Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
After reading this chapter you should be able to:
recognise the different presentations of abuse
assess and manage abuse and fabricated illness
know the emotional and behavioural consequence of abuse and neglect
Parents, wider family members, carers, teachers, health professionals, law enforcement agencies and society at large must have a role in protecting children and young people from physical or emotional harm. It is important to recognise that child abuse occurs in all societies, all cultures, all socioeconomic groups, all ethnic groups and all parental age groups.
Health professionals need to be aware of, and recognise, the features and signs of abuse when they meet children and understand that intervention and taking appropriate actions could prevent potentially catastrophic consequence for the child. Most perpetrators of child abuse are known to the child and are often in a position of authority with the ability to manipulate and coerce the child or young person.
child disability
parental mental health problems
parental alcohol abuse
parental drug abuse
domestic violence
socioeconomic deprivation
Proving that particular injuries are the result of abuse is difficult as usually only the perpetrator and the victim were present at the time of the event. Features that should raise suspicion include:
age of the child—inconsistent with the explanation of injury
changing history of events
unreasonable delay in seeking help
repeated contact with health care services
repeated injuries and presentation to emergency department
suggested mechanism of trauma—“fell off settee onto carpeted floor”
multiple fractures
fractures in unusual bones for age
fractures of different ages
inappropriate adult reaction including aggression, vagueness, lack of concern
obvious anxiety or inappropriate reactions of the child
evidence of neglect or poor growth
The recognised forms of child abuse are:
physical abuse
neglect
emotional abuse
fabricated and induced illness
sexual abuse
Recognising that a particular pattern of physical injury is unusual for the age of the child or that it may be the result of physical abuse is a difficult aspect of paediatric care. The issue is further compounded by the fact that children are prone to falls, accidents and injury and thereby sustain physical injuries that have accidental causes. Types of injury seen in physical abuse are:
