Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Grading of mitral regurgitation (MR) severity by echocardiography should not be based on visual inspection of the color Doppler MR jet, but rather on integration of multiple qualitative and quantitative parameters.
Secondary MR is dynamic, changing during systole in a biphasic pattern, and often varying dramatically with changes in loading conditions.
Any degree of secondary MR is associated with an adverse prognosis; however, LV size and function are also worse with worsened degrees of secondary MR.
Treatment of secondary MR begins with optimally tolerated doses of guideline-directed medical therapy for heart failure and/or left ventricular dysfunction. Cardiac resynchronization therapy and coronary revascularization should be performed when indicated.
Mitral valve surgery (replacement or repair) may be considered in selected patients with secondary MR but has not be shown to improve outcomes.
In randomized clinical trials, transcatheter mitral valve repair with the MitraClip device has been shown to reduce heart failure hospitalization and mortality in patients with secondary MR and LV EF between 20% to 50%.
Primary mitral regurgitation (MR) is caused by a lesion of the mitral valve leaflets, such as mitral valve prolapse, flail leaflet, endocarditis, rheumatic heart disease, radiation-induced heart disease, or various inflammatory conditions. Secondary MR, also known as functional MR (FMR), occurs when normal or nearly normal mitral leaflets are prevented from adequate coaptation by underlying left ventricular (LV) dysfunction or mitral annular dilation or both. Most cases of secondary MR are caused by chronic ischemic or nonischemic cardiomyopathy, but it occasionally results from pure annular dilation in chronic atrial fibrillation or restrictive cardiomyopathy. The term ischemic mitral regurgitation is often used to describe MR that occurs in chronic ischemic cardiomyopathy due to LV remodeling, although it can also refer to transient and reversible MR occurring during acute myocardial ischemia.
Acute MR due to papillary muscle rupture as a complication of acute myocardial infarction (MI) is not covered. This chapter focuses on the epidemiology, mechanism, prognostic implications, and treatment of chronic FMR in ischemic and nonischemic cardiomyopathies.
MR is the most common form of valvular heart disease; the incidence is less than 1% before age 55 years but increases with each decade to more than 9% after age 75 years. These estimates were based on an analysis of pooled data from three large epidemiologic studies and the Olmstead County database, in which moderate or severe MR was reported from qualitative echocardiographic grading. The study did not distinguish between moderate and severe MR, nor did it differentiate primary from secondary MR. A subsequent meta-analysis attempted to examine the prevalence of MR in the U.S. population using the Carpentier classification of leaflet motion to determine mechanism. The study authors estimated that MR affected 2 to 2.5 million people in the United States in the year 2000. The most common underlying mechanism was restricted motion of the leaflets only during systole (i.e., Carpentier class IIIb), which is the classic condition for FMR. The prevalence of FMR due to ischemic cardiomyopathy was estimated at 7500 to 9000 cases per 1 million people, and that of FMR due to nonischemic LV dysfunction was 16,250 cases per 1 million.
Although FMR is common, most cases are mild or moderate in severity. For example, in the Surgical Treatment of Ischemic Heart Failure (STICH) trial, an independent echocardiography core laboratory adjudicated the severity of FMR in ischemic cardiomyopathy as none in 27%, mild in 47%, moderate in 17%, and severe (grade 3+ or 4+) in 9% of 1852 patients with interpretable studies. Moderate or severe MR seems to occur in roughly one fourth of patients with cardiomyopathy.
The mitral apparatus consists of the leaflets, annulus, chordae tendineae, and papillary muscles with their supporting LV myocardium. Normal mitral valve closure is achieved by proper balance between closing forces that push the valve leaflets together during systole and tethering forces that prevent the valve from prolapsing into the left atrium (LA) ( Fig. 18.1 ). The mechanisms underlying FMR were eloquently reviewed by Levine and Schwammenthal. Closing forces are exerted on the mitral leaflets by systolic contraction of the LV myocardium and the mitral annulus. These forces are counterbalanced by the tethering forces exerted by the papillary muscles with their chordal attachments to the leaflets. In the normally shaped LV, the papillary muscles and chordae tendineae exert a vertical force on the leaflets, bringing them together during isovolumic contraction and preventing them from prolapsing into the LA during ejection. Spherical LV geometry due to remodeling causes the papillary muscles to migrate laterally and apically; as a result, they can no longer exert a vertical force during systole, leading to FMR.
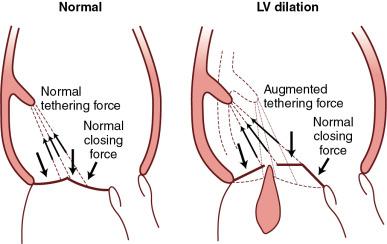
Because wall motion abnormalities may be regional rather than global, tethering forces are often asymmetric. For example, inferoposterior wall motion abnormalities commonly tether the posteromedial scallop (P3 segment) of the posterior leaflet and lead to asymmetric dilation of the annulus on its medial aspect. In addition to an imbalance between closing forces and tethering forces, annular dilation, flattening of the annulus, and loss of systolic annular contraction may contribute to FMR. In some patients, LV dyssynchrony leads to discoordinated myocardial contraction that further distorts the balance between closing and tethering forces, resulting in a loss of normal mitral leaflet coaptation and competence.
