Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Image-guided interventional procedures in the spine and the appendicular skeleton are used in the diagnosis and treatment of various medical conditions of benign or malignant origin. The procedures that are described in the present chapter should be performed by appropriately trained interventional radiologists, who work within a wider multidisciplinary team of clinical specialists that may include neurosurgeons, orthopaedic surgeons, oncologists and pain physicians. Interventional radiologists are trained to perform safely and effectively a variety of bone and soft-tissue percutaneous interventions under appropriate medical indications and can manage relevant procedure-related complications.
Percutaneous bone biopsy is a minimally invasive procedure with the advantages of low cost, low morbidity, high accuracy and repeatability, and it has replaced open surgical bone biopsy in most cases. Fluoroscopy-guided bone biopsy was first described in the 1970s, and image-guided bone biopsy is currently a critical part of the management of musculoskeletal lesions, including primary tumours, bone metastases and bone infections. Spinal applications include image-guided biopsy of the vertebrae, the sacrum and the iliac bones. Disc aspiration for the investigation of spondylodiscitis is also widely practised. Under x-ray or computed tomography (CT) guidance a cutting or trephine bone biopsy needle can be used to access and sample small lesions in difficult anatomies, such as the vertebral body or intervertebral discs, without surgical exploration. The introduction of reusable hand-held battery-powered mechanical drill systems has recently transformed the practice of percutaneous skeletal biopsies, with significantly better diagnostic yield, more versatile use and especially less painful access of almost all hard osteosclerotic lesions.
Before considering an image-guided spinal biopsy, all relevant medical history, laboratory tests and relevant imaging findings must be analysed thoroughly and discussed with the multidisciplinary team. The multidisciplinary team usually includes the spinal neurosurgeon, the musculoskeletal radiologist, the responsible oncologist and an experienced cytopathologist. Correlation with plain films and magnetic resonance imaging (MRI) is critical to avoid unnecessary procedures in certain benign lesions with typical imaging appearances (‘do not touch lesions’). Well-recognised and accepted indications and contraindications for spinal biopsies are outlined in Table 87.1 . In general, skeletal biopsy is indicated to identify tumour or infection. If bone metastasis is suspected, biopsy should be undertaken only if the result will influence oncological management. Spinal biopsy may also be considered for tumour staging or to compare histological characteristics in patients with synchronous or metachronous metastatic cancer. Primary musculoskeletal tumours require identification, grading and often cytogenetic analysis to determine appropriate treatment strategies and prognosis. A bleeding diathesis is the only absolute contraindication to spinal biopsy because it can cause severe haemorrhage or epidural haematoma that may compromise the spinal cord. Alternative options and the risk–benefit ratio should be considered in all patients with spinal lesions that are difficult to access percutaneously.
| Indications |
|
| Contraindications |
|
Correction of coagulopathy, informed consent and consideration regarding conscious sedation or general anaesthesia constitute key elements of preoperative assessment for all spinal biopsy procedures. Anticoagulant agents such as warfarin, direct oral anticoagulants and heparin must be stopped before the procedure according to local institutional policy. A platelet count less than 50,000/mL must be corrected by a platelet transfusion. Bleeding diathesis with an international normalised ratio (INR) greater than 1.3 to 1.5 may be reversed with transfusions of fresh frozen plasma or cryoprecipitate as needed. Antiplatelet agents must be stopped in all cases of spinal interventions at least 5 days before the procedure to correct platelet dysfunction.
