Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The ideal scar is narrow, flat with surrounding skin, parallel to the relaxed skin tension lines (RSTLs), or camouflaged within natural anatomic lines.
Available scar revision techniques include excision, irregularization (including Z-plasty, W-plasty, and geometric broken line closure [GBLC]), and dermabrasion.
Hypertrophic scars do not extend beyond the boundaries of the original wound and often regress with time, while keloids invade the surrounding tissue and do not regress with time.
Corticosteroid injections have multiple decades of proven use for hypertrophic and keloid scars, but newer injectables, topicals, and lasers continue to provide clinicians with a wide range of evolving treatment options.
Adjunctive techniques include steroid injection, silicone sheeting, and cosmetics.
With superficial injuries, most facial wounds will heal with little to no scar formation. However, once the reticular dermis has been violated, some amount of residual scarring is destined to occur. Several factors that are beyond the surgeon's control can affect the final appearance of the scar, including the mechanism of injury, position of the wound, health status of the patient, the patient's skin type, and the tendency to form robust scars. Factors that are under the surgeon's control include proper realignment of wound edges, conservative debridement of injured tissues, meticulous handling of tissues during primary repair, and aesthetically favorable alignment of scars whenever possible.
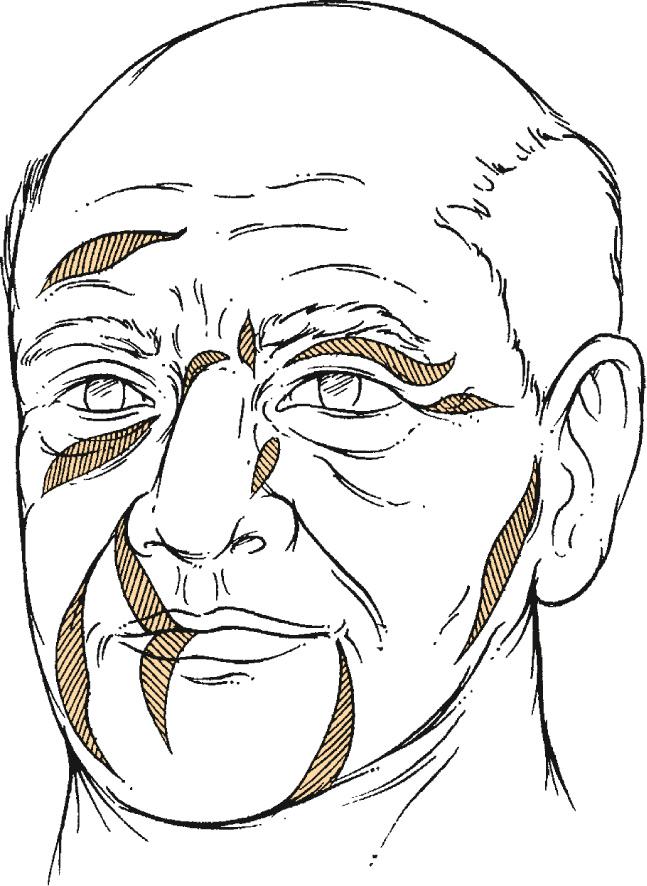
After complete maturation and healing, an ideal scar should have a good color match and be flat and level with the surrounding skin, narrow, and parallel to the relaxed skin tension lines (RSTLs) ( Fig. 18.1 ) or on the border of aesthetic facial subunits ( Fig. 18.2A ). Scars with aesthetically unfavorable characteristics include those that are wide or misaligned with RSTLs or aesthetic subunits, and those that are thickened, hypertrophied, or keloid (see Fig. 18.2B ). The facial plastic surgeon has many options to improve, but not eliminate, these aesthetically unfavorable scars. Successful application of various treatments requires an understanding of which techniques are best indicated when performing scar revision or treating hypertrophic and keloid scars.
Successful scar revision begins with a precise analysis of both the scar and the patient's expectations. Patients often have the false perception that plastic surgery can make an existing scar invisible. The surgeon should educate the patient on the true realistic goal of surgery, which is to modify the scar to a point of maximized camouflage within the natural shadows, lines, and borders that exist within the head and neck. Experience has shown that many scars that are narrow, well positioned along aesthetic subunit borders, or in parallel with RSTLs will continue to mature, improve, and become less noticeable over a period of 12 to 36 months.
