Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Segmental mandibulectomy involves the removal of a full-thickness segment of the mandible, often secondary to a malignant or benign tumor, trauma, or osteoradionecrosis. Segmental mandibulectomy may be performed in the setting of a composite resection, a term coined by Ward and Robben in 1951. It was thought that cancer of the oral cavity had a propensity to spread via periosteal lymphatics to the mandible; thus resection of a segment of mandible in continuity with a cancer of the oral cavity, oropharynx, or a primary cancer of the alveolar ridge was recommended regardless of whether the bone was actually invaded. Marchetta and colleagues disproved the theory of lymphatic invasion; thus mandibulectomy ( Table 182.1 ) is reserved for those with advanced cancer of the oral cavity or oropharynx where invasion of the mandible is clinically evident or cannot be ruled out. Fundamental concepts of extirpation have not changed in the interval. However, methods of reconstruction continue to evolve with the development of microsurgical techniques and reliable free flaps.
| Mandibulotomy | Osteotomy of the mandible to permit exposure, no bone resected; bone is reapproximated at the completion of the procedure |
| Marginal mandibulectomy | A portion of the mandible, typically the alveolus or lingual plate, is resected while leaving the continuity of the mandible intact. |
| Segmental mandibulectomy | A portion of the mandible is resected, with disruption of condyle-to-condyle continuity.
|
Most patients must undergo a tracheostomy, because postoperative oral disability could otherwise result in aspiration, and edema may lead to airway obstruction.
Mandibulectomy results in significant cosmetic and functional compromise and should be undertaken only if the operating surgeon feels that negative margins can be obtained.
The periosteum and mandible serve as barriers to invasion; however, patients who have undergone radiation, have had surgery that resulted in periosteal stripping/resection, or have poor peridontal health are at greater risk.
Cancers generally arise at the occlusal surfaces, but they can also invade at the muscular attachments or through invasion of the mental/inferior alveolar nerve.
Defects after segmental resection of the mandible can be divided into anterior and lateral defects in reference to the mental foramen.
An anterior defect results in loss of function of the oral cavity, including mastication, oral competence, drooling, swallowing ability, and airway compromise.
A lateral defect results in less morbidity; however, they include imbalance of mastication forces and altered contour of the posterior lower third of the face. The mandible will deviate toward the resected side due to the pull of the suprahyoid muscles on the residual fragment, causing inferior displacement and rotation around the remaining condyle.
Free flap reconstruction offers a high degree of reliability and good aesthetic outcomes.
Decisions regarding reconstruction should be based on the patient’s age, dentition, and expectations as well as on the anticipated soft tissue defect.
Plans for reconstruction of the mandible must be finalized before the mandibulectomy procedure. Various techniques are listed in Table 182.2 .
|
A simulated virtual surgical plan may be helpful.
Comorbidities and lifestyle habits that would affect the healing process
Postoperative swallow, speech, and dental rehabilitation
Approximately 25% of all head and neck cancers and 60% of all oropharyngeal cancers are positive for human papillomavirus (HPV), a finding that may alter postoperative treatment.
We have found varying association of mandibular invasion with inferior alveolar nerve paresthesia, loose teeth, gender, age, habits (alcohol, tobacco chewing), clinical type of lesion, skin fixation by the tumor, dental status, and patients with recurrent cancers who have received prior radiotherapy.
Routine preoperative examination of the head and neck with attention to the relationship of the primary cancer to the mandible using bimanual palpation to evaluate for adherence of the cancer to the periosteum or bone invasion.
Preoperative determination of the presence or extent of invasion of the mandible is challenging.
Testing for numbness of the lower lip to ascertain whether the cancer has involved the mental nerve
Clinical examination has been found to be a sensitive way to identify bone invasion; however, the best results can be obtained by combining it with a radiologic study.
No imaging technique is 100% accurate in identifying invasion of the mandible.
More than 60% to 70% of bone mineral must be lost before radiographic changes become evident.
Computed tomography (CT) scans, magnetic resonance imaging (MRI), and bone scintigraphy have been reported to have sensitivity and specificity ranging from 85% to 95%.