bruises
fractures
burns
head injury
Bruising is the most common physical sign of abuse and various factors must be considered when abuse is suspected. These would include:
age of child
explanation of cause
location of bruising
pattern of bruising
The age of the child will dictate mobility; it is unusual for a baby or a nonmobile child to have bruising. Bruising is commonly seen in mobile children especially toddlers who are starting to walk.
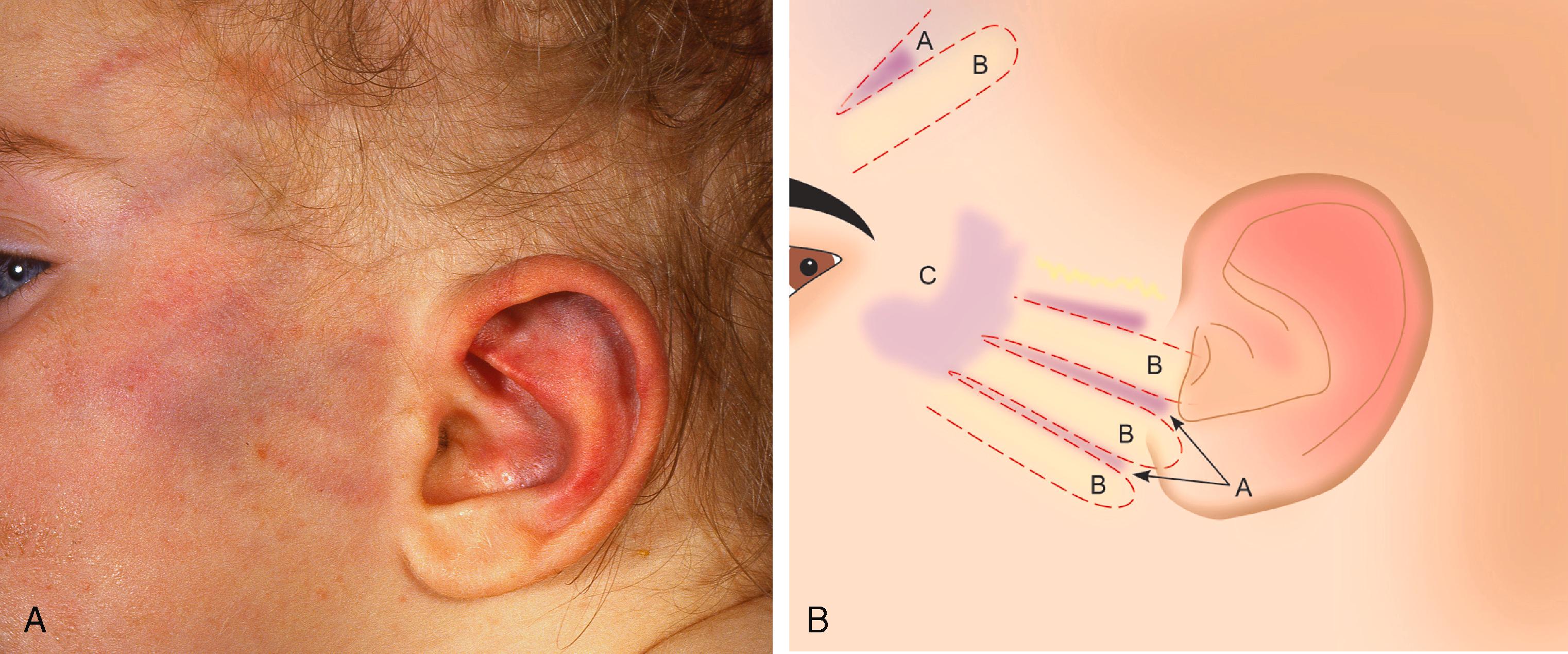
The location of bruises on the shin, knees and elbows are common in a child who is just starting to walk and are usually on the front of the body. Toddlers are likely to injure their foreheads, nose, chin or the back of their head and hence bruises in these locations are not always suspicious. Unusual areas of bruising that should raise suspicion of abuse are ears, neck, buttocks and back of trunk. Bruises in the upper arm or thigh may represent a forceful grip with small circular ‘fingertip’ bruises evident. Bruises on sites away from bony prominences ( Figure 11.1 ) are of concern and require further assessment usually with the child in a place of safety.

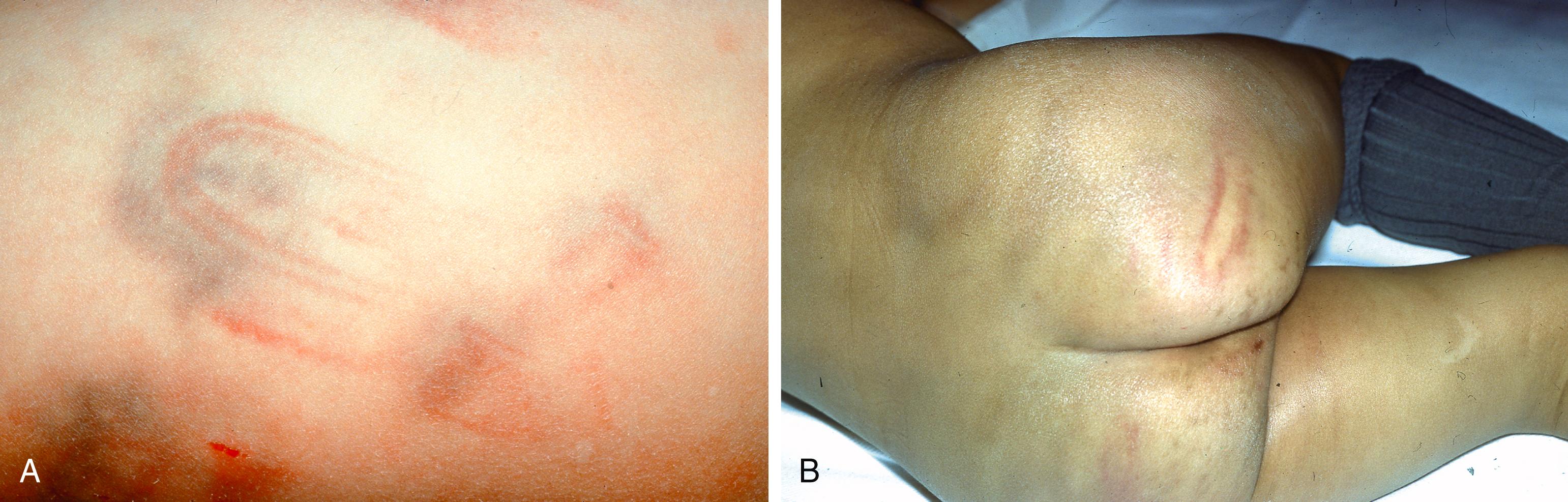
The pattern of bruising can give clues to the mechanism of injury; pinch marks, hand slap marks ( Figure 11.2a and 11.2b ), belts ( Figure 11.3a and 11.3b ) and shoes all cause recognisable bruising patterns. Cluster of bruises with petechiae are common in abuse as they suggest a forceful squeeze or sudden impact leading to leakage from small vessels in the skin. Bite marks ( Figure 11.4 ) leave a characteristic circular pattern of bruising on the skin, and although they can be caused by abusing adults, they can also be caused by other children. This distinction may be obvious, but if doubt exists then the opinion of a forensic dentist will help identify specific tooth patterns and differentiate between the bite from an adult or child.

Colour of bruises change over time and the recording of this was previously used to date the injury. Current evidence, however, suggests that such observations and conclusions are not reliable.
idiopathic thrombocytopenic purpura
rare causes of low platelets and bleeding—e.g. leukaemia
coagulation disorders
congenital dermal melanocytosis in babies