Despite the obvious fact that closing forces and tethering forces are abnormal in virtually all patients with chronic ischemic or nonischemic cardiomyopathy, many of these patients do not have FMR or have only mild FMR. The most obvious explanation is that the reduction in closing force and the increase in tethering force may be balanced so that MR remains absent or mild. Another reason is the potential for mitral leaflet tissue to expand over time, allowing more leaflet surface for coaptation. In patients with chronic severe aortic regurgitation, who have very dilated LV chambers with leaflet tethering, the mitral leaflet surface is 30% larger than normal, and FMR is uncommon. FMR may not simply be a disease of the LV but may also involve inadequate compensatory mitral leaflet enlargement due to lack of time for compensatory enlargement to occur (e.g., MR after MI) or to biologic abnormalities (e.g., advanced age, diabetes, genetic factors).
During percutaneous coronary intervention (PCI), acute myocardial ischemia induced by balloon inflation causes prompt segmental myocardial dyskinesis, which reverses on balloon deflation. Relief of ischemia by PCI has been shown to reduce or eliminate acute ischemic MR. In the setting of acute MI, a significant wall motion abnormality may lead to FMR, particularly with inferoposterior MI. Although this represents true ischemic MR, that term is most often used to refer to MR in the setting of chronic ischemic heart disease with LV dilation and dysfunction.
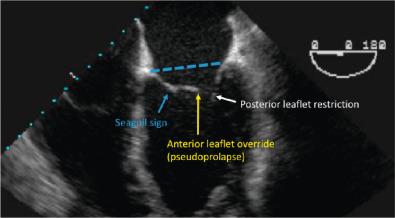
The mechanism of MR can vary, depending in part on the distribution of coronary artery disease (CAD). Right coronary disease typically leads to an inferoposterior wall motion abnormality, often with normal or only mildly reduced left ventricular ejection fraction (LVEF). On echocardiography, the posterior leaflet, particularly the posteromedial scallop, appears to be restricted, whereas the anterior leaflet appears to override the posterior leaflet without rising above the annulus plane (i.e., pseudoprolapse) ( Fig. 18.2 ). The mid-anterior leaflet may be tented by tension on strut chords, resulting in the so-called seagull sign (see Fig. 18.2 ). In anterior MI, FMR often results from spherical LV remodeling with reduced LVEF. The alterations in LV geometry change the papillary muscle position and the direction of tension exerted on mitral leaflets.
Contrary to traditional teaching, isolated infarction of the papillary muscles does not cause FMR. Rather, it is displacement of the papillary muscles by the underlying myocardium that increases tethering forces and results in ischemic FMR. This can occur with wall motion abnormalities in any myocardial territory or with global LV remodeling in ischemic heart disease.
MR is common in all forms of nonischemic cardiomyopathy, including dilated, hypertrophic, and restrictive cardiomyopathy. In dilated cardiomyopathy, the mitral annulus is dilated and the papillary muscles are outwardly and apically displaced as a result of the spherical LV remodeling. The papillary muscle displacement causes an abnormal tethering of mitral leaflets so that the point of coaptation is inside the LV chamber, well beneath the MV plane. In hypertrophic cardiomyopathy, FMR occurs in late systole as the mitral valve is displaced anteriorly.
In restrictive cardiomyopathy, the LV usually is not dilated and typically exhibits normal systolic function until late in the course of the disease. MR is usually caused by severe atrial enlargement with annular dilation rather than by tethering.
Atrial FMR is a subcategory of secondary MR that occurs in patients with chronic atrial fibrillation and a markedly dilated LA. This form of FMR is caused by pure annular dilation with normal (i.e., Carpentier type I) leaflet motion. It occurs in a minority of patients with chronic atrial fibrillation.
MR may be suspected from the history and physical examination. Exertional dyspnea and fatigue are the predominant symptoms associated with MR. However, in most patients with secondary MR, it can be difficult to distinguish whether symptoms are the result of the underlying cardiomyopathy, FMR, or other common comorbidities such as chronic lung disease, obesity, or deconditioning.
In FMR, the typical holosystolic murmur of MR may be absent. In a small substudy of the Thrombolysis in Myocardial Infarction (TIMI) trial, a murmur was appreciated in only 50% of cases in which MR was clearly present on contrast-enhanced left ventriculography. When the MR is directed posteriorly, as occurs with posterior leaflet tethering, the murmur may radiate to the back and may be missed on routine precordial examination. When LA pressures are severely elevated, the duration of MR is brief and the murmur may be missed or mistaken for an ejection murmur. Findings on chest radiographs are nonspecific and may include cardiomegaly with evidence of LV and LA enlargement and pulmonary vascular congestion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here