Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Women who present for percutaneous coronary intervention (PCI) are generally older and have more comorbidities compared with men. Women and men have comparable short- and long-term outcomes with bare-metal stents (BMSs) and drug-eluting stents (DESs), including similar mortality rates after PCI. Adjunctive PCI devices such as directional coronary atherectomy and excimer laser atherectomy are associated with higher complication rates in women.
Women have higher rates of vascular complications and bleeding after PCI. Despite the potential benefits of transradial PCI and documented higher risks than men with femoral access, women are more likely to undergo transfemoral PCI, possibly based on presumed limiting technical challenges with transradial access.
Women who present with non–ST-elevation acute coronary syndromes (NSTE-ACS) are less likely to benefit from an early-invasive strategy when they have low-risk features (i.e., negative cardiac biomarkers), and risk stratification with noninvasive testing should be considered accordingly in these situations. However, women have a higher risk of several in-hospital and long-term complications after NSTE-ACS overall and derive similar benefits from guideline-based therapies as men. As such, these therapies should be applied irrespective of sex when women are not at explicitly low risk. Data suggest sex-difference disparities in the application of these therapies.
Women and men derive similar benefit from primary PCI for ST-elevation myocardial infarction (STEMI), but the short-term mortality after STEMI is higher among women.
Women and men derive similar benefit from adjuvant acute coronary syndrome (ACS) and post-PCI medical therapies including glycoprotein (GP) IIb/IIIa inhibitors, P2Y 12 inhibitors, and direct thrombin inhibitors.
Women are disproportionately affected by the unique syndromes of stress cardiomyopathy, spontaneous coronary artery dissection, and microvascular angina.
Race-specific analyses of PCI are limited. However, African-American patients who present for PCI are younger and are more likely to be women, have more comorbidities, and are more likely to present with an ACS.
Cardiovascular disease (CVD) remains the leading cause of death regardless of sex and race. Historically, data extrapolated from large studies and registries have been applied to all populations irrespective of sex, race, or ethnicity. However, a growing body of literature shows sex and race differences in CVD manifestations, outcomes, and treatment effects. This chapter will explore these pertinent differences within the context of interventional cardiology.
CVD is the leading cause of morbidity and mortality among women in the United States. It claims the lives of more women than the next five major causes of death combined. CVD typically manifests approximately 5 to 10 years later in women than in men, which has in part contributed to the misconception that CVD is predominately a disease affecting men. Although overall rates of death attributable to CVD have declined over the past several decades, increasing data show a slower rate of decline and worse overall outcomes in women after a cardiovascular event, which may be explained by differences in comorbidities and pathophysiology and disparities in treatment.
More than 1.3 million percutaneous coronary interventions (PCIs) are performed annually in the United States, with an estimated 35% performed in women. Compared with men, women undergoing PCI are 5 to 10 years older and have a higher prevalence of hypertension, hyperlipidemia, diabetes, and other comorbidities such as smoking. They are less likely to have a history of myocardial infarction (MI), PCI, or coronary artery bypass graft (CABG) surgery. Women are more likely to present with non–ST-elevation acute coronary syndromes (NSTE-ACS), whereas men are more likely to present with an ST-elevation MI (STEMI). Compared with men, women have similar lesion types but less multivessel disease and substantially smaller vessels. Despite a lower prevalence of left ventricular dysfunction at baseline, women tend to have a higher incidence of congestive heart failure (CHF) and cardiogenic shock, and they have more functional impairment after revascularization than do men.