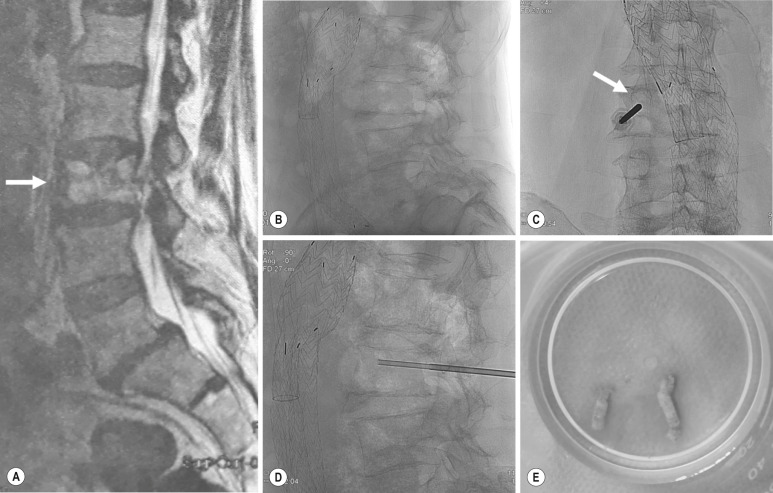
Image guidance may be real-time plain fluoroscopy based on bony landmarks or CT, which offers higher soft-tissue resolution but is not real time. There are several different routes for performing an image-guided spinal biopsy depending on lesion anatomy and size. Typically, patients are placed in a prone or lateral decubitus position. The transpedicular or posterolateral approach is often used for lumbar vertebral body biopsy ( Fig. 87.1 ). The intercostovertebral approach is usually indicated for the thoracic spine and an anterolateral approach with manual displacement of the large vessels is recommended for the cervical spine. Fluoroscopic guidance is the technique of choice for the majority of spinal procedures and may be supplemented by CT for cervical lesions ( Fig. 87.2 ). Biplane fluoroscopy and rotational flat panel angiography with cone beam CT capabilities are emerging techniques for enhanced image guidance during difficult spinal procedures. CT fluoroscopy is readily available in many institutions but is generally avoided because of the increased radiation exposure. An oropharyngeal approach is indicated for the biopsy of C1 or the dens. A posterior oblique CT-guided approach is usually chosen for biopsy of the pedicles and the other posterior spinal elements or the surrounding soft tissues. The access route will also depend on the image-guidance techniques available. For the rest of the skeleton, such as bone biopsy of the pelvis and/or the long bones, the needle pathway is adapted so as to avoid critical nerve and vascular structures. Beware that certain musculoskeletal tumour lesions may be eligible for curative surgical resection; thus, certain anatomical compartments, not involved by the tumour, must not be breached by the biopsy needle. This is especially true for soft-tissue sarcomas and osteosarcomas to limit local recurrence after resection. Nevertheless, the risk of tract seeding following musculoskeletal fine-needle aspiration is very low, estimated to be 3 to 5/100,000 cases.

Routine monitoring of vital signs is necessary during all skeletal procedures. Percutaneous vertebral biopsy may be a painful procedure because of osseous puncture, and conscious sedation is necessary. Sedation is routinely administered using a combination of fentanyl and midazolam according to national and international guidelines. General anaesthesia may be necessary on a case-by-case basis.
In patients with multiple skeletal metastases, the largest and most easily accessible lesion should be chosen. The integrity of the underlying weight-bearing bone must also be considered, although the risk of postbiopsy iatrogenic bone fracture is very low. In patients with painful vertebral pathological fractures, consideration of palliative cementoplasty following successful histological analysis is worthwhile to improve quality of life. Bone sampling may be accompanied by sampling of adjacent soft tissues, and percutaneous disc biopsy may include biopsy of the neighbouring subchondral vertebral end plates to increase the diagnostic yield. When planning a bone biopsy, mixed sclerotic-lytic or contrast-enhancing lesions are preferred as target lesions compared with hypodense or cystic areas that often contain necrotic components. Beware of certain spinal lesions, such as renal cell carcinoma metastases and haemangiomas, which may be highly vascular and can be associated with an increased risk of haemorrhagic complications that may produce compressive neurological sequelae. Different specimens must be sent for histology, cytopathology and microbiology.
With regard to needle choice, the length of the needle (10 to 20 cm long) must be appropriate to the depth of the lesion. Spinal bone biopsies require the use of 11- to 15-G trephine needles that obtain an adequate core of bone marrow. Spinal trephine needles are inserted through a matching outer cannula that is hammered to penetrate the osseous cortex, as necessary. Routine 16- to 20-G core biopsy cutting needles are used in patients with tumours that have a soft-tissue component or extensive osteolysis. Fine-needle aspiration with a 20- to 22-G needle (Chiba needle) is usually adequate for sampling intervertebral discs and the aspiration of collections. Larger-bore needles are preferred for percutaneous biopsy of the vertebrae because of their rigidity and ability to be hammered or drilled into the bone. Battery-powered automated drilling biopsy systems have recently been made available for routine bone marrow biopsy and can be used in patients with bony lesions that have a thick overlying cortex or, in cases of particularly osteosclerotic lesions, to improve sampling yield. Depending on the indication, trephine core biopsy for histology may be combined with coaxial fine-needle aspiration for cytology and microbiology.