Often, patients will have scars that are amenable to improved surgical camouflage. Indications for scar revision include those that are (1) widened; (2) perpendicular to RSTLs; (3) webbed; (4) pin-cushioned; (5) long and linear and misaligned with RSTLs; (6) hypertrophied; (7) interrupting an aesthetic unit of the face; (8) adjacent to, but not lying within, a favorable site; or (9) causing distortion of facial features or anatomic function. Many of these scars should be considered for revision after the first 60 to 90 days of scar maturation has occurred. In fact, early revision with realignment of the scar may allow it to mature more rapidly.
Numerous techniques and interventions are available when planning scar revision. This chapter will discuss the following categories:
Routine scars
Primary closure
Serial excision and expansion
Irregularization, elongation, and reorientation
Topical therapies
Injectable therapies
Dermabrasion
Hypertrophic scars and keloids
Topical therapies
Injectable therapies
Lasers
Radiotherapy and cryotherapy
Adjunctive techniques
A cardinal principle of surgery is that the best treatment of any complication is primary prevention. For scar revision, this translates into the use of proper technique when closing any wound primarily. When presented with wounds that were not closed properly, re-excision with meticulous closure may be all that is needed. Re-excision should be done by use of a fusiform shape with 30-degree angled ends positioned within RSTLs when possible ( Figs. 18.3 and 18.4 ). A slight vertical bevel outward from the original scar will prepare the wound edges for proper everted closure. Routine undermining of 1 to 2 cm around the periphery of the wound allows for reapproximation of the skin edges with minimal tension. The use of buried subcutaneous sutures further decreases wound edge tension. Final eversion of the wound edges is achieved with properly placed monofilament interrupted sutures. Vertical mattress sutures can also prove helpful when wound edge eversion needs to be maximized.

When excising a prior scar, care should be taken to preserve the subcutaneous scar tissue, because this can provide a stable bed for new scar healing. The initial scar excision begins with a scalpel pass just along the edge of the existing scar. This initial skin incision should be performed with a favorable bevel—about 10 degrees off of a true perpendicular cut. The epithelium of the scar is then excised with a sharp scissor or scalpel, but the dermis and immediately deeper tissues are left in the bed of the wound to provide a more stable “platform” on which the revised scar can lie. This is a bedrock principle that should be applied in practically all scar revision cases.
Wide scars, birthmarks, and skin grafts with poor match to surrounding tissues can all be candidates for serial excisions. In some ways, this is a variant of tissue expansion, in that scarred skin is excised and adjacent normal skin brought into the defect area. Like tissue expansion, this technique relies on the skin's biologic creep (ability to stretch over time) and is limited by the given amount of stretch attainable during each excision. Typically, older patients and those with increased skin laxity will require fewer excisions than younger patients with increased skin tone. As with all techniques of scar revision, the patient must be well informed as to the proposed number of excisions and must understand that serial excision can require months to years to complete.
When treating larger scars, the best camouflage is afforded when abundant amounts of similar-appearing tissue can be brought into the repair. Tissue expansion can be a powerful tool to help create excess amounts of surrounding tissue. Tissue expanders are available in a variety of shapes and sizes. Studies on the gain of surface area afforded by the three most commonly shaped expanders have determined that rectangular expanders provide the greatest expansion at 38%, crescent-shaped expanders provide 32%, and round expanders provide only 25%. As a general rule, the base of an expander should be approximately 2.5 to 3 times as large as the area to be reconstructed.
The effects of tissue expansion on skin have been debated. The currently accepted understanding regarding tissue layer expansion is that (1) the epidermis is thickened, (2) melanin production increases, (3) mitotic activity increases, (4) dermis thins (30% to 50%), (5) collagen synthesis is enhanced, (6) hair follicle number remains unchanged, (7) hair density decreases, (8) muscle thins and can atrophy, and (9) blood vessels proliferate. Interestingly, epidermal changes and increased melanin production seen during expansion resolve a few months after surgery.
Implantation of the expanders must take into account the neurovascular supply and final positioning of the skin to be transferred. Expansion can proceed until the skin blanches or the patient complains of discomfort. Intervals between injections can be from 4 to 14 days, ideally two to three times per week.
