Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Foot orthoses—also commonly called orthotics, arch supports, and inserts—have been applied to the treatment of pathologic musculoskeletal conditions for more than a century. The term foot orthosis refers to any orthotic device that is distal to the ankle. This naming convention was introduced in the early 1970s by the Committee on Prosthetic-Orthotic Education.
A foot orthosis may be as simple as a prefabricated arch support available over the counter at the local pharmacy or as complex as a custom-designed device incorporating multiple supportive elements. Whatever the type, the beneficial effects of a foot orthosis are determined by its relative shape, stiffness, and compressibility with respect to the weight-bearing foot.
Although research suggests that foot orthoses are efficacious in the treatment of pathologic musculoskeletal conditions, outcome studies point to considerable variation in the reliability and effectiveness of orthotic treatment. Clinical methodologies have been developed in an attempt to standardize treatment and improve the predictability of the clinical outcome. Still, the results achieved by clinicians often differ, and interpractitioner variability appears to play a major role in the biomechanical response to orthotic intervention. There is little objective evidence regarding how foot orthoses achieve favorable therapeutic results. In spite of this, a growing body of objective evidence suggests that foot orthoses often produce positive clinical outcomes. The potential benefits of a conservative, cost-effective treatment modality arguably justifies the continued prescription of foot orthoses and interest in orthotic-related research. An improved understanding of the mechanisms of action of foot orthoses is necessary to enhance clinical methodologies and better inform their prescription.
Historically the focus of research has been the response of the lower extremity to the mechanical influence of an orthosis. Many studies have attempted to isolate the passive response of the limb by studying patients with neuropathy or utilizing cadaveric specimens.
Study designs have attempted to isolate variables of interest and to measure the discrete mechanical influence of orthotic supportive elements such as base materials, interface materials, and metatarsal/scaphoid pads. Biomechanical studies suggest that foot orthoses are capable of altering plantar pressure distribution, foot and ankle kinetics/kinematics, and knee kinetics.
Brodtkorb et al. found that the thickness of a metatarsal pad was more significant than its positioning in load shielding the metatarsal heads and that the maximum load-shielding effect occurred distal to the apex of the pad.
Kogler et al. isolated the mechanical effects of arch supports as well as full-foot and forefoot wedges on plantar fascial strain. These cadaveric studies demonstrated the load-sharing effect of arch supports with the plantar fascia. The medial column of the foot approximated the arch support's boundaries ( Fig. 116.1 ).
Tsung et al. investigated the effect of arch supports on plantar pressure distribution in patients with sensory neuropathy. In this study, the method of casting determined the shape of the arch support for patients with neuropathy and strongly influenced the plantar pressure distribution. Foot shape was captured with the subjects in non–weight bearing, semi–weight bearing, and full weight-bearing conditions. In their study, the authors found that casting the foot in what they termed semi–weight bearing, with the subject standing with equal body weight on both feet, resulted in an orthotic shape with the least mean plantar pressure. The control of orthotic shape by the magnitude of the physiologic load produced orthoses with predictable, plantar pressure distributions.
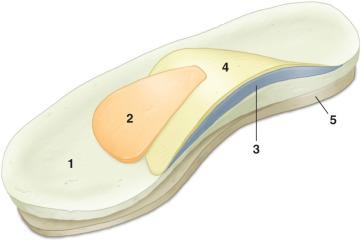
Guldemond et al. investigated the effects of metatarsal pads, arch supports, and full foot wedges on plantar pressure distribution in patients with neuropathy. The orthotic elements were added to a basic insole to alter its relative shape at the medial longitudinal arch and transverse arch. This study revealed that the plantar pressure distribution could be altered in a predictable fashion and that the load-shielding effects of the various elements were additive ( Fig. 116.2 ).

