Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
List the components of a standard obstetric examination in the second and third trimesters, recognize and describe the fetal anatomy recommended for review
Define terminology specific to fetal presentation and fetal situs
Specify equipment and policies required for facilities performing obstetric sonography
Describe sonographic techniques used to image specific fetal structures
Describe normal fetal anatomy visualized in an obstetric sonography examination and variations that may be significant
The second and third trimesters are the ideal time to obtain sonographic images of detailed fetal anatomy. Fetal anatomy may be accurately assessed after 18 weeks of gestation, although structures may be seen earlier in many pregnancies. Technical factors, such as fetal movement, fluid quantity, fetal position, and maternal wall thickness or obesity, may obscure the anatomy and result in less than optimal images throughout pregnancy.
To perform a complete evaluation of the fetus during the second and third trimesters, the sonographer should follow a specific protocol that includes, at a minimum, the components recommended for a standard examination. The practice parameter guidelines for obstetric scanning as outlined by the American Institute of Ultrasound in Medicine (AIUM), the American College of Radiology (ACR), and the American College of Obstetricians and Gynecologists (ACOG) were utilized to create the suggested scanning protocol in this chapter.
This chapter focuses on the fetal anatomy that the sonographer needs to recognize and analyze within a systematic scanning protocol. A sonographer will screen many normal fetuses when performing standard antepartum obstetric examinations during the second or third trimester of pregnancy. A systematic protocol will ensure a comprehensive review of fetal anatomy in each patient. Thoroughness and experience applied to the recommended components and to additional details, such as facial features, open hands, and fetal situs, will maximize the opportunity to detect fetal anomalies.
The protocol for second- and third-trimester sonography examinations includes a biometric and anatomic survey of the fetus (see Box 51.1 ). The second- and third-trimester sonography examination often includes the following:
Observation of fetal viability by visualization of cardiac motion.
Demonstration of presentation (fetal lie).
Demonstration of the number of fetuses. In multiple gestations, anatomy images are obtained on each fetus, growth parameters of each fetus are obtained and compared, placenta and membrane structures are assessed, and amniotic fluid levels in each sac are documented.
Characterization of the quantity of amniotic fluid as normal or abnormal by subjective visualization or by semiquantitative estimates.
Characterization of the placenta, including localization and relationship to the internal cervical os. Placenta previa should be excluded by examination of the lower uterine segment.
Visualization of the cervix. Transvaginal or transperineal imaging may be necessary to document cervical length if there are risk factors for spontaneous preterm birth, when the cervix appears shortened, or if there is a history of uterine contractions. Transvaginal cervical length measurements may be used for screening in low-risk pregnancy.
Assessment of fetal age through fetal biometry. Fetal growth studies may include a serial growth analysis when serial examinations are performed at intervals that are 2 to 4 weeks apart. Typically, the following fetal measurements are included, and gestational age correlation from each measure is averaged to assess fetal age by sonography:
Biparietal diameter
Head circumference
Femur length
Humerus length
Abdominal circumference
Evaluation of uterus, adnexa, and cervix to exclude masses that may complicate obstetric management. Maternal ovaries may not be visualized during the second and third trimesters of pregnancy.
Anatomic survey of the fetus to exclude major congenital malformations. At a minimum, the anatomy specified in Box 51.1 must be visualized. Specialty or repeat studies may be appropriate if anatomy is not well visualized. Technical difficulty in visualizing anatomy should be recorded and images preserved to document visualization of all required components.
Survey uterus and determine fetal number.
Observe fetal cardiac activity.
Determine fetal position(s) and placental location(s).
Check cervix and lower uterine segment.
Survey for uterine or adnexal masses.
Assess amniotic fluid.
Perform anatomy survey of each fetus.
Perform biometric measurements of each fetus.
The sonographer should establish a systematic scanning protocol encompassing elements of the protocol outlined previously, all criteria of the guidelines, and any additional views requested in the practice environment. A referral for a detailed fetal anatomy examination may be necessary when a fetal anomaly is suspected. An organized approach to scanning ensures completeness and reduces the risk of missing a fetal defect.
The second- and third-trimester standard sonography examination requires current two-dimensional real-time sonography equipment with transabdominal and transvaginal capability. Doppler capabilities facilitate evaluation of amniotic fluid volume, the umbilical cord, and specialty evaluations of the fetal heart and other aspects of fetal and maternal circulation. Three-dimensional equipment can record the volume of a targeted anatomic region and represents an advance in imaging technology. The technical advantage of three-dimensional imaging is that it can acquire, manipulate, and display a number of two-dimensional planes within a volume that may not be accessible with traditional real-time imaging. Three-dimensional equipment is currently an adjunct to traditional scanning. Until clinical evidence shows a clear medical advantage, three-dimensional sonography is not considered required equipment.
Practice parameters related to patient education and communication during an examination, competency requirements for sonographers and interpreting physicians, equipment use, scheduling, documentation of results, and image storage specific to obstetric patients must be developed at every facility. Practices that receive ultrasound accreditation from the ACR or the AIUM show improved compliance with published national standards and guidelines. Accreditation is available for fetal echocardiography and for the detailed anatomic examination, as well as for a standard obstetric ultrasound practice.
Recognizing normal fetal anatomy is essential to the performance of obstetric sonography. The task of capturing images of standard anatomic planes and organs in a small and mobile fetus poses a considerable challenge for the sonographer. The “eye” and experience required to recognize abnormal structures develop over time.
A key to developing scanning expertise is to become organized and systematic in assessing the fetus, placenta, and amniotic fluid.
The sonographer should initially determine the position of the fetus in relation to the position of the mother. In determining fetal position and in surveying the uterine contents, the sonographer can systematically move the transducer superior toward the uterine fundus, maintaining a midline path. By angling the probe from side to side, fetal position, cardiac activity, the number of fetuses, the presence of uterine and placental masses, and any obvious fetal anomalies may be recognized and amniotic fluid assessed.
It is important to remember to view cardiac activity at the beginning of each study to ensure that the fetus is alive. If a fetal demise or an obvious anomaly is initially recognized, the sonographer is better prepared to perform the study and involve the physician immediately.
After fetal position is conceptualized, the sonographer determines the left and right sides of the fetus. Being continuously aware of the right and left sides of the fetus is necessary to correctly assess fetal anatomy and situs. Assessment and measurement of the fetus may proceed systematically by moving from fetal head to feet, obtaining anatomy images and measurement at each level. The obstetric sonographer also needs to be prepared to vary this systematic examination and “catch as catch can” when pertinent anatomy presents during fetal movements. The placenta, amniotic fluid, uterus, and adnexa are also examined.
Fetal position may change as a result of fetal movement until actual labor commences. However, fetal position changes less frequently after 34 weeks. Visualizing nonvertex fetal positions after 34 weeks may be predictive of positional difficulties during labor and delivery. An atypical fetal presentation, such as face, brow, or shoulder presentation, will complicate delivery. Similarly, hyperextension of the fetal head may alter obstetric management.