Early reports of patients undergoing balloon angioplasty showed lower procedural success rates in women. In addition, early registry data found that women had higher in-hospital mortality after PCI even after adjusting for baseline comorbidities. However, more recent studies report similar procedural success rates in both groups, with an increase in the number of women undergoing PCI over the past several decades. Overall these studies demonstrate that both in-hospital and long-term mortality rates after PCI are similar between men and women despite women being older and having more complex lesion types ( Tables 9.1 and 9.2 ). This is likely due to heightened awareness of the effects of CVD on women, as well as advances within the field (i.e., newer-generation stents and balloons, smaller sheath sizes and catheters, and advances in adjunctive pharmacotherapies). Controversy has surrounded the previously documented, less frequent use of diagnostic catheterization and delays in PCI in women compared with men. These issues will be addressed further in the section on acute coronary syndromes (ACSs) later in the chapter.
| Study | Women/Men ( N ) | Women (%) | Men (%) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Peterson et al. | ||||
| In-hospital death | 35,571/74,137 | 1.8 | 1.0 | 1.07 (0.9–1.2) |
| In-hospital MI | 1.5 | 1.2 | 1.25 (1.1–1.4) | |
| Jacobs et al. | ||||
| In-hospital death | 895/1,629 | 2.2 | 1.3 | 1.6 (0.76–3.35) |
| In-hospital MI | 0.2 | 0.7 | ||
| Lansky et al. | ||||
| In-hospital death | 2,077/5,295 | 1.4 | 0.7 | 2.28 (1.15–4.55) |
| Watanabe et al. | ||||
| In-hospital death | 29,227/53,556 | 1.2 | 0.6 | 1.65 (1.33–2.04) |
| Malenka et al. | ||||
| In-hospital death | 3,983/8,057 | 1.04 | 0.79 | 1.24 (0.96–1.60) |
| In-hospital MI | 1.71 | 1.36 | 1.02 (0.85–1.24) | |
| Heer et al. | ||||
| In-hospital death | 24,262/65,972 | 0.3 | 0.2 | 1.07 (0.83–1.41) |
| In-hospital MACE | 24,262/65,972 | 0.7 | 0.4 | 1.37 (1.12–1.67) |
| Study | Women/Men ( N ) | Women (%) | Men (%) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Jacobs et al. | ||||
| 1-Year death | 895/1,629 | 6.5 | 4.3 | 1.26 (0.85–1.87) |
| 1-Year death/MI | 11.1 | 9.0 | 1.14 (0.86–1.50) | |
| Lansky et al. | ||||
| 1-Year death | 2,077/5,295 | 4.4 | 3.3 | No difference between sexes was noted; however, OR was not reported . |
| 1-Year MACE | 29.2 | 32.7 | ||
| Mehili et al. | ||||
| 1-Year death | 1,001/3,263 | 4.0 | 4.1 | 0.99 (0.54–1.13) |
| 1-Year MACE | 6.0 | 5.8 | — | |
| Chiu et al. | ||||
| 1-Year death | 5,301/12,738 | 7 | 5 | 1.14 (0.93–1.41) |
| 1-Year MACE | — | — | 1.05 (0.97–1.13) | |
| Kunadian et al. | ||||
| 1-Year death | 3,938/7,448 | 8.1 | 5.6 | 1.44 (1.38–1.50) |
| Bavishi et al. | ||||
| 1-Year death | 4,391/4,132 | 8.5 | 8.0 | 1.01 (0.93–1.11) |
No sex-based comparisons were made in the earlier randomized clinical trials comparing bare-metal stents (BMSs) with balloon angioplasty. Restenosis and revascularization rates were not well defined for women after bare-metal stenting because of the small sample of women in prospective trials with systematic angiographic follow-up. Even though women tend to have smaller vessel size, shorter lesions, and a higher prevalence of diabetes, some intriguing initial studies reported that women had similar or lower target-vessel revascularization (TVR) rates compared with their male counterparts after PCI. However, systematic angiographic and clinical follow-up has not validated these findings. In the drug-eluting stent (DES) era, both sirolimus and paclitaxel stents have shown favorable outcomes in women. The Sirolimus-Eluting Stent in De-Novo Native Coronary Lesions (SIRIUS) trial and the TAXUS IV trial demonstrated the superiority of DESs with reduction in restenosis, TVR, and major adverse cardiac events (MACEs) at 1-year follow-up in women and men. TAXUS IV randomized patients with severe coronary artery stenosis to DES (paclitaxel) versus BMS. Women accounted for 27.9% of the study population. Restenosis rates were similar in women and men treated with the TAXUS stent (7.6% vs. 8.6%, P = .80), as were measurements of late luminal loss (0.23 mm vs. 0.22 mm, P = .90). Compared with BMSs, women treated with the TAXUS stent had a significant reduction in 9-month restenosis (29.2% vs. 8.6%, P < .001) and 1-year target-lesion revascularization (TLR) rates (14.9% vs. 7.6%, P = .02). Of note, women had higher unadjusted TLR rates compared with men at 1 year; however, female sex was not an independent predictor of TLR (odds radio [OR], 1.72; 95% confidence interval [CI], 0.68 to 4.37; P = .25). A pooled analysis from four randomized sirolimus versus BMS trials was done to assess for sex differences. In 1748 patients, 497 of whom were women, sirolimus-eluting stents were associated with a significant reduction in the rates of in-segment binary restenosis in women (6.3% vs. 43.8%) as well as in men (6.4% vs. 35.6%), which resulted in significant reduction in 1-year MACE rates ( P < .0001). A pooled analysis of 11,557 women in 26 trials showed decreased mortality, MI, in-stent thrombosis, and TVR in those treated with a DES versus a BMS. In addition, a significant benefit was found with newer-generation over early-generation DESs, including a lower risk of stent thrombosis at 12 months. With respect to contemporary-generation, everolimus-eluting stents, women experience similar risk of 1-year MACEs (death, MI, TVR) but have higher adjusted risk of recurrent ischemic events related to nonstent-related MIs compared with men.
Few sex-based studies on the efficacy of coronary atherectomy and adjuvant devices exist. Although directional coronary atherectomy (DCA) is no longer used, from a historical perspective, it appears to have been associated with lower procedural success and more bleeding complications in women. Likewise, laser atherectomy with the excimer laser catheter was also associated with higher coronary perforation rates and increased morbidity in women. Despite this demonstration, newer atherectomy techniques such as orbital atherectomy have not shown an increased rate of in-hospital or 30-day MACEs compared with men, despite higher baseline risks such as smaller vessels and older age. Female sex is an independent risk factor for TVR after modern, coronary brachytherapy with beta radiation for resistant DES in-stent restenosis (ISR). Limited sex-specific data on rotational atherectomy, cutting or scoring balloon angioplasty, extraction atherectomy, or gamma brachytherapy are available. In smaller studies, sex has generally not been found to be an independent predictor of complications on the efficacy of these devices as a whole, although women have historically been underrepresented in earlier studies of adjuvant device therapies.
Women experience greater vascular and bleeding complications during PCI, particularly in the context of ACSs. Compared with men, they have an increased risk of major hematoma, retroperitoneal bleeding, bleeding that requires transfusion, and vascular injury that requires surgery after PCI. Much of this may be explained by smaller vessel size, lower body mass index, and differences in platelet biology, drug distribution, and bioavailability. With the development of weight-adjusted heparin dosing, introduction of smaller sheath sizes, and early sheath removal, vascular complications have decreased. However, even in the current era, women continue to have a 1.5 to 4 times higher risk of vascular complications compared with men. Table 9.3 shows different vascular complication rates by sex as reported in recently published large studies.
