalence of chronic kidney disease in the United States by glomerular filtration rate and albuminuria category. Colors reflect the ranking of relative risk for kidney disease progression and cardiovascular risk. Green, low risk (if no other markers of kidney disease, no chronic kidney disease [CKD]); Yellow, moderately increased risk; Orange, high risk; Red, very high risk. Cells show the proportion of adult population in the United States. Data from the NHANES 1999 to 2006, N = 18,026. Glomerular filtration rate (GFR) is estimated from a single measurement of standardized serum creatinine with the CKD-EPI 2009 creatinine equation. Albuminuria is determined by one measurement of albumin-to-creatinine ratio, and persistence is estimated. Values in cells do not total to values in margins because of rounding. Category of very high albuminuria includes nephrotic range. eGFR, Estimated glomerular filtration rate; KDIGO, Kidney Disease: Improving Global Outcomes; NHANES, National Health and Nutrition Examination Survey. (From Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl . 2013;3:1–150.) Fig. 51.2, Prognosis and prevalence of chronic kidney disease in the United States by glomerular filtration rate and albuminuria category. Colors reflect the ranking of relative risk for kidney disease progression and cardiovascular risk. Green, low risk (if no other markers of kidney disease, no chronic kidney disease [CKD]); Yellow, moderately increased risk; Orange, high risk; Red, very high risk. Cells show the proportion of adult population in the United States. Data from the NHANES 1999 to 2006, N = 18,026. Glomerular filtration rate (GFR) is estimated from a single measurement of standardized serum creatinine with the CKD-EPI 2009 creatinine equation. Albuminuria is determined by one measurement of albumin-to-creatinine ratio, and persistence is estimated. Values in cells do not total to values in margins because of rounding. Category of very high albuminuria includes nephrotic range. eGFR, Estimated glomerular filtration rate; KDIGO, Kidney Disease: Improving Global Outcomes; NHANES, National Health and Nutrition Examination Survey. (From Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl . 2013;3:1–150.)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/StagingandManagementofChronicKidneyDisease/1_3s20B9780323791229000510.jpg)
Fig. 51.2 shows the prevalence estimates derived from measurements of serum creatinine to estimate GFR (eGFRcr) and albumin-to-creatinine ratio (ACR) during National Health and Nutrition Examination Surveys (NHANES) from 1999 to 2006. The prevalence of ACR greater than 30 mg/g or estimated GFR less than 60 mL/min/1.73 m 2 is approximately 11.5% of the US adult population. The proportion of participants with CKD in the groups at moderate, high, and very high risk is about 73%, 18%, and 9%, respectively, representing a prevalence in the general population of about 8.5%, 2%, and 1%, respectively. This prevalence is more than 50 times greater than the prevalence of treated ESKD of approximately 0.2% reported by the US Renal Data System during this interval. Because kidney disease usually begins late in life and progresses slowly, most people in the earlier stages of CKD die of other causes before reaching kidney failure. In these patients, the burden of CKD is reflected in the complications of earlier stages, including increased mortality and morbidity, reduced quality of life, and high cost.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here