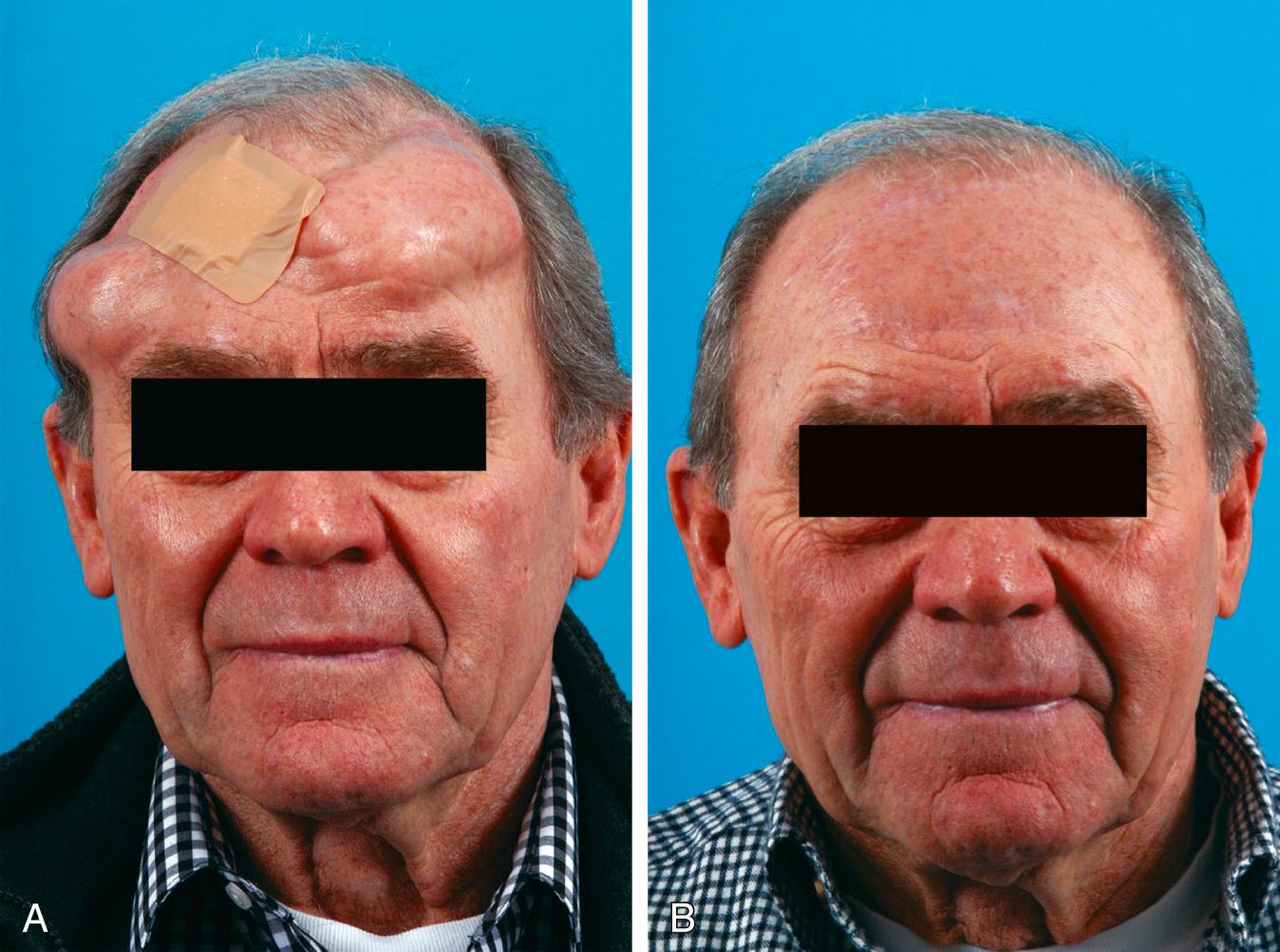
A critical point of understanding for the clinician is the temporary psychological toll that is placed on the patient undergoing expansion. Tissue expanders can cause impressive disfigurement of the head and neck, which naturally results in significant emotional stress to the patient ( Fig. 18.5A ). It is essential to remind the patient that the disfigurement is temporary and that the final reconstruction will warrant the time spent dealing with the expansion devices (see Fig. 18.5B ).