The reported diagnostic accuracy of spinal bone biopsies is greater than 95%, but there is always a small risk of a non-diagnostic outcome because of insufficient tissue sampling or sampling of necrotic or sclerotic areas. The diagnosis of spinal metastatic tumours is considered to be generally easier than primary bone tumours, but the diagnostic yield also depends on lesion size and accessibility. In general, more than three needle passes are recommended to obtain an adequate volume of tissue and increase biopsy success. Multiple core biopsies are required for the diagnosis of lymphoma, whereas fine-needle aspiration may suffice for the diagnosis of metastasis and infection. Large core trephine biopsy is indicated for investigation of primary bone tumours like osteoblastomas. The diagnostic accuracy of percutaneous disc biopsy for the investigation of infectious spondylodiscitis is approximately 50%, and the rate of negative cultures may well exceed 60%, even when paravertebral or intervertebral disc fluid collections are aspirated. The most commonly isolated pathogen in infectious spondylodiscitis is blood-borne Staphylococcus aureus , and empirical antibiotic treatment may be initiated even without definite diagnosis. Antibiotics can be stopped 24 to 48 hours before tissue sampling to increase the diagnostic yield from fluid cultures.
Lumbosacral radicular pain is defined as pain radiating to one or more lumbar or sacral dermatomes caused by nerve root compression producing irritation and inflammation. The pathology is also known as sciatica or nerve root pain. Radiculitis (only radicular pain) should be distinguished from radiculopathy that includes objective findings of sensory or motor disturbance. Lumbosacral radicular pain is the commonest form of neuropathic pain, with an annual prevalence of 9.9% to 25% in the general population. Pain usually resolves spontaneously in two-thirds of patients within 12 weeks of onset. However, almost a third of patients continue to suffer from radicular pain after 3 months to 1 year. Before the age of 50, the most frequent cause is disc herniation, whereas after the age of 50, degenerative spine changes are more prevalent. Radiating pain may be sharp, stabbing, throbbing or burning, and the diagnosis is based on medical history and medical examination. Dermatomal distribution, pain that increases while bending forward or coughing and a positive Lasègue or crossed Lasègue test are the usual clinical findings. Disc herniation most commonly occurs in the L4 to L5 (approximately 30%) and L5 to S1 (approximately 50%) intervertebral segments, and the L4, L5 and S1 roots are the ones most commonly affected. MRI may confirm the presence of a disc herniation, but the specificity of the examination is very low because incidental disc herniations are detected in 20% to 36% of asymptomatic individuals.
Selective segmental nerve blocks, whereby a specific nerve root is anaesthetised via an image-guided transforaminal injection of a small amount of lidocaine, may be helpful in excluding one level if negative, but positive blocks are considered non-specific because of significant overlap between innervation of adjacent segments. Transforaminal blocks may simultaneously block afferent input from the corresponding nerve root, the sinuvertebral nerve that innervates the intervertebral disc anteriorly and the dorsal ramus that innervates the facet joint and the muscles posteriorly at the same level. Therefore the differential diagnosis between true radiculitis, discogenic low back pain and mechanical low back pain originating from the facet Z joints may be difficult. It is crucial that any red flags (trauma, cancer and infection) are excluded during diagnostic work-up of the patient. The physician should watch out for a previous medical history of cancer or unexplained weight loss, structural spinal deformities, symptoms appearing before the age of 20 or after 50 and acute neurological deficits that may require urgent surgical decompression. For example, a patient with acute cauda equina syndrome with saddle anaesthesia, sacral polyradiculopathy and sphincter dysfunction must be referred for emergent neurosurgery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here