Fractures are a common childhood injury but are the second most common physical injury seen in child abuse. X-rays undertaken for other reasons may identify unexplained and healing fractures and thereby raise suspicion of a previous physical injury. Fractures in children under 18 months and, in particular, in those who are not ambulatory should raise suspicion of an abusive cause. The incidence of fractures as a result of abuse reduces as the child grows older.
Multiple rib fractures, particularly those of different ages or posteromedial in position, without a known history of trauma, birth injury or metabolic bone disease should be considered as abusive in origin and a comprehensive assessment undertaken. The presumed mechanism of these rib injuries is that the infant is held tightly around the chest and shaken.
A 5-month-old boy was brought to the emergency department with a short history of poor feeding, cough and pyrexia. Examination found him to be tachycardic, tachypnoeic with hypoxaemia and localised crackles in left base. He had been born at 34 weeks’ gestation and required CPR at birth due to the umbilical cord being around the neck. He had been well since discharge at 3 weeks of age.
A CXR was requested in the emergency department and showed patchy changes in the lower left area. He was given supplemental oxygen and IV fluids and started on IV antibiotics.
The subsequent review of the CXR by the consultant radiologist identified three posterior rib fractures with callus formation. There were no features suggesting an underlying bone disorder.
The question was therefore asked as to whether these identified fractures were the result of the cardiac massage at birth. The radiologist advised that if callus was present on a CXR when the infant was over 3 months of age (and over 3 months since the episode of CPR) then the fractures would not be considered to result from CPR early in the neonatal period. Any fractures induced over 3 months previously would be expected to have healed and be fully remodelled or in a late stage of remodelling without overt callus.
The conclusion was that the fractures were recent and the result of nonaccidental injury. Safeguarding procedures were implemented.
Metaphyseal fractures are also described in abuse and are seen with multiple other injuries in fatal abuse. In the very young, it is thought to be the result of the limb being pulled or twisted, causing the shearing of the metaphysis. Rarer fractures such as scapular fractures or sternal fractures are also highly suspicious of abuse.