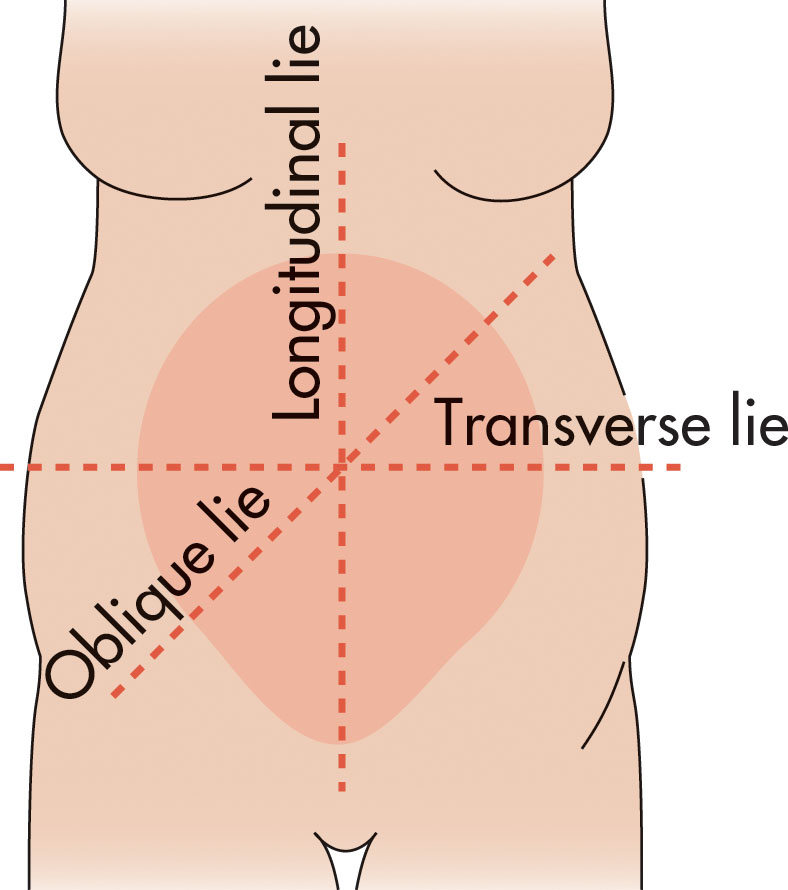
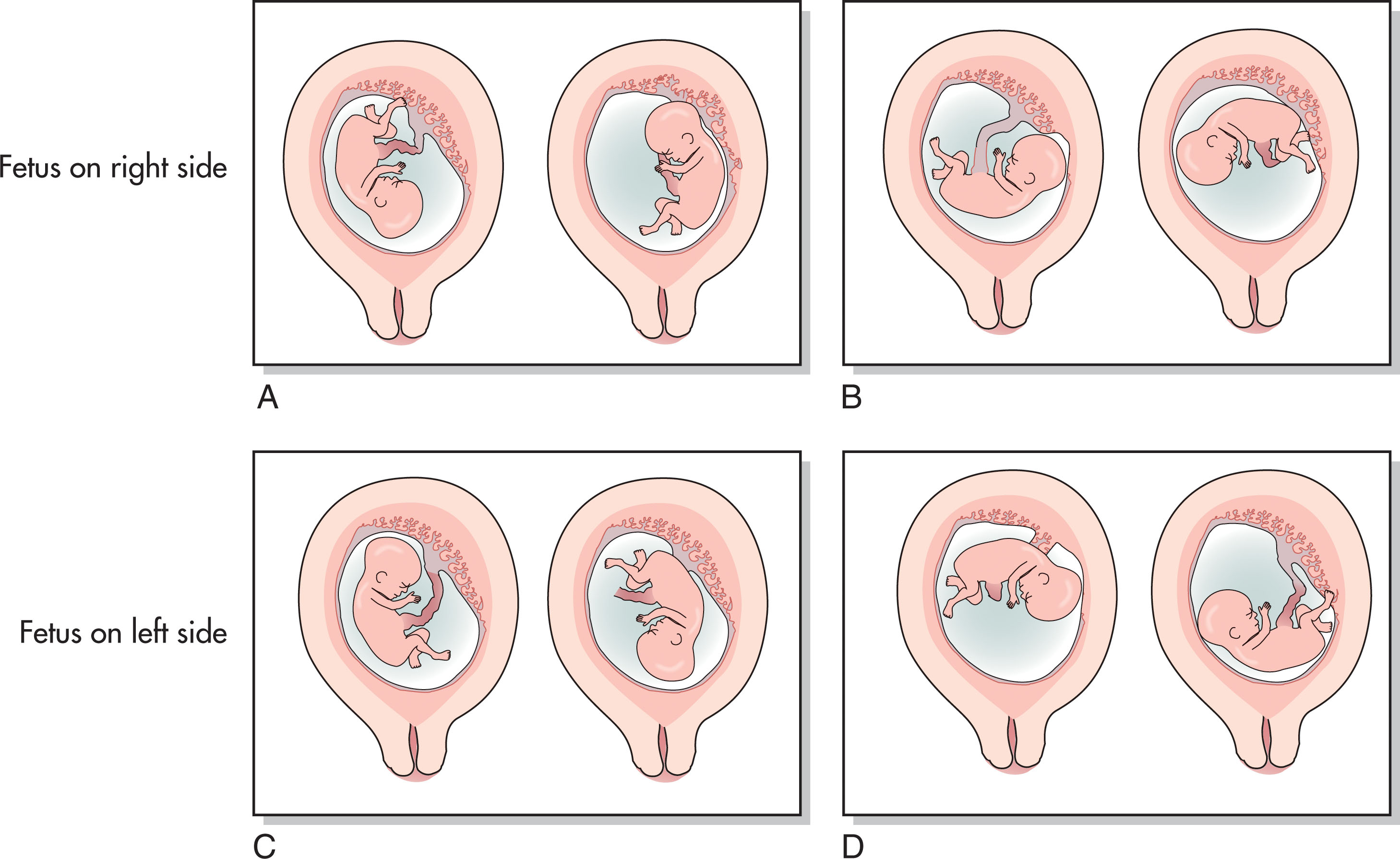
The fetal lie is described in relation to the maternal long axis. Fetuses generally assume a longitudinal, transverse, or oblique lie within the uterus ( Fig. 51.1 ). If the fetus is lying perpendicular to the long axis of the mother, this is described as a transverse fetal lie . When the fetus lie is transverse, the sonographer typically reports the position of the fetal head (maternal right or left) and the position of the fetal spine (inferior, superior, anterior, or posterior) ( Fig. 51.2 ). When the fetal lie is oblique, it is generally described by stating which quadrant of the uterus contains the fetal head and the direction and position of the fetal spine. If the fetus is lying longitudinal or parallel to the maternal long axis, this is described as a vertex (head down) presentation or breech (head up) presentation ( Fig. 51.3 ).
