Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term splenic marginal-zone lymphoma (SMZL) was coined by Schmid and colleagues in 1992 for a B-cell lymphoma involving the spleen and bone marrow characterized by a micronodular tumoral infiltration that replaces the preexisting lymphoid follicles and shows marginal-zone differentiation as a characteristic finding. SMZL is defined in the WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues as a B-cell neoplasm comprising small lymphocytes that surround and replace the splenic white pulp germinal centers, efface the follicle mantle, and merge with a peripheral (marginal) zone of larger cells, including scattered transformed blasts; both small and larger cells infiltrate the red pulp.
Most cases have a fairly typical clinical presentation characterized by prominent splenomegaly and bone marrow and peripheral blood infiltration. Cells in peripheral blood can frequently be recognized by the villous cytology; this and other findings confirm that SMZL and splenic lymphoma with villous lymphocytes are the same entity.
In spite of the name, the clinical, immunophenotypic, and genetic features of SMZL are different from those in other MZLs, indicating that SMZL is a distinct clinicopathologic entity, unrelated to MALT or nodal MZL.
The incidence of SMZL may be underestimated because until recently the diagnosis was typically made on splenectomy specimens; because splenectomy is not performed in many cases of low-grade lymphoma, it is difficult to compare the incidence of this disease with that of other B-cell lymphomas. Nevertheless, SMZL appears to account for about 1% to 2% of all lymphomas.
The median age at diagnosis is around 65 years, with a range from 30 to 90 years. A female predominance has been found in different series.
Analysis of the immunoglobulin (Ig) genes in SMZL shows biased use of selected VH1 genes (VH1.2), suggesting a role of unknown antigens in the promotion of tumor cell growth. Interestingly, a small fraction of SMZL patients harbor hepatitis C virus, and the therapy directed against hepatitis C seems to influence control of the tumor load in these patients, suggesting that infectious agents play a role in the pathogenesis of SMZL. This role of infectious agents is supported by the similarities between SMZL and so-called hyperreactive malarial splenomegaly.
SMZL is a disorder of older adults, with a median age of around 65 years. Most patients are asymptomatic, and usually the disease runs an indolent course. Splenomegaly is the most common sign, observed in 75% of patients; anemia, thrombocytopenia, or leukocytosis is reported in 25% of patients. Autoimmune hemolytic anemia is found in 10% to 15% of patients. SMZL is infrequently diagnosed incidentally on routine examination, but monoclonal B-lymphocytosis with a marginal-zone phenotype has been recently recognized and could precede some of these marginal-zone lymphomas.
Almost without exception, SMZL involves the bone marrow at diagnosis, and roughly 33% of patients have liver involvement. Tumor involvement of peripheral blood (defined as the presence of absolute lymphocytosis or >5% tumor lymphocytes in peripheral blood) was detected in 68% of cases by Chacon's group and in 57% by Berger's. Abdominal lymphadenopathy was observed in 25%; peripheral lymphadenopathy was observed more rarely (17%). Because of the high frequency of bone marrow or liver involvement, most patients are at Ann Arbor stage IV at diagnosis. Serum paraproteinemia (usually IgM) is observed in 10% to 28% of cases.
Although the diagnostic criteria were initially based on splenic morphology, the conjunction of clinical features, immunophenotype, and morphology usually allows a diagnosis with a reasonably high level of confidence on bone marrow biopsy specimens.
Splenic involvement in SMZL is characterized by a micronodular lymphoid infiltrate in which white pulp follicles are increased in both size and number, with a variable degree of red pulp involvement always present ( Fig. 17-1 ). The follicles typically have a biphasic appearance, with the presence of both a small-cell and a marginal-cell component. The cells in the center of the follicles are small lymphocytes with generally round nuclei and scant cytoplasm; the cells in the marginal zones have irregular nuclear contours and moderately abundant pale cytoplasm. In addition, most cases contain scattered large B cells resembling centroblasts or immunoblasts; in the spleen, these appear in the marginal zone and red pulp, but they can also be seen in the bone marrow and lymph nodes. A reactive or regressed germinal center may be seen in the centers of some nodules, but these are often absent. Neoplastic plasma cells may be present within the germinal centers, forming clusters in rare cases, and in the splenic red pulp, surrounding small arterioles. The cellular composition of the tumor follicles may reflect the capacity of marginal-zone B cells to induce germinal-center development through the transport of immune complexes to the follicular dendritic cells ; this tissue infiltration by SMZL in the bone marrow or other locations is frequently accompanied by the presence of induced lymphoid follicles with reactive germinal centers.