More recent studies suggest that in addition to their direct mechanical influence, foot orthoses can also evoke a neuromotor response that may play a significant role in their function. Evidence suggests that tactile stimuli may, under certain conditions, affect foot and ankle posture. Several authors have investigated the influence of comfort and surface texture on the biomechanical effectiveness of foot orthoses.
Ritchie et al. found that plantar sensory feedback influenced midfoot pronation. The addition of mild, non–mechanically supportive surface features plantar to the medial arch elicited active arch elevation in walking subjects.
Mundermann et al. found that foot and ankle kinematics were related to orthotic comfort. In these studies, orthotic use also significantly changed muscle activity.
The evidence suggests that the neuromotor response to orthotic stimuli may play a significant role in the orthotic influence on biomechanical function. Some manufacturers have even begun incorporating tactile elements in products based on this evidence. At this writing, the orthotic action upon a sensate, volitional foot appears to comprise a complex combination of direct mechanical action and the neuromotor response to the orthotic stimulus.
Further exploration of the tactile response to orthotic mechanical action and the individual and combined mechanisms of action of functional elements in foot orthoses may help to enrich our understanding of the complex nature of foot orthosis design. An improved understanding of these functional elements may ultimately also enhance communication for clinical collaboration and research.
Injuries of the lower extremities are extremely common in runners, and the majority of running injuries are associated with overuse. Although training distance and history of previous injury are primary risk factors, a significant contributing factor is biomechanical abnormality of the lower extremity. At this writing, there is evidence to suggest that foot orthoses may be efficacious in the treatment of metatarsalgia, plantar fasciitis, tendinopathies, stress fractures, compartment syndrome, and shin splints. Foot orthoses may also be efficacious in the treatment of posterior tibial syndrome and foot pain secondary to postural pes planus and pes cavus.
The complexity of the action of foot orthoses in treating foot pathology derives from the complexity of foot and ankle biomechanics and the neuromotor response to orthotic action. The clinician's initial approach to orthotic design is mechanically focused. The process of orthotic design typically begins with identification of the nature and severity of the patient's biomechanical deficits. Orthotic supportive elements are selected with the intent of providing a mechanical influence that may beneficially affect the biomechanical deficits.
The delivery of orthotic care is an iterative process of optimization of the orthotic design based on both subjective and objective clinical indicators. Patient comfort is an important clinical indicator utilized by most clinicians during orthotic fitting and optimization. Comfort in this sense implies not just the tactile feel of the orthosis but also the beneficial change in biomechanical variables associated with orthotic treatment of the pathology. It is difficult to predict the response of a specific foot to orthotic support, which may account for some of the variability in patient satisfaction that occurs when the same condition is treated with a similar orthotic design. Despite having acquired an appropriately prescribed orthosis, many patients require multiple adjustments to achieve pain relief, and such adjustments are critical to ensuring the patient's satisfaction. Some basic guidelines that may serve as a starting point for the prescription of orthoses in the treatment of sports-related injuries are shown in Table 116.1 . Note that these guidelines are intended to serve only as a starting point.
| Pathology | Elements of Orthotic Support in Foot Orthoses |
|---|---|
| Sesamoiditis with no other postural abnormality |
|
| Metatarsalgia |
|
| Morton neuroma with no other postural abnormality |
|
| Plantar fasciitis with mild pes planus |
|
| Mild pes planus |
|
| Moderate to severe pes planus |
|
| Pes cavus |
|
| Diabetes |
|
It is helpful to consider the focal influence of discrete orthotic supportive elements when foot orthoses are being prescribed to treat pathologic musculoskeletal conditions. There is some evidence, for example, suggesting that a simple flat insole added to a shoe may alter the comfort, pressure distribution, friction, or resistance to bacterial growth within the shoe. Polyurethanes and elastomers such as Poron and Spenco, respectively, are examples of resilient insole materials that may enhance a shoe's comfort. Although cushioned insoles influence pressure distribution, it should be noted that there is evidence to suggest that they appear to have a questionable influence overall on shock attenuation. Leather, vinyl, and silver-impregnated fabrics such as X-Static® are examples of interface layers that may influence friction and discourage bacterial growth.
