Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In the late 1920s, Edgar Adrian conducted a series of experiments showing that nerves carry critical information via electrical impulses to and from the brain, which dramatically changed how the human nervous system was viewed ( ). This led to him and Charles Sherrington winning the Nobel Prize in 1932. One particular experiment Adrian conducted had exemplified this idea in a profound way. Adrian had recorded and amplified electrical signals from a toad’s retina, and later commented, “I had arranged electrodes on the optic nerve of a toad in connection with some experiments on the retina. The room was nearly dark and I was puzzled to hear repeated noises in the loudspeaker attached to the amplifier, noises indicating that a great deal of impulse activity was going on. It was not until I compared the noises with my own movements around the room that I realised I was in the field of vision of the toad’s eye and that it was signaling what I was doing.” Adrian’s series of landmark experiments showed that the nerves in our bodies form a vast network, rich with information, which is crucial to our survival.
Today we know that nerves not only carry critical information related to our five senses, but also carry information to and from our organs. Tapping into and deciphering signals traveling within this network, known as neural decoding, is showing promise in “closing-the-loop” to create new responsive neuromodulation approaches and bioelectronic devices for areas including Parkinson’s disease, epilepsy, obesity, blindness, movement restoration in paralysis, and many others. Furthermore, monitoring and decoding hidden messages within the human nervous system through noninvasive and invasive methods may lead to new, powerful diagnostic methods for a wide variety of chronic diseases and injuries in the future. This opens the door to an exciting new array of possibilities for the fields of neuromodulation and bioelectronic medicine.
Before, and in parallel to, the work in neural decoding, “open-loop” neuromodulation methods have been used and studied in a variety of clinical applications. These open-loop devices lack sensing capabilities and therefore have no feedback signal available to make automatic stimulation adjustments. However, successful studies have targeted indications such as rheumatoid arthritis ( ), Crohn’s disease ( ), chronic pain ( ), Parkinson’s disease ( ), obsessive compulsive disorder and depression ( ), Alzheimer’s disease ( ), and the treatment of high blood pressure ( ). In these studies, neurostimulation patterns were set manually and no feedback was provided to “close-the-loop.” As neural sensing and neural decoding methods were developed, the idea of closed-loop, or responsive, stimulation began to emerge. Responsive stimulation has the advantages of improved efficacy and reduced power consumption, thereby extending battery life, which can be particularly important in implantable devices.
In a closed-loop, or more generally, responsive stimulation device, the main functions are sensing, decoding/processing, and stimulation. The sensing may be electrical in form, detecting signals from the nervous system through various types of electrodes. Decoding often involves advanced signal processing techniques to first convert the signals into a useful form or extract “features” that can be used to automatically adjust the stimulation or inform the selection of stimulation parameters. Finally, the stimulation function may involve electrical methods or other methods such as optogenetics ( ) to stimulate or modulate the neural pathways of interest in the brain or elsewhere in the nervous system.
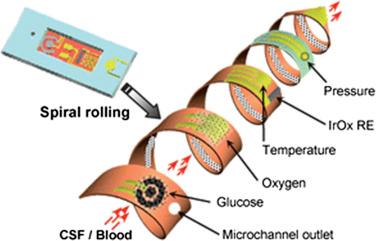
The sensing function in a responsive stimulation device can involve electrical methods or employ the use of a biosensor that detects chemical or other processes. Sensing electrically involves different types of electrodes such as noninvasive types including electroencephalogram (EEG) electrodes or can involve microelectrodes that are often implanted surgically ( ). These can be used for BCI (brain–computer interface) applications to restore lost function sustained from stroke, amyotrophic lateral sclerosis (ALS), or spinal cord injury, for example. Various biosensors can also be used to provide useful feedback in a neuromodulation device. These include multimodal sensors for traumatic brain injury patients that can measure multiple parameters in the brain including pressure, temperature, oxygen, and glucose, as shown in Fig. 131.1 ( ). Fiber optic-based sensors with a bioactive component (e.g., enzyme-based) are also used to detect various chemicals of interest in the body ( ) and can be used as feedback as well. Finally, neurotransmitter levels, such as dopamine, can be estimated in the brain through the use of fast-cyclic voltammetry techniques ( ). These various modalities of sensing can provide valuable feedback for responsive stimulation.