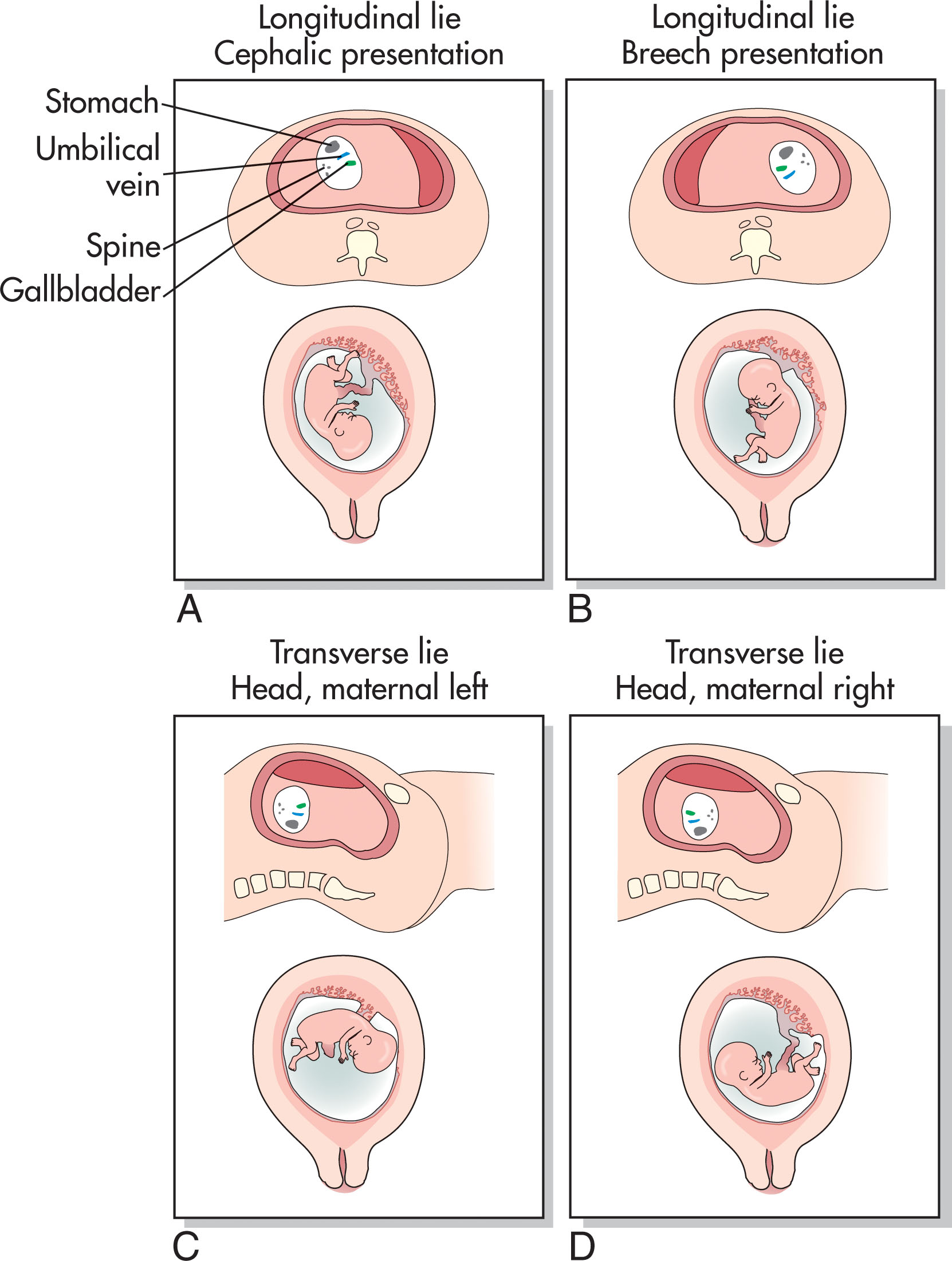
A simple method to determine fetal presentation consists of a midline sagittal scan in the lower uterine segment. Immediately cephalad to the symphysis pubis, the maternal bladder is visualized with the cervix and lower uterine segment posterior. This view allows the sonographer to determine which fetal part is presenting and to check the relationship between the cervix and the placenta. The fetal head is visualized at this level when the fetus is in a vertex or cephalic presentation. Proceeding fundally, if the fetal body is noted to follow the head, a vertex lie is confirmed ( Fig. 51.4 ). The fetal body may lie in an oblique axis to the right or left of the maternal midline. If the body is not initially recognized in the midline, the sonographer should direct the transducer from side to side to search for the abdomen. Identification of the vertebral column when entering the cranium further delineates the fetal lie. The position of a fetus in vertex position may be described by stating the relationship of the fetal occiput (back of the head) to the maternal pelvis. If the occiput is adjacent to the left anterior portion of the maternal pelvis, the fetal position is left occiput anterior. If the occiput is adjacent to the left lateral portion of the maternal pelvis, this is called left occiput transverse. Similarly, fetuses may be described as left occiput posterior, occiput posterior (OP), right occiput posterior, right occiput transverse, right occiput anterior, or occiput anterior. Fetuses that are occiput anterior (looking straight down) or OP (looking straight up) may present technical difficulties in measuring the fetal head and abdomen and in visualizing fetal cranial anatomy.
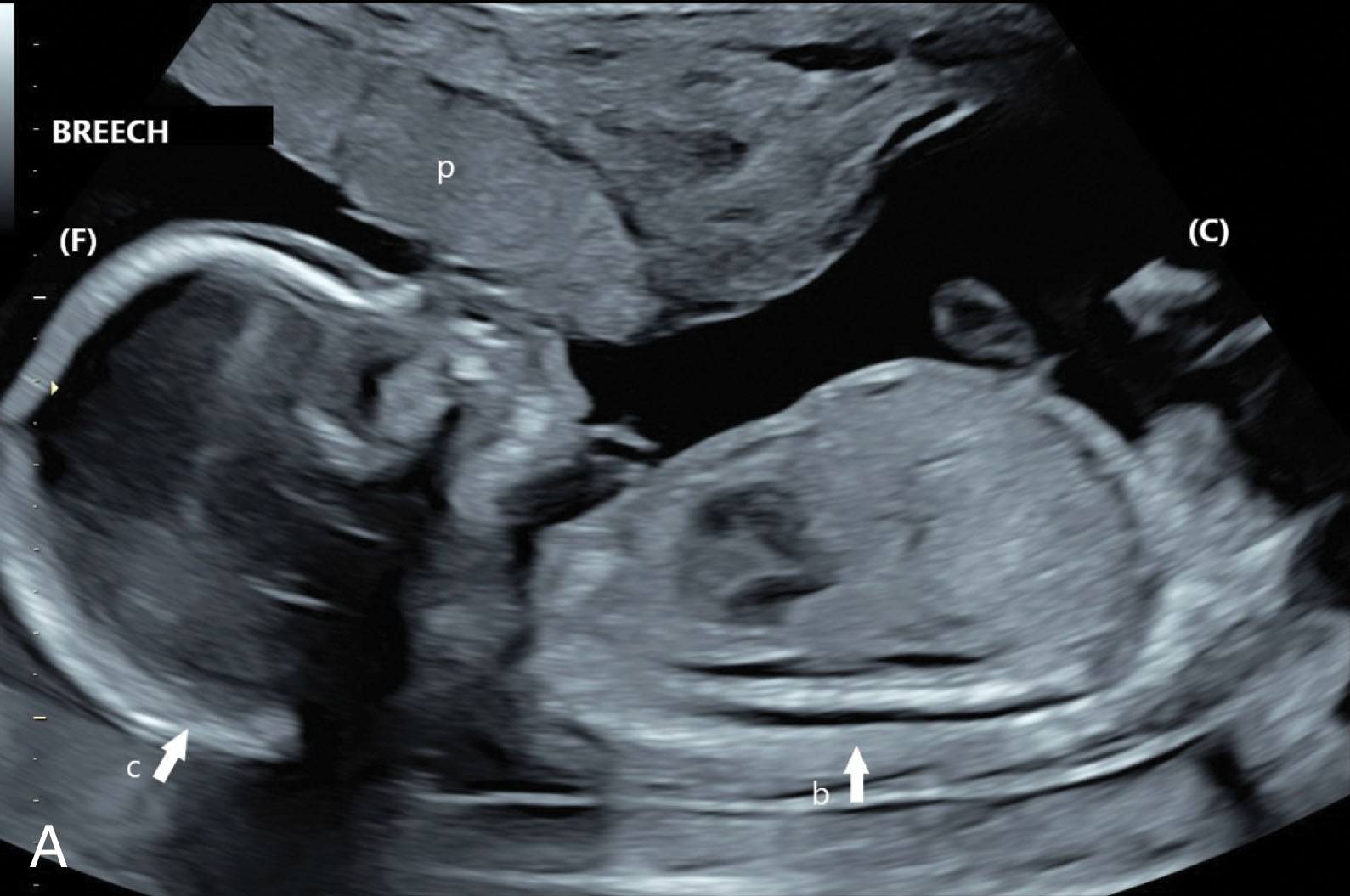
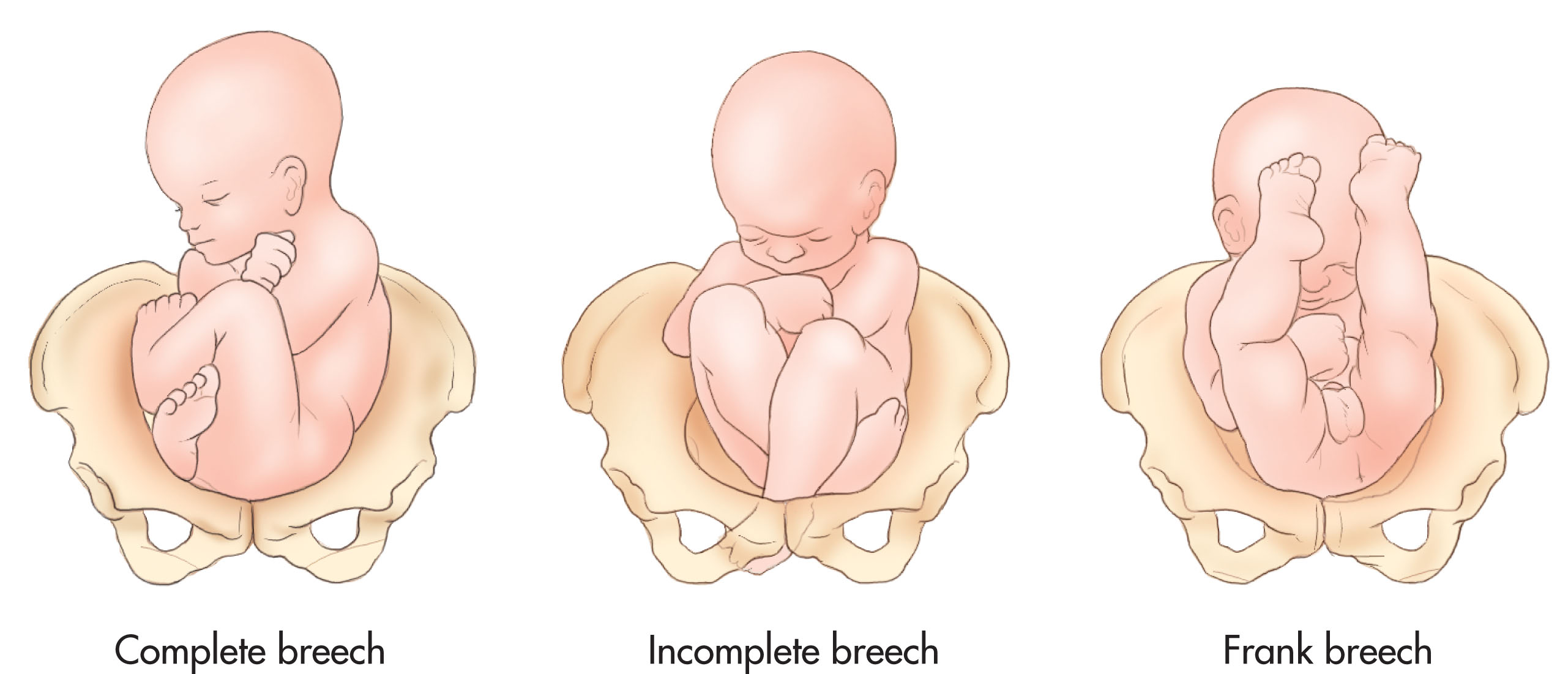
When the lower extremities or buttocks are found to be in the lower uterine segment, and the head is visualized in the uterine fundus, a breech presentation is suspected ( Fig. 51.5 ). In fetuses near term, determination of the specific type of breech lie provides important clinical information for the obstetrician planning the safest route of delivery. Some fetuses in a breech position, such as those in a frank breech position with the thighs flexed at the hips and the lower legs extended in front of the body and up in front of the head ( Fig. 51.6 ), may be safely turned, allowing vaginal delivery. Fetuses in other breech lies, such as complete breech (when both the hips and the lower extremities are found in the lower pelvis), need to be delivered by cesarean section. A footling