Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
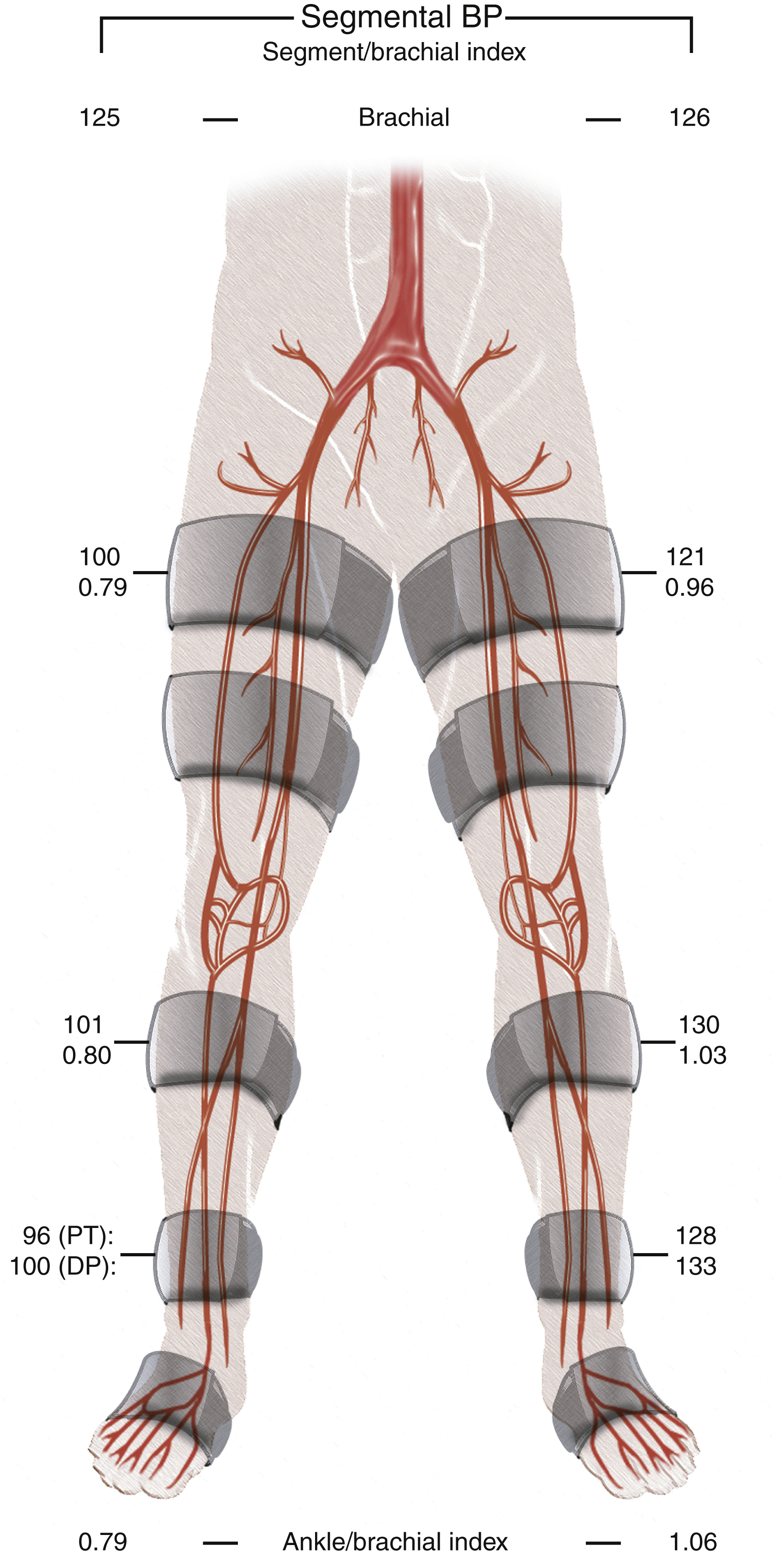
Aortoiliac occlusive disease (AIOD) refers to stenotic or occlusive disease of the infrarenal aorta and iliac arteries, and is a significant cause of peripheral arterial disease (PAD). Epidemiologic studies reporting on PAD include both AIOD and infrainguinal arterial disease, with most patients having multilevel disease. Although more than half of patients with PAD can have a component of AIOD, femoropopliteal and infrageniculate disease are more common causes of PAD. PAD is uncommon before age 50 but increases to around 20% over the age of 60 and over 40% over the age of 85. The prevalence of PAD is most commonly assessed with ankle-brachial pressure index (ABI) or by questionnaires. An ABI of <0.9 is used in clinical practice and epidemiologic studies to diagnose PAD, identifying both symptomatic and asymptomatic patients. The prevalence of asymptomatic PAD is reported as up to 11% and is higher in women than men. The prevalence of PAD is higher in low- and middle-income countries compared with high-income countries and varies by ethnicity, with higher rates reported in African Americans. Risk factors for PAD are well established (Fig. 13.1) . Patients with AIOD are more likely to be smokers and have a 2.5–3.5-fold risk of mortality and cardiovascular events compared with those with distal PAD, whereas patients with diabetes mellitus are more likely to have tibial disease as the cause of PAD. Global smoking trends show a significant decrease in the prevalence of tobacco use in high-income countries but increasing use of tobacco in low- and middle-income countries. At the same time there has been a doubling of the prevalence of diabetes mellitus between 1980 and 2014. This is likely to impact the future disease localization in PAD with increasing tibial disease and stable or declining AIOD, although temporal trends can lag several decades behind smoking trends.
The Trans-Atlantic Inter-Society Consensus (TASC) document classifies aortoiliac disease by angiographic appearance and pattern. It provides recommendations regarding percutaneous versus surgical revascularization based on severity of anatomic obstruction, describing anatomic lesions from a simple focal stenosis (TASC A) through to complex multifocal stenotic and occlusive disease (TASC D). Initially published in 2000, the guidelines were updated in 2007 as TASC II. A further update in 2015 expanded the TASC classification to include below-the-knee arteries, but due to a lack of contemporary randomized