Fractures of the long bones such as humerus and femur are common in both accidental and nonaccidental injury. The most common abusive humeral fractures in children aged less than 5 years are spiral or oblique although it is now recognised that some accidents such as falling down stairs could result in spiral fractures. Supracondylar humeral fractures are common in accidental injury although a fracture of the humeral shaft in a child less than 18 months is suspicious ( Table 11.1 ).
| fractures in absence of adequate explanation | |
| multiple fractures | |
| spiral fracture of humerus in under 5 years | |
| oblique fracture of humerus in under 5 years | |
| under 18 months | |
| metaphyseal fractures | |
| spiral fracture of femur in ‘nonwalker’ (under 15 months) | |
| metaphyseal fractures in young |
When abuse is suspected a detailed skeletal survey of the whole body is undertaken and follow-up images at 4 to 6 weeks to reveal newer fractures as they mineralise and calcify.
The dating of fractures is difficult and the confidence in the time of injury will be over weeks rather than days. Even if the initial skeletal survey is normal, a shorter series of follow-up images should be repeated on all children within 11 to 14 days as this may identify fractures which only become visible when healing.
Preterm babies less than 28 weeks’ gestation at birth or babies with a birthweight less than 1500 gm are at risk of osteopenia and therefore an increased risk of fractures. The most common abnormality seen is fractures to the ribs and are usually an incidental finding on a chest x-ray. Long bones are rarely involved.
Osteogenesis imperfecta is described in more detail in Chapter 29 Musculoskeletal system.
Vitamin D deficiency and rickets, scurvy and osteomyelitis can cause metaphyseal changes but rarely cause fractures.
Children with severe disability have a higher risk of fractures due bone demineralisation from prolonged immobility. Unfortunately, this group of children and young people is also at an increased risk of physical abuse and attempting to clarify the cause of any fracture can be difficult.
Burns can be caused by:
contact with hot surfaces—hot radiators or an iron
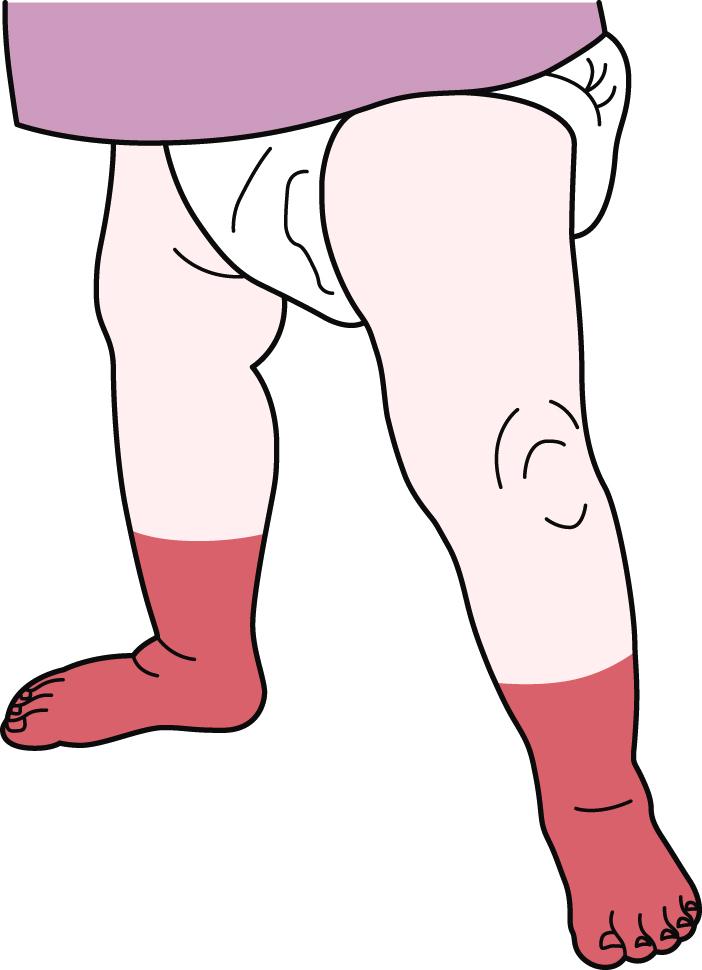
immersion of limbs in hot water ( Figure 11.5 )—produces a glove or stocking distribution
cigarette burns ( Figure 11.6 )—produce deep, circular craters with discrete margins

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here