breech is found when the hips are extended and one (single footling) or both feet (double footling) are the presenting parts closest to the cervix. The position of a fetus in breech position may be described by stating the relationship of the fetal sacrum (lower spine) to the maternal pelvis. If the sacrum is adjacent to the left anterior portion of the maternal pelvis, the fetal position is left sacrum anterior. If the sacrum is adjacent to the left lateral portion of the maternal pelvis, this is called left sacrum transverse. Similarly, fetuses may be described as left sacrum posterior, sacrum posterior (SP), right sacrum posterior, right sacrum transverse, right sacrum anterior, or sacrum anterior. When a fetus is in breech presentation, the shape of the head may appear elongated or dolichocephalic, especially in the third trimester.

When a transverse cross section of the fetal head or body is noted in the sagittal plane, a transverse lie is suspected ( Fig. 51.7 ). By rotating the transducer perpendicular to the maternal axis, the long axis of the fetus may be observed. When a fetus remains in transverse lie late in pregnancy, it is important to screen for a mass or placenta previa in the lower uterine segment that is preventing the fetus from moving into a vertex or breech position.

In addition to determining fetal lie, the right and left sides of the fetus need to be conceptualized to ensure normal situs (positioning) of fetal organs. Some sonographers memorize this relationship. For example, if the fetus is in a vertex presentation with the fetal spine toward the maternal right side, the right side of the fetus is down, and the left side is up. However, it is more helpful to practice maintaining a mental picture of the fetal body and position throughout the examination, which allows recognition of the fetal right and left sides.
A sonographer may also differentiate the right from left side by identifying anatomic landmarks after an initial orientation is verified. For example, if the sonographer initially verifies that the fetal stomach lies on the fetal left side, later in the examination, the fetal right and left may be determined in relation to the stomach. The gallbladder on the right side and the apex of the heart pointing toward the fetal left side may be verified by their relationship to the stomach. The fetal aorta lies slightly to the left of midline, anterior to the spine, and the inferior vena cava is to the right of midline and slightly more anterior to the aorta.
Effective obstetric scanning is founded on the operator’s ability to visualize fetal position.