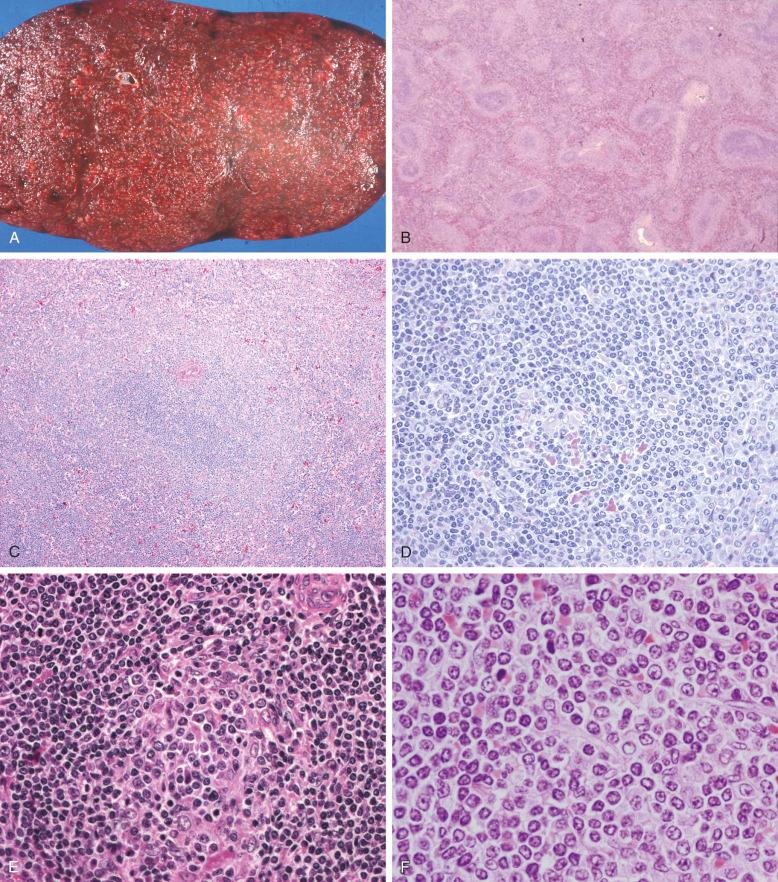
In contrast with the organoid pattern of involvement of the white pulp, mimicking the architecture of normal splenic lymphoid follicles, the red pulp more frequently shows a diffuse pattern of involvement, with infiltration of both the cords and the sinuses. Aggregates of lymphoid cells can also be seen in the red pulp. The cells in the red pulp include both small lymphocytes and large centroblasts or immunoblasts. Epithelioid histiocytes may be present in some cases.
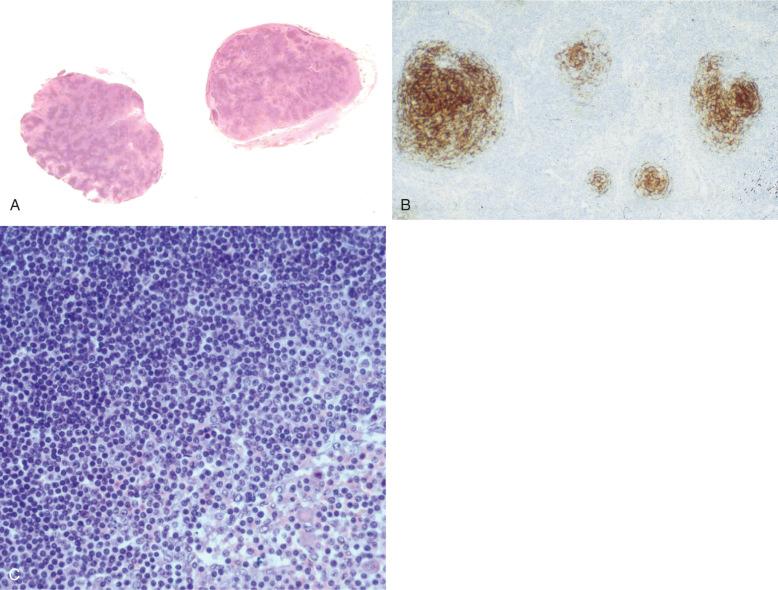
Splenic hilar lymph nodes are commonly involved in SMZL ( Fig. 17-2 ), but lymph node involvement is infrequent in other localizations. In lymph nodes, a marginal-zone pattern is only rarely observed. The pattern is typically micronodular, and the cells are predominantly small; sinuses may be dilated. The variability of the cellular composition of the tumor in various sites suggests that the microenvironment is relevant to the pattern of tumor growth.