| Study | Women/Men ( N ) | Women (%) | Men (%) | P Value |
|---|---|---|---|---|
| Chiu et al. | ||||
| Blood transfusion | 5,301/12,738 | 12 | 4 | <0.001 |
| Major hematoma | 5 | 2 | <0.001 | |
| Pseudoaneurysm | 0.6 | 0.3 | 0.005 | |
| Lansky et al. | ||||
| Major hematoma | 562/1,520 | 2.5 | 1.5 | 0.005 |
| Retroperitoneal bleed | 0.5 | 0.2 | 0.05 | |
| Surgical repair | 3.8 | 2.4 | 0.001 | |
| Welty et al. | ||||
| Vascular injury | 2,101/3,888 | 1.6 | 0.6 | 0.001 |
| Peterson et al. | ||||
| Vascular injury | 35,571/74,137 | 5.4 | 2.7 | 0.001 |
Given that women have higher rates of vascular complications, they are seemingly ideal candidates for radial access. Data from the Study of Access Site for Enhancement of PCI for Women (SAFE-PCI) trial demonstrated significantly reduced bleeding and vascular complications in women undergoing cardiac catheterization or PCI with radial access as compared with femoral access (0.6% vs. 1.7%; OR 0.32; 95% CI, 0.12 to 0.90). However, this trial did not show significant differences when limited to women undergoing PCI alone. Of note was a significant access site crossover to the femoral approach, mostly as a result of radial artery spasm. In addition, in a subgroup analysis of the Radial Vs. femorAL access for coronary intervention (RIVAL) randomized trial, women undergoing coronary angiography and PCI had a significant reduction in major vascular complications when radial access was performed (3.1% vs. 6.1%; hazard ratio [HR] 0.5; 95% CI, 0.32 to 0.78; P = .002). Despite the potential benefits from radial access in women, observational retrospective data from the National Cardiovascular Data Registry (NCDR) CathPCI registry suggest that women are still less likely to undergo radial access than men, presumptively because of ongoing concern for technical challenges involving spasm and tortuosity. These data notably suggest similar procedural success rates among women undergoing transradial PCI.
Data are sparse on sex differences in vascular complications related to arterial vascular closure devices. However, subgroup analyses of a number of studies have shown that the odds of a vascular complication related to a closure device is 2 to 8 times higher in women than in men. Again, this is thought to be related to women’s smaller arterial luminal diameter.
Limited data exist on sex-based outcome differences for PCI by coronary lesion subsets as the primary trial and registry data for efficacy and safety of chronic total occlusions (CTOs), left main coronary disease (LM), and saphenous vein graft (SVG) interventions has historically underrepresented women. Older data indicated the possibility of higher MACEs in women undergoing PCI for CTOs, but these data were acquired between 1998 and 2007, after which techniques and understanding of CTO-PCI improved considerably. More recent retrospective, single-center data demonstrate no discernable differences in procedural success and complication rates. Men are much more likely to undergo CTO-PCI in published data. Data on unprotected LM PCI of 2328 patients from the IRIS-MAIN registry demonstrated that ostial left main and ACS presentations of LM disease were more common in women, and that subsequent TVR was significantly higher in women than men (8.8% vs. 5.7%, P < .05). Women and men had similar frequency of the composite primary end point of all-cause death, MI, or cerebrovascular accident. Sex appears to be a significant predictor of outcomes after SVG PCI. Women have higher 30-day cumulative mortality compared with men (4.4% vs. 1.9%, P = .02) but with notably higher incidence of vascular complications and postprocedural acute renal failure that may drive some of this effect.
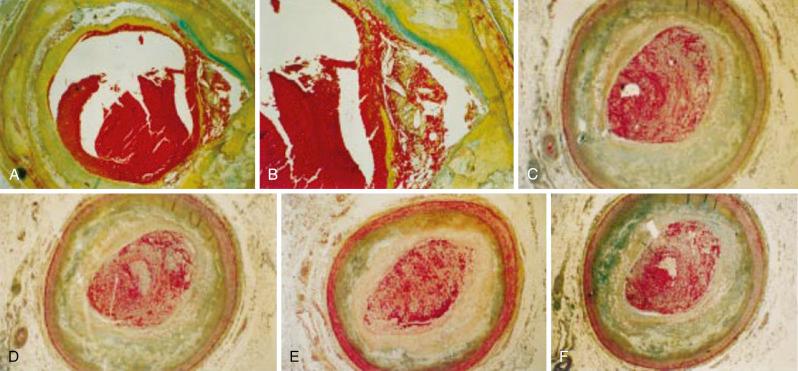