The sonographer must be adept at recognizing the normal appearances and developmental changes of the fetal brain throughout pregnancy. It is imperative to identify neuroanatomy at specific levels where measurements are obtained, such as a biparietal diameter or posterior fossa, and to screen for malformations in brain development.
By the 12th week of gestation, the cranial bones ossify. It is important to survey the fetal head to check the contour or outline of the skull bones by sweeping the transducer through the cranium from the highest level (roof) in the brain to the skull base. The cranium appears as a circle at the highest levels and as an oval at the ventricular, peduncular, and basal levels. Extracranial masses (e.g., cephaloceles), central nervous system anomalies, skeletal pathology, or fetal death may distort the normal shape of the skull.
Transverse scanning planes are required to evaluate brain anatomy and perform cranial measurements ( Fig. 51.8 ). The transducer is aligned in a longitudinal or sagittal position over the fetus and then is specifically positioned over the fetal head. Rotation of the transducer perpendicular to the sagittal plane generates transverse sections of the brain. Brain anatomy and measurements are assessed in serial transverse planes. A longitudinal or oblique view of the fetal brain may also be used to locate and assess normal anatomy.
Normal fetal brain parenchyma appears hypoechoic because of the small size reflectors and high water content in the tissue. The sulcus and gyrus are more echogenic. The gyral/sulcal pattern of the brain becomes more complex and more prominent as gestational age increases. Branches of the anterior cerebral artery run within the midline sulci and may be seen to pulsate within the echogenic structures.
As pregnancy progresses, brain anatomy may be more difficult to visualize because of increasing calcification of the skull and the position of the fetal head deeper in the pelvis. The calcification of the skull may cause reverberation artifacts in the proximal (near-field) cranial hemisphere that preclude evaluation. Fortunately, most brain anomalies are symmetrical processes, and documentation of the brain may be based on the anatomy seen in the distal hemisphere. In most cases, if there is a defect, it is present bilaterally, even though the anatomy may not be adequately discerned. When a brain anomaly is suspected, and the fetus is in a vertex presentation, use of a transvaginal probe or transperineal scanning may allow better visualization of the skull and brain. Magnetic resonance imaging may also be used to evaluate fetal brain anatomy.
Standard obstetric examination guidelines require the sonographer to image and record the cerebellum, the choroid plexus, the cisterna magna, the lateral cerebral ventricles, the midline falx, and the cavum septum pellucidi. It is also suggested that measurement of the nuchal fold may be helpful during a specific age interval to suggest increased risk of aneuploidy. These specific portions of anatomy are described in the following paragraphs in a systematic review of brain structures seen when moving in transverse planes from the roof to the base of the skull.
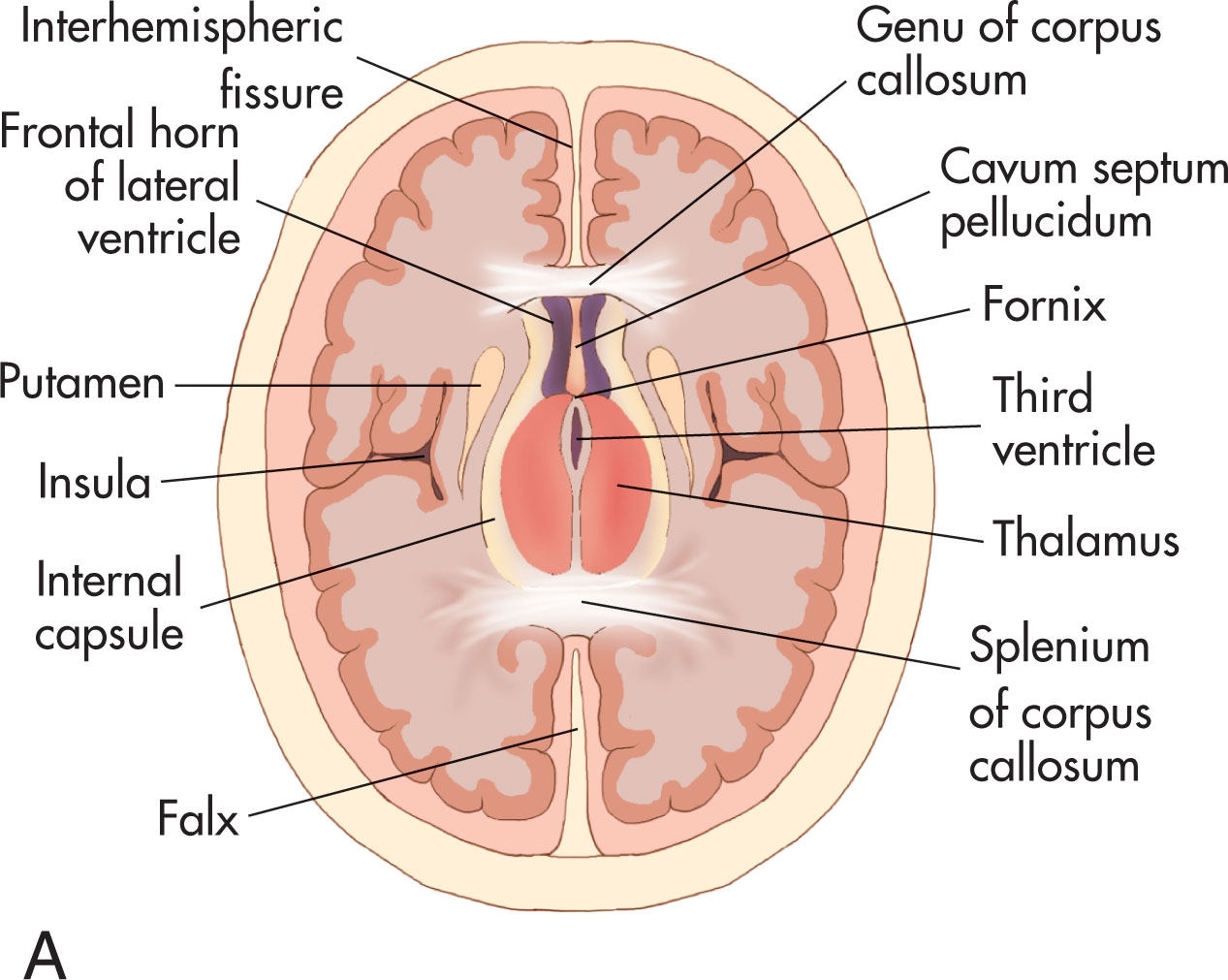
In a transverse plane, at the most superior level within the skull ( Fig. 51.9 ), the contour of the skull should be round or oval and should have a smooth surface. At this level, the interhemispheric fissure, midline echo (falx) , or falx cerebri, is observed as a membrane separating the brain into two equal hemispheres. The midline falx is an important landmark to visualize because its presence implies that separation of the cerebrum has occurred. Lateral and parallel to the midline falx in the superior plane, two linear echoes representing deep venous structures (white matter tracts) are viewed (see Fig. 51.9 ). It is important to recognize that these white-matter tracts are positioned above the level of the lateral ventricles.