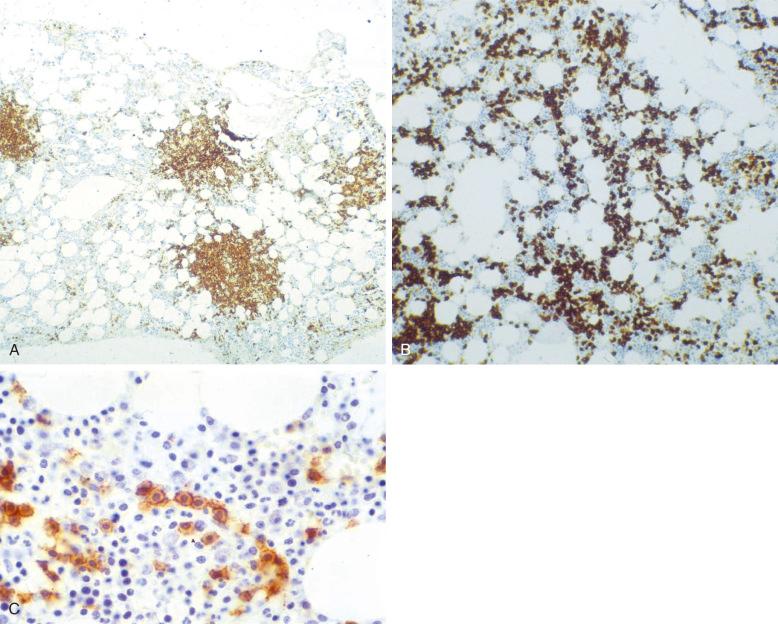
Bone marrow infiltration is the rule in SMZL, although it may be difficult to recognize on routine morphologic sections ( Fig. 17-3 ). CD20 staining helps reveal the presence of intertrabecular lymphoid aggregates and intrasinusoidal small tumor cells. The intertrabecular nodules mimic the architecture and cell composition of tumor nodules in the spleen, with occasional reactive germinal centers surrounded by tumor cells. Characteristically, CD20 staining reveals the presence of linear aggregates of intrasinusoidal B cells. None of these findings is restricted to SMZL, but their combination is quite characteristic.
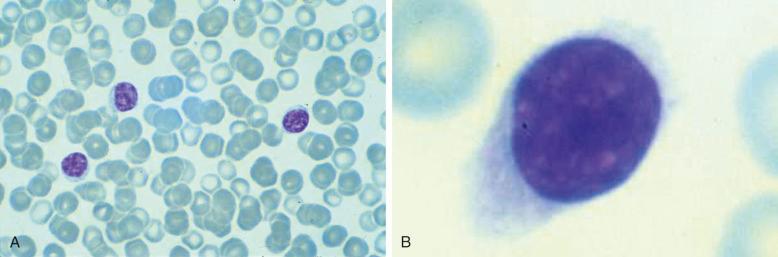
Peripheral blood involvement is less frequent than bone marrow infiltration. However, it is relatively common to find a small number of neoplastic B cells in the blood, some of which may have a villous morphology. This usually takes the form of small cytoplasmic projections at one pole of the rather abundant cytoplasm ( Fig. 17-4 ).
Cases characterized by massive splenomegaly and a morphologic picture of increased large lymphocytes have been described. Unlike in classic SMZL, these cases had a conspicuous component of larger lymphocytes distributed in the marginal zone, occasionally overrunning it, with the isolated presence of the same cells within the central small-cell component and in the red pulp. The bone marrow and peripheral lymph nodes showed similar histologic findings to those described for SMZL in these locations. The genetic and molecular features of these cases showed no alterations specific to other lymphoma types, such as t(14;18) and t(11;14). Instead, there was 7q deletion in three of five cases, p53 inactivation in two of six cases, scattered cyclin D1 + cells in two of six cases, and the presence of translocations involving the 1q32 region in two of four cases.
Immunophenotypic features are summarized in Box 17-1 and shown in Figure 17-5 . The most common profile is CD20 + , CD3 − , CD23 − , CD43 − , CD38 − , CD5 − , CD10 − , BCL6 − , BCL2 + , cyclin D1 − , IgD + , p27 + , and annexin A 1 − . DBA.44 expression has been described in a small fraction of cases. MIB-1 staining shows a distinctive annular pattern, indicating the presence of an increased growth fraction in both the germinal centers and the marginal zones. BCL2 staining helps to distinguish the reactive germinal centers, occasionally infiltrated by BCL2-positive neoplastic cells. MNDA staining has been proposed as a potential diagnostic tool in the differential with follicular lymphoma.
Splenomegaly
Bone marrow involvement
Lymphocytosis with or without villous cells
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here