The addition of discrete pads to the native shoe insole may enhance the support or comfort of a shoe. Metatarsal pads and bars, arch pads, lifts, and wedges are support elements that are available in various materials including felt, elastomers, and polyurethanes. Felt is typically supportive, whereas elastomers and polyurethanes are typically more resilient and conformable. Several examples of orthotic materials, pads, and their applications are shown in Table 116.2 .
| Component | Example | Intended Application | References |
|---|---|---|---|
| Foam-cushioned insole | Polyurethane, a Poron EVA, a P-cell polyethylene, a Plastozote |
|
Mills et al. Paton et al. Chiu and Shiang |
| Antifriction insole | Leather interface |
|
Yavuz et al. Lu |
| Antibacterial insole | Silver-impregnated fabric, a X-Static ® |
|
Sedov et al. |
| Metatarsal pad |

|
|
Brodtkorb et al. Guldemond et al. |
| Cushioned heel cup |

|
|
Perhamre et al. |
| Medial/lateral heel wedge |

|
|
Huerta et al. Leitch et al. Bonanno et al. |
| Full-foot medial/lateral wedge | Cork, EVA, or polyurethane Preformed wedge material 
|
|
Shelburne et al. Kogler et al. |
| Arch support (scaphoid pad) |

|
|
Kogler et al. Tsung et al. Kitaoka et al. |
a Acor Orthopaedics, Inc. Cleveland, OH; www.acore.com
The decision whether to prescribe prefabricated or custom foot orthoses involves consideration of the posture of the weight-bearing foot. The inclusion of supportive elements in the design of the orthosis that are intended to treat biomechanical deficits should also be considered. Comfort may associate with the blending of the supportive elements with the anatomical contour, and this may best be achieved using custom devices.
The primary application of prefabricated foot orthoses is the enhancement of medial longitudinal arch support. The shape of these orthoses is designed to fit the average foot; therefore their application is most often limited to feet with normal arch height.
Custom foot orthoses fall into two categories, accommodative and corrective. The basis for the orthotic design of custom foot orthoses is an anatomic model produced by casting, foam impression, contact, or optical scan of the patient's foot.
The shape of the patient's foot in weight bearing determines the shape of an accommodative foot orthosis. Most commonly these orthoses are designed to redistribute focal pressure or to minimize the mean plantar pressure. Rigid deformities of the foot such as posttraumatic pes planus and arthrosis from a Lisfranc injury are best treated with an accommodative orthotic, as any attempt to realign the foot will create increased focal pressure and pain. Diabetic foot orthoses are another example of an accommodative type.
The shape of corrective foot orthoses is also anatomic, but with the inclusion of intentionally incongruous contours termed modifications . Examples of anatomic mold modifications used to create orthotic supportive elements are enhanced or reduced medial longitudinal arch supports, metatarsal pads, medial or lateral heel wedges, and medial or lateral forefoot wedges. The intent of these modifications is the seamless incorporation of supportive elements into the anatomic contour. These elements are often intended to influence foot and ankle kinetics and kinematics by redistributing plantar pressure. The Functional Foot Orthosis and the University of California Biomechanics Laboratory (UCBL) orthosis are two examples of corrective types.
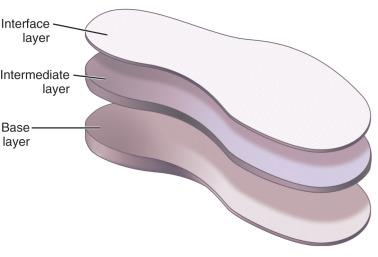
Materials selection is an important aspect of foot orthosis design. Most foot orthoses comprise multiple layers, including a base and intermediate and interface layers. The use of multiple layers offers the combined benefits of their individual properties ( Fig. 116.3 ). Firm base materials such as ethylene vinyl acetate (EVA), with compressibility like that of shoe outsoles, are typically used for the base layer of what are termed soft foot orthoses . Rigid base layers employ materials such as polypropylene, copolymer, and fiber glass or carbon lamination. Laminated foot orthoses typically offer the highest stiffness while taking up the least room in the shoe.