The fetal ventricular system consists of two paired lateral ventricles, a midline third ventricle, and a fourth ventricle adjacent to the cerebellum. The ventricular system contains cerebrospinal fluid (CSF), which coats the brain and spinal cord. Choroid plexus tissue within the lateral ventricles produces the CSF. Choroid plexus tissue is located within the roof of each ventricle, except at the frontal ventricular horns. This spongelike material is echogenic and is very prominent in early pregnancy. Occasionally, small cysts—which are engorged, spongelike cavities—may be seen in normal pregnancy. It is thought that CSF may become trapped during development within the neuroepithelial folds, resulting in the formation of choroid plexus cysts. This commonly represents a normal fetal development, but these cysts are also associated with trisomy 18. As the cerebral hemispheres grow, the ventricular system and the choroid plexus appear to occupy a much smaller portion of the cranium.
From the lateral ventricles, the fluid travels to the third ventricle through the foramen of Monro. From the third ventricle, the fluid travels through the aqueduct of Sylvius to the fourth ventricle. When the fluid reaches the fourth ventricle, it flows into the cerebral and spinal subarachnoid spaces from the interventricular foramina and the foramen of Luschka. CSF then spreads through the cisterns and surrounds the hemispheres along the subarachnoid spaces. After reaching the arachnoid granulations, it is reabsorbed and enters the venous system (e.g., cranial venous sinuses).
The fetal ventricles are important to assess because ventriculomegaly or hydrocephalus (dilated ventricular system) may be a sign of central nervous system abnormalities. Mild ventriculomegaly may also be associated with congenital anomalies. Aqueductal stenosis at the level of the aqueduct of Sylvius is the most common type of fetal hydrocephaly and will result in excess fluid in the lateral and third ventricles. Dilation of the entire system, including the fourth ventricle, is associated with spinal defects.