It is well known that the presentation, pathophysiology, diagnosis, treatment, and outcomes of ACSs differ among men and women. Although women usually present with typical symptoms of ACS, the frequency of atypical presentations of ACS is increased as compared with men. Women typically have higher Killip class and longer prehospital delays when presenting with ACS. Women with suspected ACS are less likely than men to have obstructive or extensive epicardial coronary artery disease (CAD) and are more likely to have either a noncardiac cause or cardiac causes other than obstructive epicardial CAD. Despite this, women with NSTE-ACS with no apparent obstructive epicardial disease still have a 2% 30-day mortality. In fact, women of all ages have higher rates of in-hospital and long-term complications after NSTE-ACS than men including heart failure, cardiogenic shock, acute renal failure, recurrent MI, stroke, readmissions, and bleeding and vascular complications. Data from more than 450,000 patients in the British Cardiovascular Intervention Society (BCIS) and Swedish Coronary Angiography and Angioplasty Registry (SCAAR) between 2007 and 2011 demonstrate significantly higher 30-day and 1-year mortality rates in women compared with men for both non–ST-elevation MI (NSTEMI) and STEMI. After multivariate regression, female sex was an independent predictor of all-cause mortality at 30 days and 1 year. Further large registry data indicate higher in-hospital mortality for women with STEMI but not NSTEMI. Women are also more likely to report preindex psychiatric symptoms including anxiety and depression. Of pathobiologic interest, women who present with NSTE-ACS are more likely to have elevated C-reactive protein (CRP) and brain natriuretic peptide (BNP), whereas men are more likely to have elevated creatine kinase MB (CK-MB) and troponin. Surprisingly, sex differences are apparent in acute MI plaque morphology as well. Autopsies reveal more plaque erosion than plaque rupture in women after fatal MI compared with men ( Fig. 9.1A and B ). In addition, women appear to have more distal microvascular embolization compared with men during fatal MI.
Women who present with an MI are less likely to undergo primary angioplasty within 90 minutes or to receive pharmacologic treatment on admission and are also less likely to be on evidence-based secondary prevention medical treatment upon discharge. In numerous publications, median prehospital delays ranged from 1.8 to 7.2 hours for women versus 1.4 to 3.5 hours in men. In the HORIZONS-AMI trial, symptom-onset-to-balloon time was longer, but this delay was largely driven by late arrival at the hospital. Delays are partly due to the higher frequency of atypical presentations. Overall, women monitored by the National Registry of Myocardial Infarction (NRMI) were more likely than men to present without chest pain, particularly if younger. Women aged younger than 45 years were 30% more likely to present without chest pain than men of similar age. This is an important discrepancy because the nature of presentation for ACS also prompts downstream diagnostic testing such as electrocardiographic (ECG) and biomarker testing, and the lack of symptoms may contribute to delays in diagnostic clarification even when women present to the hospital earlier in their course. Importantly, in studies of the most recent, high-sensitivity troponin assays, which improve diagnosis in both men and women, establishing sex-dependent thresholds doubles the diagnosis of MI in women without affecting the diagnosis rates in men. Women diagnosed by these sex-specific thresholds were notably at a higher risk for death or recurrent MI at 12 months in the same study. .