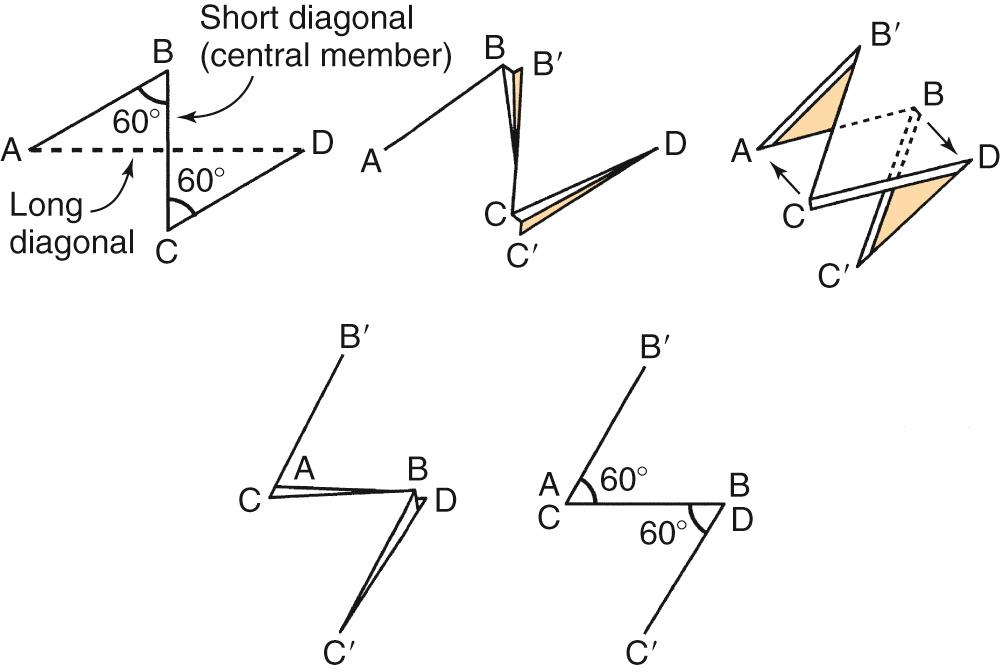
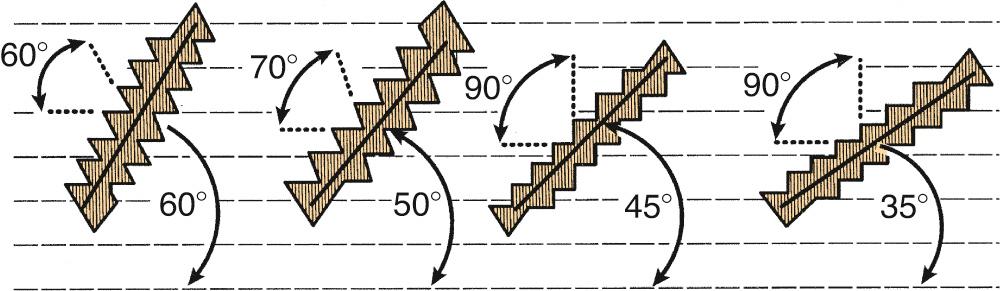
The Z-plasty is one of the oldest and simplest techniques for scar irregularization, with the additional benefits of scar reorientation and adjustable elongation. A “classic” Z-plasty involves the transposition of equilateral 60-degree triangles ( Fig. 18.6 ). When these triangular flaps are transposed and closed, the original direction of the scar is rotated and the scar is lengthened by 75%. When lesser amounts of lengthening are required, a 30-degree or 45-degree Z-plasty can be used to lengthen the scar by 25% or 50%, respectively. Longer scars may benefit from multiple Z-plasties. This can be particularly helpful when correcting scar contractures along anatomic concavities. Consecutive Z-plasties allow for the redistribution of forces more evenly along the entire length of the scar and help camouflage the scar into the surrounding RSTLs ( Fig. 18.7 ).

Both W-plasty and geometric broken line closure (GBLC) are useful irregularization techniques that often use shorter limbs compared with Z-plasty and do not create lengthening of the scar. The general concept is the same—that the human eye will have a harder time following an irregular line versus a straight line. The key difference is that W-plasty creates regular irregularization and GBLC creates irregular irregularization of the final scar line. The technique begins with the marking out of a series of consecutive shapes. The arms should be between 5 and 7 mm in length, and ideally at least one arm of a given shape is in parallel with the RSTLs ( Figs. 18.8 and 18.9 ). Although these segments may look long when marked on the patient's face, due to the natural skin contraction following incision, 5 mm turns out to be the shortest segment one would want to use. After excision previously stated principles of wide undermining, low tension closure, and delicate skin edge suturing are all followed. These wounds are also amenable to postoperative dermabrasion to further camouflage the wound.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here