Once a sensing strategy has been determined, various signal processing and neural decoding methods can be used to find and classify patterns in the measured signals. Machine-learning methods such as linear discriminant analysis and support vector machine (SVM) methods can be used to automatically classify neural signals (typically after an initial training period). Advanced techniques such as L1-SVM can also be utilized to exclude signals that are not useful as inputs for classification ( ) and has been used in real-time BCI applications ( ). Nonlinear methods such as the kernel method can be used as well to transform the input features into high-dimensional space to accommodate multiple neural modulation patterns for a similar condition ( ). Nonlinear methods often help increase the robustness and accuracy of a decoder, or classification algorithm ( ).
Integrating the sensing and neural decoding algorithms and then linking to an output completes the responsive stimulation device. Research has been conducted in multiple areas demonstrating the power of responsive stimulation. This type of stimulation has been studied in epilepsy, where subdural electrodes were used to detect neural activity electrically, which thereby triggered stimulation with the goal of reducing the severity and occurrence rate of seizures ( ). In another example of responsive stimulation, a biosensor that measures a neurotransmitter, dopamine in this case, was used to provide feedback information in a closed-loop DBS device for Parkinson’s disease ( ).
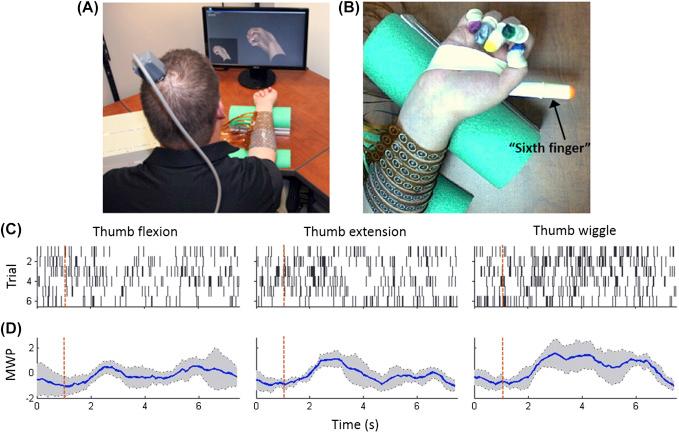
Another important use of responsive stimulation is in the area of restoring movement after an injury such as spinal cord injury. By recording and decoding information from the motor area of the brain, information about movement intent can be extracted and linked to neuromuscular stimulation, thereby restoring volitional movement. In a first-in-human demonstration of this type of responsive stimulation using a cortical electrode implant, a 24-year-old male quadriplegic study participant was able to achieve functional hand movement ( ). In this study, an electronic “neural bypass” was used to record, decode, and reroute signals around the participant’s spinal cord injury. In related, subsequent work, the participant was able to voluntarily switch between discrete (sustained) flexion/extension and rhythmic movement of a digit in the hand ( ). See Fig. 131.2 .
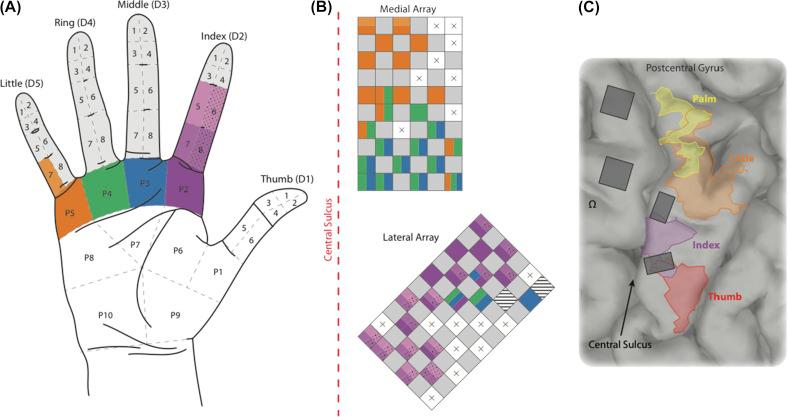
Another area where responsive stimulation is showing significant promise is in restoring the sense of touch. This is a case where the input driving the stimulation is not neural in nature, but rather from touch sensors on a prosthetic arm. In one study, the stimulation was applied to multicontact electrodes placed around forearm nerves and resulted in tingling and touch sensations in multiple hand locations for various stimulation patterns driven by tactile sensors in a prosthetic arm ( ). In another study, tactile sensors were also used in a prosthetic hand, but were used to drive microstimulation in somatosensory cortex resulting in tactile sensations in a long-term spinal cord injury participant ( ). See Fig. 131.3 for hand/finger locations where tactile sensations were perceived.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here