In 2005, the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the American College of Cardiology/American Heart Association Guidelines (CRUSADE) investigators published data on sex differences in patients with NSTEMI from a large registry of more than 35,000 patients, of which 41% were women. They found that women were less likely to receive guideline-based therapies such as heparin (adjusted OR, 0.91; 95% CI, 0.86 to 0.97) at presentation. Moreover, women were less likely to undergo diagnostic left heart catheterization (adjusted OR, 0.86; 95% CI, 0.82 to 0.91) or PCI (adjusted OR, 0.91; 95% CI, 0.86 to 0.96). The CRUSADE registry confirms the unfortunate presence of continued treatment disparities between men and women. Another study that used the American College of Cardiology (ACC) NCDR looked at sex differences among patients with ACS (both NSTEMI and STEMI) and again showed disparities in treatment. Of 199,690 patients, despite fewer high-risk criteria, the 55,691 women had greater in-hospital complications. For example, although the adjusted mortality among women and men was similar (OR, 0.97; 95% CI, 0.88 to 1.07; P = .52), women had higher rates of CHF (OR, 0.80; 95% CI, 0.69 to 0.92; P = .002), bleeding (OR, 0.55; 95% CI, 0.52 to 0.58; P < .01), and cardiogenic shock (OR, 0.82; 95% CI, 0.75 to 0.89; P < .01). Moreover, they found that women were less likely to receive aspirin (OR, 1.16; 95% CI, 1.13 to 1.20; P < .01) at admission and were less likely to be discharged on statins (OR, 1.10; 95% CI, 1.07 to 1.13; P < .01) or aspirin (OR, 1.17; 95% CI, 1.13 to 1.21; P < .01). Older age of female patients, symptom differences, and delay in presentation after acute MI have been suggested as possible explanations. Although these factors may explain initial treatment differences, they do not explain treatment disparities once the diagnosis has been made. These findings call for significant improvements in the care of ACS patients and highlight the importance of continued investigations into perceptual barriers that contribute to these differences.
Numerous randomized trials have shown the benefit of an invasive strategy over conservative (“ischemia-guided”) treatment in NSTE-ACS; however, the benefits for women in previous subgroup analyses have been less certain, and controversy exits over sex differences in revascularization benefits. A meta-analysis of eight large ACS trials that included 3075 women and 7075 men found that, similar to men, an invasive strategy was safe and effective in terms of the composite end point of death, MI, or rehospitalization (OR, 0.67; 95% CI, 0.50 to 0.88) in women who had positive biomarkers. However, in women with negative biomarkers (unstable angina), an invasive strategy was associated with a trend toward higher rates of death and MI (OR, 1.35; 95% CI, 0.78 to 2.35; P = .08), suggesting potential harm. A more recent study of 46,455 patients in the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) registry, which included 14,819 women—all of whom presented with NSTEMI and had positive biomarkers—showed a marked mortality reduction for both men and women treated with an invasive versus a noninvasive strategy (relative risk [RR], 0.46; 95% CI, 0.38 to 0.55). However, a study of 184 women from the Fifth Organization to Assess Strategies in Acute Ischemic Syndromes (OASIS-5) trial randomized to a routine invasive strategy versus a selective invasive strategy—defined as catheterization for patients with refractory ischemia, hemodynamic instability, or new ST elevations—showed no difference in the rates of death, MI, or stroke (HR, 1.46; 95% CI, 0.73 to 2.94). A meta-analysis of 2692 women, which included this study group, showed no significant difference in the composite outcome of death or MI (OR, 1.18; 95% CI, 0.92 to 1.53) between the two treatment groups and demonstrated a trend toward higher mortality in those who received a routine invasive strategy (OR, 1.51; 95% CI, 1.00 to 2.29). Overall, the 2014 ACC/American Heart Association (AHA) guidelines on NSTE-ACS specifically outline recommendations for women with NSTE-ACS and notably give a class III recommendation for an early-invasive approach in low-risk women (i.e., those with negative biomarkers) because of the lack of benefit and the possibility of harm. Given the previously summarized data, the guidelines now specifically mention that women with NSTE-ACS should otherwise be managed with the same pharmacologic therapy as men and that women with high-risk features (i.e., positive troponin) should undergo an early invasive strategy (class I recommendations).
The overall superiority of primary PCI (PPCI) over fibrinolytic therapy for women presenting with a STEMI has been demonstrated. In fact, because of higher baseline comorbidities in women at presentation, the absolute benefit with PPCI is greater for women than for men. An estimated 56 deaths are prevented for every 1000 women treated with PPCI compared with 42 deaths per 1000 men. Sex-associated differences are also apparent in the amount of myocardial salvage after PPCI for STEMI, with greater salvage in women than in men. This may be attributed to sex-specific tolerance of hypoxia demonstrated in a number of basic science experiments. From a historical perspective, sex-specific data regarding primary stenting versus primary balloon angioplasty in STEMI are also available. Women who presented with a STEMI benefitted from primary stenting with less reinfarction, TVR, and TLR. The Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial randomized 2082 patients, of whom 27% were women, to BMS versus primary balloon angioplasty with or without a glycoprotein (GP) IIb/IIIa inhibitor and found superior efficacy and safety with primary stenting, with or without abciximab, compared with balloon angioplasty. In women, primary stenting resulted in a reduction in the 1-year composite of death, reinfarction, ischemia-driven TVR, or disabling stroke from 28.1% to 19.1% ( P = .01) compared with percutaneous transluminal coronary angioplasty (PTCA) alone.
