Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
List risk factors for shoulder dystocia.
Recognize shoulder dystocia.
Describe maneuvers used to relieve shoulder dystocia.
Apply a team-based approach to shoulder dystocia.
Identify complications of shoulder dystocia.
Shoulder dystocia is an obstetric emergency. It occurs when, following delivery of the fetal head, routine gentle traction fails to deliver the fetal shoulders.
Known risk factors for shoulder dystocia include:
High birth weight
Diabetes mellitus
Previous shoulder dystocia
Postterm pregnancy
Abnormal labor progress
Operative vaginal delivery
Male fetal gender
Maternal obesity and high gestational weight gain
Advanced maternal age
African-American
Most shoulder dystocia cases occur in women with no risk factors. The obstetric team must be prepared for the possibility of shoulder dystocia with every delivery.
Scheduled cesarean delivery is reasonable in the following cases:
Prior shoulder dystocia, especially with a severe neonatal injury
Estimated fetal weight >4500 g in women with diabetes (estimated risk of shoulder dystocia 15%)
Estimated fetal weight >5000 g in women without diabetes (estimated risk of shoulder dystocia >20%)
In addition, women with estimated fetal weights >4000 g who undergo a trial of labor become high risk for shoulder intrapartum if they have a prolonged second stage or require an operative vaginal delivery.
Shoulder dystocia is a subjective clinical diagnosis. During delivery of the fetal head, difficulty with birth of the face and chin may be present. When the head of the infant is born, it remains tightly applied to the vulva. In addition, the “turtle sign” or retraction of the fetal head against the maternal perineum may be present.
Difficulty or failure to accomplish external rotation of the head after it has passed the perineum is another sign suggestive of shoulder dystocia. Finally, resistance to the delivery of the anterior shoulder with the usual amount of traction applied to the fetal head should alert the delivering provider of the diagnosis of shoulder dystocia.
CALL FOR HELP!! Personnel in the delivery room should include:
An experienced care provider
Two labor and delivery nurses
A neonatologist
An anesthesiologist
State clearly “There is a shoulder dystocia.”
Explain to patient the presence of shoulder dystocia and the need for additional maneuvers
Position the patient with her buttocks at the edge of the bed, lower the bed, and request a stool to assist with specific maneuvers
Note the time the head was delivered (START THE CLOCK)
Evaluate the need for episiotomy. This will not relieve the shoulder dystocia but will allow more room for performing maneuvers
If the bladder is distended, drain it
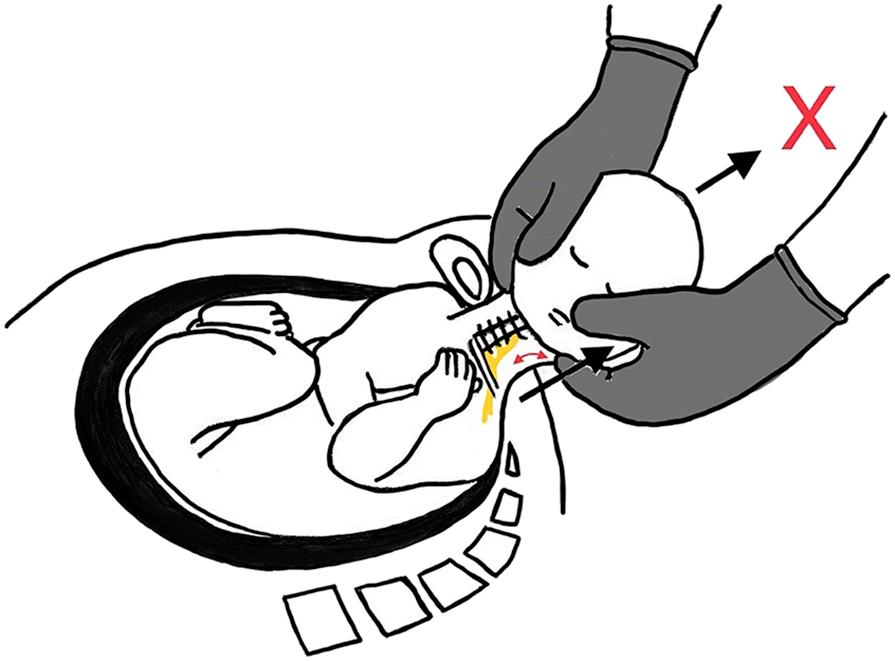
Avoid excessive head and neck traction ( Fig. 9.1 )
If a tight nuchal cord is encountered, release the cord if possible; avoid clamping and cutting the cord
NEVER apply fundal pressure. This can further engage the anterior shoulder under the pubic bone
Implement maneuvers to alleviate shoulder dystocia. Move quickly between maneuvers and do not persist in any one maneuver if it is not immediately successful
Requires two assistants who each support a maternal leg and flex the thigh sharply against the abdomen
Causes cephalad displacement of the symphysis, flattens the sacral promontory, and improves pushing efficiency
Often recommended as initial or even prophylactic maneuver due to its low invasiveness
There is not an order for the other maneuvers. The preference is given to the experience of the operator.