Soft, resilient, and conformable intermediate-layer materials include polyurethane foams, polyethylene foams, and elastomers. The intermediate layer helps to disperse plantar pressure and improve comfort.
The interface layer of a foot orthosis is typically leather, vinyl, or foam; it may enhance the durability and hygiene of the orthosis or alter the friction between the foot and the orthosis. Polyethylene foam such as Plastozote may enhance moisture control, friction, or pressure distribution of the interface layer. Fabrics may enhance the comfort, moisture control, or odor control of the orthosis.
One or more of the supportive elements may be incorporated into the orthotic design by casting or scanning, modification of the anatomic model, and materials selection for fabrication. The function of the orthosis is evaluated during its fitting and optimized for the patient's comfort.
Because early humans were largely dependent on hunting, one can postulate that the earliest footwear was used in running. With civilization's advancement and socialization, shoes took on symbolic functions. Papyrus sandals for religious ceremonies and jeweled sandals for high-fashion gatherings have been discovered at the burial sites of Egyptian pharaohs. Although these have little to do with sports shoes, they do foreshadow the current specialization and fashionable designs of athletic footwear. A shoe designed for sports alone did not come into existence until the latter half of the 19th century. The croquet sandal known as the sneaker had a fabric upper, rubber sole, and laces. Further sports shoe development followed in the late 1800s with the demand for durable but lightweight shoes. It is from these developments that the multibillion-dollar athletic shoe industry evolved in an explosion of sport-specific footwear. Today's casual and professional athletes may select from a broad range of shoes designed for sprinting, running, cross training, volleyball, basketball, hiking, dance, and bowling, among other activities.
Over the last half century, significant progress has been made in the design, materials, and methods used to fabricate athletic shoes. Manufacturers have flooded the market with stylish models. These shoes are packed with inventive features ranging from mesh uppers to directionally siped soles. New features tend to fall in and out of fashion, however, suggesting that the consumer's selection of athletic shoes for sports activities may at times be more about form than function. In reality, the design and performance of the modern athletic shoe has dramatically improved. Manufacturers and independent researchers have performed studies to demonstrate the biomechanical influence of shoe features. While there is evidence that many of these features influence biomechanical variables, their efficacy in the prevention of sports injuries or in the enhancement of performance is less clearly understood. Although it remains difficult to identify specific aspects of design that will reduce sports injuries for a given athlete, fit and comfort appear to play a significant role in injury prevention.
Clinicians have understandably been reluctant to recommend specific footwear for their patients. This reluctance is warranted given the almost overwhelming number of shoe models available, the pace of new product introduction, and the highly individualized nature of shoe fit and comfort. It is beneficial that consumers have a broad selection of shoe models from which to choose. To assist the clinician in helping to guide their patients in their selection, the next section describes some of the features designed into the modern sports shoe and their intended application.