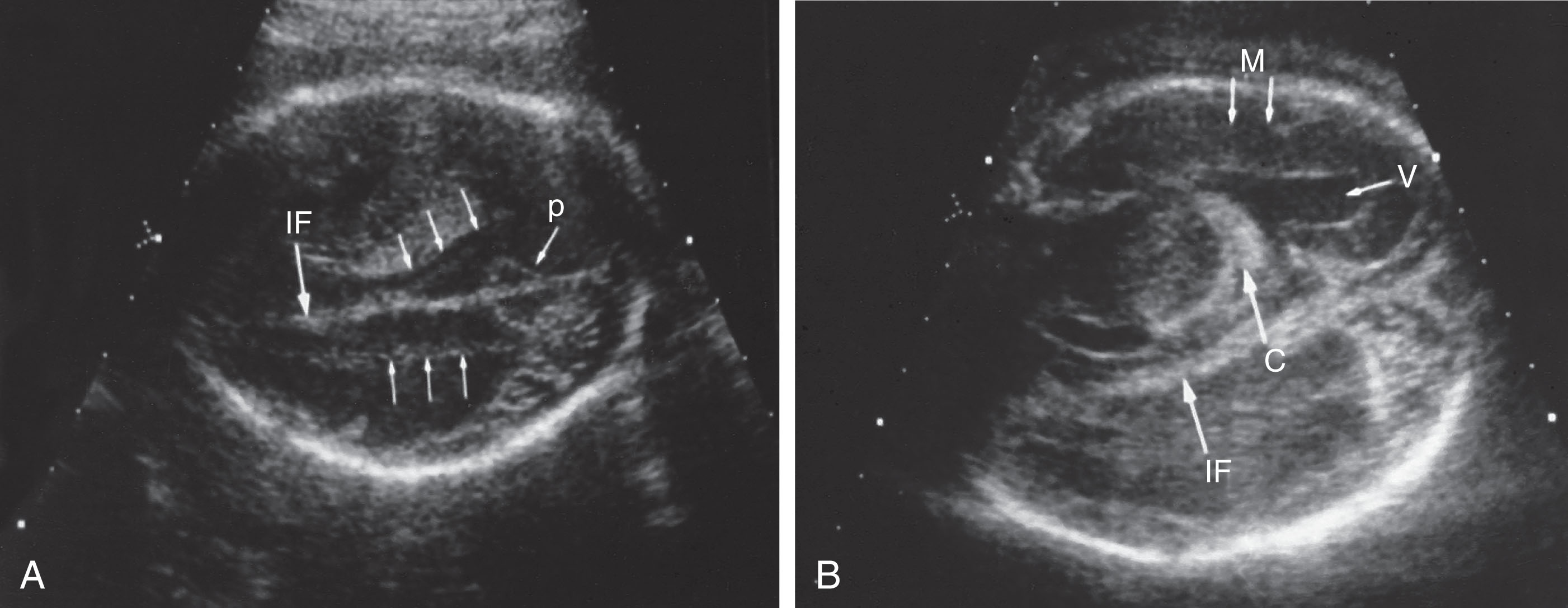
The lateral ventricles are viewed at a level just below the white-matter tracts ( Fig. 51.10 ). The lumina of the ventricles may be recognized by the bright reflection of their borders and the presence of hyperechoic choroid plexus tissue that fills the cavity of the ventricles early in gestation. The lateral borders of the ventricular chambers are represented as echogenic lines coursing parallel to the midline falx. The lateral ventricle is more easily imaged in the distal hemisphere because of reverberation artifacts in the near field. The ventricular cavity is seen sonographically as a cystic space filled with choroid plexus ( Figs. 51.11 and 51.12 ).
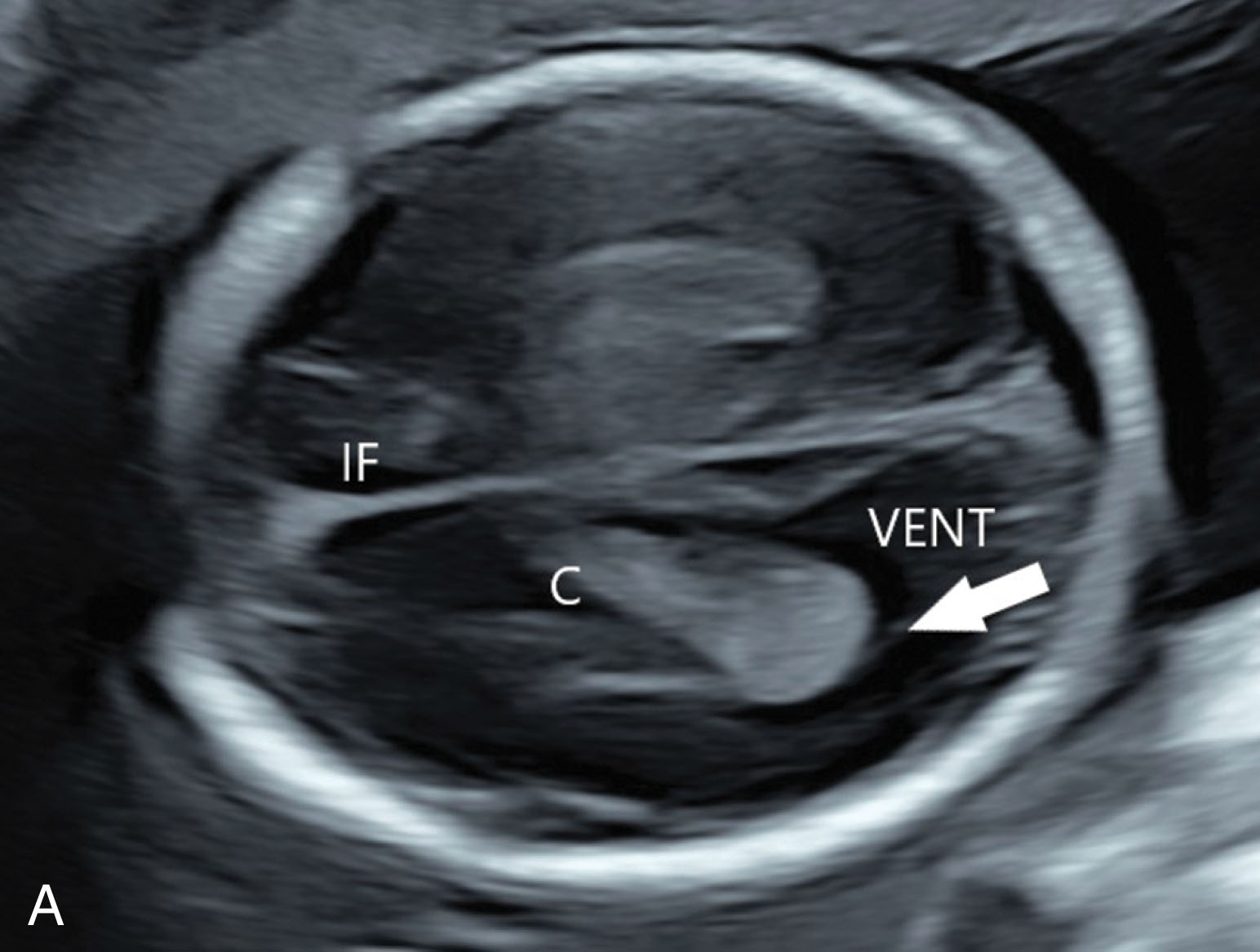

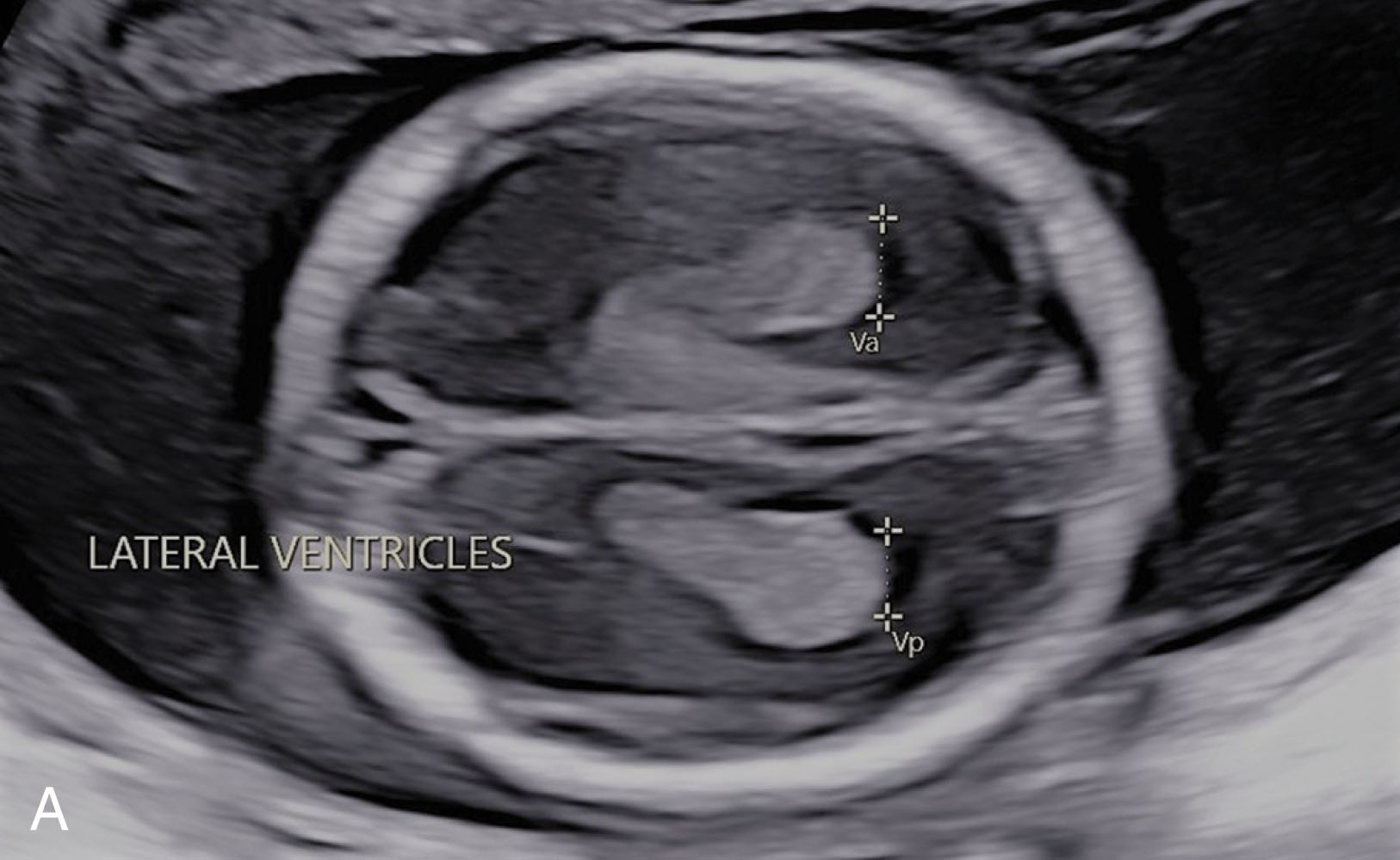
The inferior portion of the lateral ventricles connects with the temporal (inferior) and posterior horns. This portion of the ventricle is called the atrium of the lateral ventricles . The choroid plexus is tear shaped. The most inferior portion of the choroid plexus body or glomus marks the site of the atrium. The glomus or body of the choroid plexus will fill the lateral ventricle in a normal pregnancy. If the glomus appears to float or dangle within the cavity, this is a sign of abnormally enlarged or dilated ventricles (ventriculomegaly). Measurements of the atrium portion of the ventricle are clinically practical because the size of this portion remains the same throughout gestation.
When measuring the ventricle, the sonographer locates the atrium and measures directly across the posterior portion, measuring perpendicular to the long axis of the ventricle rather than the falx while placing the calipers at the junction of the ventricular wall and lumen or cavity of the ventricle (see Fig. 51.10 ). The normal atrium measures 6.5 mm. If the atrium measures greater than 10 mm, this warrants serial imaging and further evaluation.