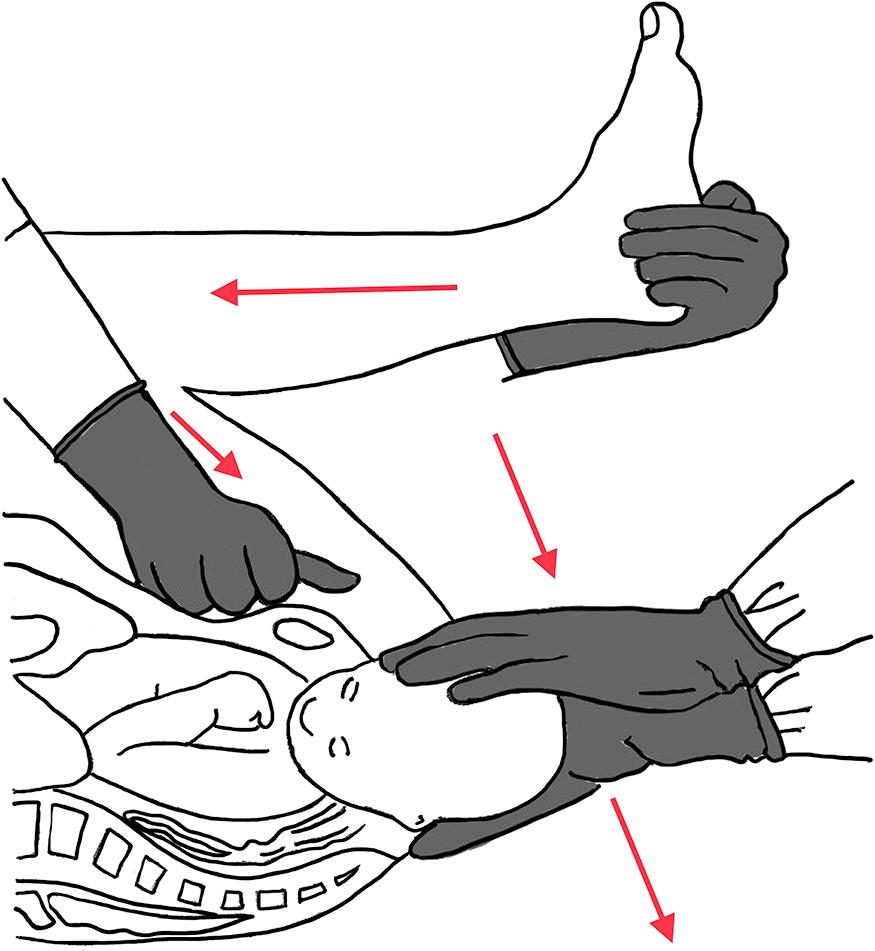
An assistant applies suprapubic pressure with his/her palm or fist. It is crucial that pressure is applied suprapubic, not fundal
Pressure is applied in a downward (below pubic bone) and lateral direction (toward the baby face or sternum) to decrease the bisacromial diameter and shift this diameter into an oblique position
This maneuver is performed simultaneously with McRoberts' maneuver ( Fig. 9.2 )
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here