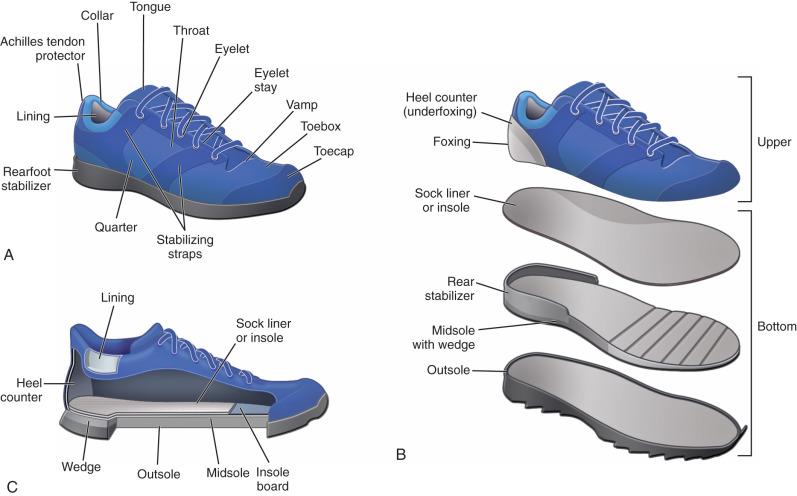
In simplest terms, the shoe can be broken down into the bottom and the upper. The bottom protects the foot, interfaces with the floor, and comprises the outsole, wedge, midsole, and insole. The upper covers the foot, supports the ankle, and comprises the toe box, tongue, closure, collar, and heel counter ( Fig. 116.4 ). Each of these parts plays a role in the form, function, and fit of the shoe. Material properties play a major role in shoe performance, support, and durability.
Advanced manufacturing methods have been developed to give modern athletic shoe sole materials unique physical properties. The primary function of the shoe outsole is to grip the running surface and resist wear. Shoe outsoles may be made of carbon rubber, the same material used for car tires. Carbon rubber is extremely durable, with exceptional wear resistance. Greater hardness imparts greater wear resistance and may distribute the contact forces from the outsole to the midsole more effectively. An outsole that is too hard, however, may impart a “stiff feel” to the shoe. Conversely, an outsole that is too soft may reduce the stability of the shoe. Blown rubber is another example of an outsole material that is sometimes used for the forefoot section of a sports shoe. This material is more flexible and light in weight than carbon rubber but is less durable.
The coefficient of friction (COF) for shoe outsoles may range from 0.1 to 0.34 or higher but is heavily dependent upon the contact surface and is strongly influenced by moisture. Research has shown that sole friction is time- and temperature-dependent as well; it also depends on tread design, even on hard flat surfaces. Shoe manufacturers have employed outsole materials with friction properties suitable for specific sports applications. The nonmarring soles used for volleyball and high-friction outsoles for hiking are two examples.
As stated previously, one function of the outsole is distribution of the compressive load to the midsole. Shoe midsole design has received much attention from shoe manufacturers. Because this is the primary dynamic element of the shoe sole, shoe designers have added ever more creative features to the midsole in an effort to improve stability, attenuate shock, and even enhance motor activation.
Shoe midsoles are most typically made of EVA, polyurethane, or some blend of thermoplastic elastomers (TPEs). Advanced methods have been developed to vary the properties of midsole materials during manufacture. For example, manufacturing methods have been developed that facilitate the selective modification of midsole density along the sole contour, creating regions with different mechanical characteristics. Research has shown that the mechanical characteristics of midsole materials deteriorate significantly under normal use. Thicker materials may deteriorate at a higher rate than thinner materials as well. The rule of thumb is to replace athletic footwear after every 4 to 6 months of regular use.
The geometry of the midsole has also received much attention from shoe designers. Frequently incorporated into the modern athletic shoe midsole is sparse structure and open cantilever or honeycomb structures intended to vary mechanical characteristics and reduce weight. These geometric features are intended to influence the compressibility, energy return, and flexibility of the midsole. Midsole geometry may also incorporate corrugations of various shapes, sipes, and other features to create directionally oriented flexion characteristics in the shoe sole. More recently, some manufacturers have begun adding composite structures in the wedge or midsole to enhance mediolateral stability of the heel, midfoot, or forefoot of the shoe. One example of this approach is New Balance Rollbar Technology.
Any discussion of athletic shoe soles would be incomplete without mention of heel and forefoot rockers. There is considerable evidence to support the role of these features in influencing the kinematics and kinetics of the lower extremity. One recent study found that running with rocker soles may lower mechanical loading on the Achilles tendon; however, loading on the knee joint was found to be increased.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here