Much controversy surrounds potential differences in mortality rates between women and men after STEMI ( Table 9.4 ). A higher in-hospital mortality is apparent among women undergoing PCI for STEMI compared with men. This is in contrast to NSTE-ACS, in which mortality differences are less apparent after adjusting for other factors. A large meta-analysis of 48 studies involving more than 100,000 patients undergoing PPCI for STEMI demonstrated significantly higher adjusted in-hospital and 30-day mortality in women compared with men at (RR 1.31, 95% CI, 1.08 to 1.65 and RR 1.19, 95% CI, 1.01 to 1.39, respectively). There was no difference in long-term mortality after adjustment. A large study that used the Nationwide Inpatient Sample of 11,717 women and 24,028 men found a 5.2% in-hospital mortality rate in women compared with a 2.7% mortality rate in men. Even after adjusting for age, hypertension, institutional volume, and pulmonary disease, women had higher mortality (OR, 1.47; 95% CI, 1.23 to 1.75). This has been replicated in a number of other studies. However, no difference in mortality rates is apparent between the two groups at 30 days or 1 year (see Table 9.4 ). Of note, female sex is an independent risk factor for the development of cardiogenic shock as a complication of MI; however, no sex difference in mortality is apparent for patients with cardiogenic shock after adjustment for age. Thus the ACC/AHA STEMI guidelines recommend PCI or CABG for patients younger than 75 years who are in cardiogenic shock and have lesions amenable to revascularization regardless of sex.
| PCI-MI Studies | Women/Men ( N ) | Women (%) | Men (%) | Adjusted Rates OR (95% CI) |
|---|---|---|---|---|
| Watanabe et al. | ||||
| In-hospital death | 11,717/ 24,028 | 5.2 | 2.7 | 1.47 (1.23–1.75) |
| Vakili et al. | ||||
| In-hospital death | 317/727 | 7.9 | 2.3 | 2.69 (1.4–5.2) |
| Mehili et al. | ||||
| 30-Day death | 502/1,435 | 8.4 | 8.5 | — |
| 1-Year death | 13.8 | 12.9 | 0.65 (0.49–0.87) | |
| Lansky et al. | ||||
| 30-Day death | 562/1,520 | 4.6 | 1.1 | — |
| 1-Year death | 7.6 | 3.0 | 1.11 (0.53–2.36) | |
| Kunadian et al. | ||||
| 30-Day death | 1,861/3,482 | 3.8 | 2.6 | 1.46 (1.38–1.54) |
| 1-Year death | 3,938/7,448 | 8.1 | 5.6 | 1.44 (1.38–1.50) |
| Bavishi et al. | ||||
| 30-Day death | 3,072/1,861 | 7.1 | 4.3 | 1.19 (1.01–1.39) |
| 1-Year death | 4,391/4,132 | 8.5 | 8.0 | 1.01 (0.93–1.11) |
| Heer et al. | ||||
| In-hospital death (STEMI) | 9,156/23,830 | 6.3 | 3.6 | 1.19 (1.06–1.33) |
| In-hospital MACE (STEMI) | 9,156/23,830 | 6.6 | 3.8 | 1.19 (1.07–1.34) |
| In-hospital death (NSTEMI) | 14,336/33,879 | 2.4 | 1.8 | 1.02 (0.89–1.16) |
| In-hospital MACE (NSTEMI) | 14,336/33,879 | 2.7 | 2.0 | 1.04 (0.91–1.18) |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here