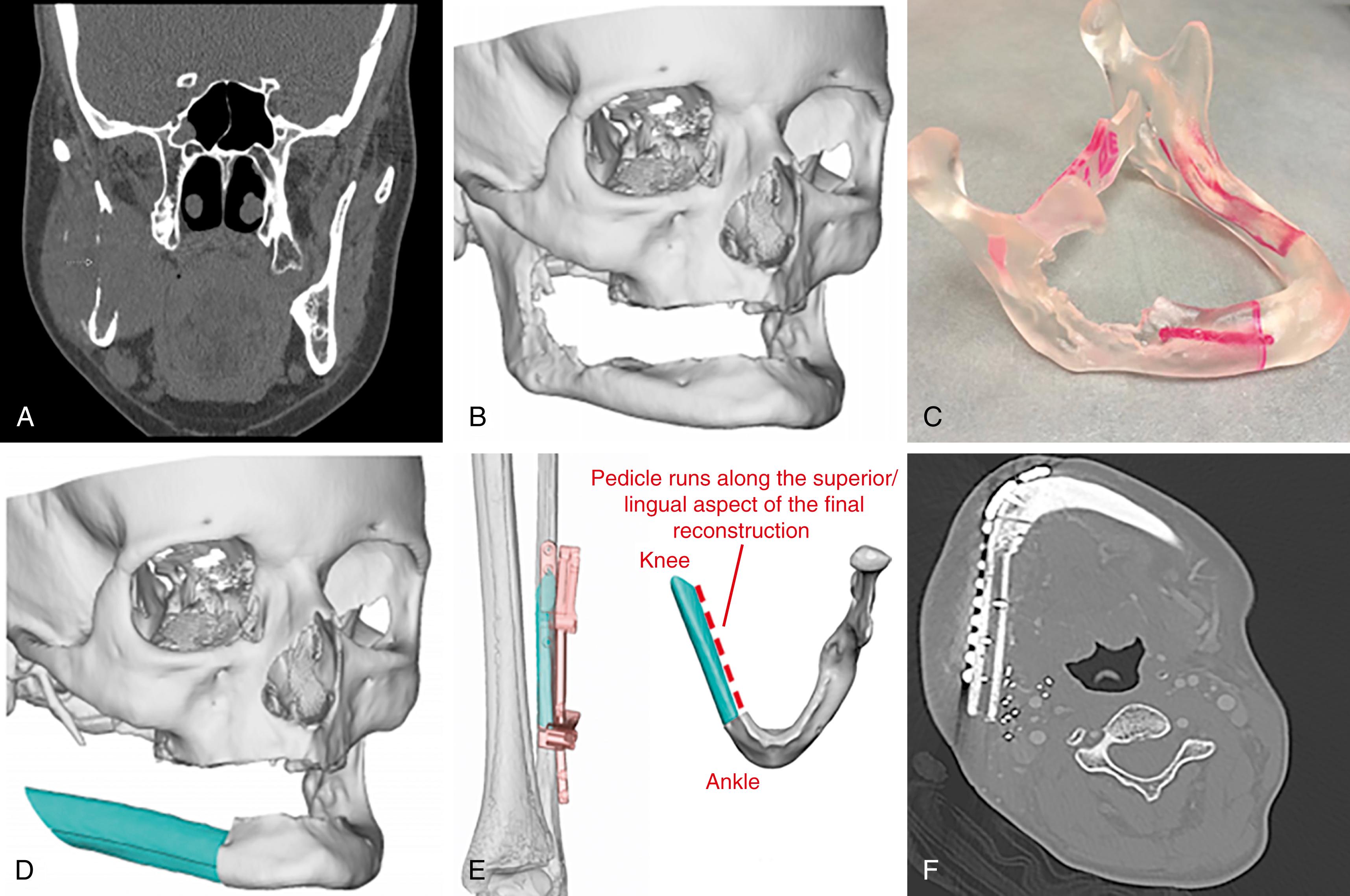
CT findings of osseous involvement include cortical erosion adjacent to the primary lesion ( Fig.182.1A ), aggressive periosteal reaction, abnormal attenuation in bone marrow, and pathologic fractures. Image quality around the alveolar crest may be hampered by severe dental artifacts and image noise.
MRI may be more sensitive for marrow and the inferior alveolar canal; however, it also results in more false positives and frequently overestimates the extent of tumor invasion. This is due to the high intensity of the edematous or inflammatory changes at the soft tissues adjacent to the tumor.
Positron-emission tomography (PET) with fluorine 18 fluorodeoxyglucose (FDG) is also expected to be useful for assessing bone invasion because FDG accumulates well at the malignant tumor.
For patients undergoing free flap reconstruction, conventional angiography or MR angiography is recommended for patients over 50 years of age and those with comorbidities such as diabetes mellitus (DM), hypertension, trauma, arteriopathy, or equivocal pulses.
Three-dimensional (3-D) imaging for reconstruction plans and 3-D modeling have greatly improved preoperative surgical planning (see Fig. 182.1 ).
Malignant tumor invasion of the medullary space of the mandible by either a primary tumor of the alveolar ridge or from an adjacent site such as the floor of the mouth
A hypoplastic, edentulous, or previously radiated mandible that precludes safe performance of a marginal mandibulectomy
Benign tumor of the jaw, such that extirpation would result in instability and possible pathologic fracture
Advanced osteonecrosis related to radiation or bisphosphonate use or osteomyelitis
Severe mandibular trauma with unstable or devitalized bone
Comorbidities for general anesthesia; cardiac, hemodynamic, nonreversible coagulopathic disorder
Extensive tumor that precludes complete resection
Distant metastases (a palliative mandibulectomy may be indicated in highly selected patients)
Discussion of patient expectations and possible outcomes, including expected sequelae and unexpected complications
Functional and cosmetic outcomes, especially in those patients who have had prior radiation therapy
Planned incision sites, tracheostomy for airway management, possible gastrostomy tube for alimentation
Multispecialty approach, as patient will likely require postoperative therapy
Dental, radiation, and medical oncology, speech/swallow
Coordination with teams involved
Reconstructive team: appropriate preparation, setup, instrument availability, reconstructive plan, and possible grafts or pedicle flaps
Dental/Oromaxillofacial Surgery: extractions, primary osseointegrated fixation devices
General surgery: gastrostomy tube placement for postoperative alimentation
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here