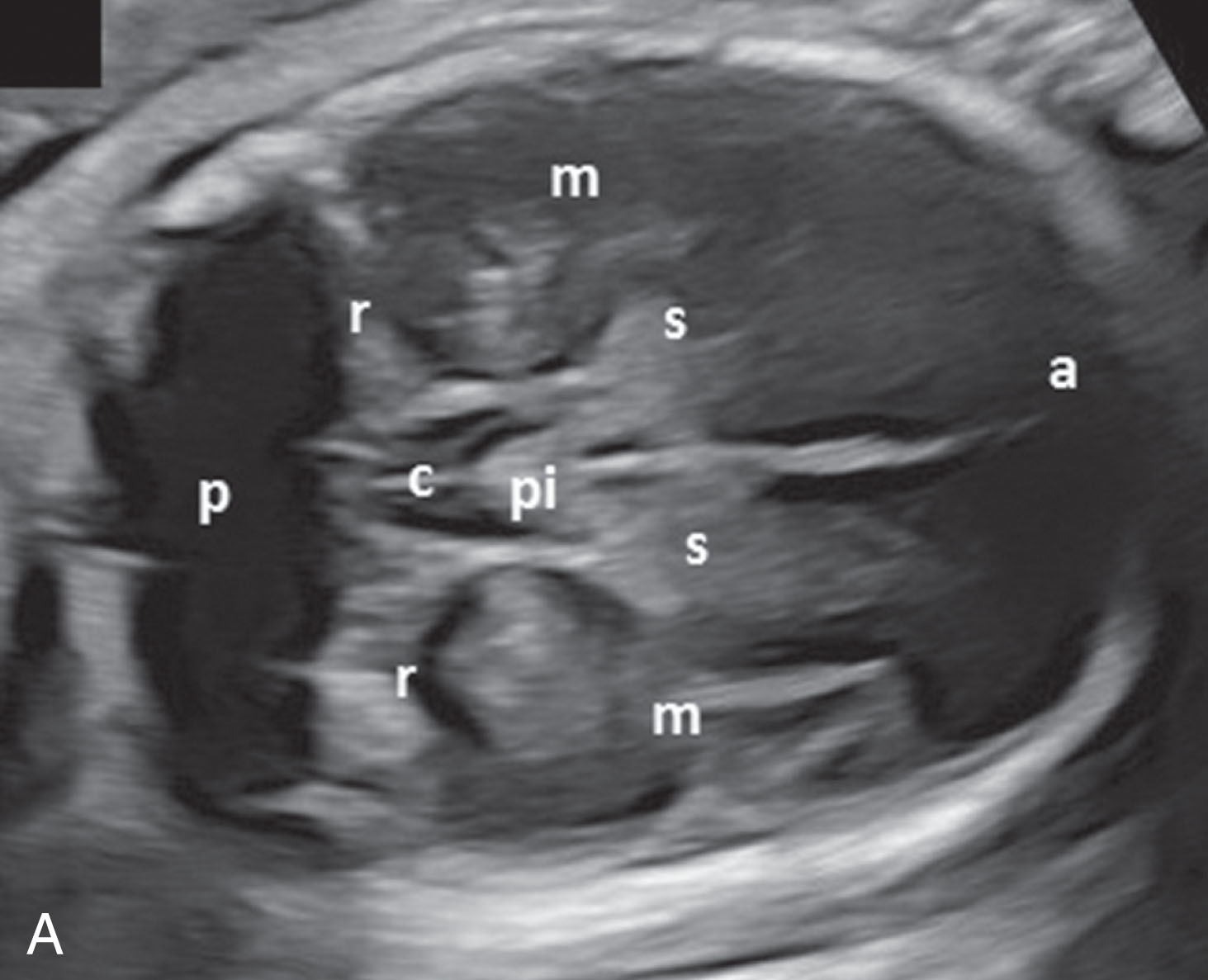
Moving the transducer slightly inferior to the ventricular atrium identifies the area of the thalami and the ambient cisterns. This is the widest transverse diameter of the skull and is therefore the proper level at which to measure the biparietal diameter and head circumference. The midline brain structures (see Fig. 51.12 ) include the cavum septum pellucidum (CSP), the midline echo, and the paired thalami lying on either side. The thalamus resembles a heart with the apex projected toward the fetal occiput.
Between the thalami lies the cavity of the third ventricle (see Fig. 51.12 ). In the same scanning plane, the box-shaped CSP is observed anterior to the thalamus. The CSP is the space between the leaves of the septum pellucidum.
At this transverse level, the frontal horns of the ventricles may be seen as two diverging echo-free structures within the frontal lobes of the brain. The frontal horns are prominent in the presence of ventricular dilation. The corpus callosum is an echogenic structure seen in the transverse plane as the band of tissue between the frontal ventricular horns. The corpus callosum can be better appreciated as a linear band in a sagittal view from the top of the fetal head, but this plane is often not accessible in pregnancy.
The ambient cisterns are pulsatile structures vascularized by the posterior cerebral artery bordering the thalamus posteriorly. When scanning laterally in the brain, the temporal lobe is visible, along with evidence of the insula (i.e., the sylvian cistern complex). The insula appears to pulsate because of blood circulation through the middle cerebral artery, which courses through the insula (see Fig. 51.12 ). The subarachnoid spaces may be seen projecting from the inner skull table.
As the transducer is moved toward the base of the skull, the heart-shaped cerebral peduncles are imaged ( Fig. 51.13 ). Although similar to the thalamus in shape, they are smaller. Pulsations from the basilar artery are observed between the lobes of the peduncles at the interpeduncular cistern. The circle of Willis may be seen anterior to the midbrain and appears as a triangular region that is highly pulsatile as a result of the midline-positioned anterior cerebral artery and lateral convergence of the middle cerebral arteries. The suprasellar cistern may be recognized in the center of the circle of Willis.

The cerebellum is in back of the cerebral peduncles within the posterior fossa. The cerebellar hemispheres are joined together by the cerebellar vermis ( Fig. 51.14 ). It is important to recognize the usual configuration of the cerebellum because distortion may represent findings suggestive of an open spina bifida. The banana sign is the sonographic term that describes the Arnold-Chiari malformation in which the cerebellum may be small or displaced downward into the foramen magnum. Measurements of transverse cerebellar width allow assessment of fetal age and permit necessary follow-up in fetuses with spinal defects and other anomalies of the cerebellum.
The cisterna magna (a posterior fossa cistern filled with CSF) lies directly behind the cerebellum ( Fig. 51.15 ). A normal-appearing cisterna magna may exclude almost all open spinal defects. The cisterna magna is almost always effaced (thinned out) or obliterated in fetuses with the Arnold-Chiari malformation changes associated with spina bifida. The cranial changes occur because tethering of the spinal cord resulting from spina bifida pulls brain tissue downward, obliterating the cisterna magna. In patients at low risk of spinal defect, confirmation of a normal posterior fossa suggests the absence of spina bifida. Because evaluation of the fetal spine remains challenging in excluding small spinal defects, cranial findings associated with this disorder may be very helpful in screening for these lesions.

Enlargement of the cisterna magna may indicate a space-occupying cyst, such as a Dandy-Walker malformation or other abnormalities of the posterior fossa. Enlargement is often a normal variant. The normal cisterna magna measures 3 to 11 mm, with an average size of 5 to 6 mm. Measurements of cisterna magna size are obtained by measuring from the vermis to the inner skull table of the occipital bone. Within the cisterna magna space, linear echoes, which are paired, may be observed posteriorly. These echogenic structures represent dural folds that attach the falx cerebelli (see Fig. 51.14 ).
In the second trimester, the thickness of the nuchal skin fold is measured in a plane containing the cavum septi pellucidi, the cerebellum, and the cisterna magna. Values of skin thickness of 5 mm or less up to 20 weeks of gestational age are normal. Fetuses with thickened nuchal skin are at increased risk for aneuploidy.
At the base of the skull, the anterior, middle, and posterior cranial fossae are observed (see Fig. 51.14 ). The sphenoid bones create a V-shaped appearance as they separate the anterior fossa from the middle fossa, with the petrous bones further dividing the fossa posteriorly. At the junction of the sphenoid wings and the petrous bones lies the sella turcica (site of the pituitary gland).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here