controlled trials no new guidelines were issued regarding revascularization of AIOD. It was recognized there had been significant change in clinical practice secondary to a rapid evolution in technology and increasing technical skill of endovascular specialists. Consensus was not achieved on the concept of recommending an “endovascular-first” approach for more complex TASC C and D lesions, and the update reflected a pragmatic approach to clinical practice, advising that the choice of revascularization method should be based on each vascular center’s experience and competence in treating complex AIOD. For complicated (TASC D) cases the update advised that primary surgical or hybrid endovascular and open strategies may be more appropriate in medically fit patients because the durability of an open approach over time may be superior to an endovascular procedure.
A directed history and physical examination should be performed to determine the presence and severity of PAD, bearing in mind that patients with hemodynamically significant aortoiliac disease are often asymptomatic, with only one-third presenting with intermittent claudication (IC). Clinical classification of systems for grading PAD are used widely in research and can also provide objective criteria for assessing the baseline disease state, disease progression, and treatment decisions for individual patients. The Fontaine Classification and Rutherford Classification are most widely used, and the Rutherford Classification includes clinical criteria with noninvasive objective criteria to assess the grade of PAD ( Table 13.1 ).
| Study Name | First Author, Year ∗ | No. of Subjects | Country | Population | Study Design | PAD End Point |
|---|---|---|---|---|---|---|
| Index studies | ||||||
| Cardiovascular Health Study | Newman, 1993 28 | 5084 | United States | Aged 65+ | Cross-sectional | ABI<0.9 |
| Framingham Study | Murabito, 1997 32 | 5209 | United States | Cross-sectional | IC | |
| Rotterdam Study | Meijer, 2000 33 | 6450 | Netherlands | Cross-sectional | ABI<0.9 (<0.7 also studied) | |
| Framingham Offspring Study | Murabito, 2002 26 | 3313 | United States | Longitudinal | ABI<0.9 | |
| Multiethnic Study of Atherosclerosis | Allison, 2006 34 | 6653 | United States | Cross-sectional | ABI<0.9 | |
| Other large studies | ||||||
| Quebec Cardiovascular Study | Dagenais,1991 35 | 4570 | Canada | Men only | Longitudinal | IC |
| Edinburgh Artery Study | Fowkes, 1992 36 | 1592 | Scotland | Cross-sectional | ABI and reactive hyperemia | |
| Israeli Ischemic Heart Disease | Bowlin, 1994 22 | 10059 | Israel | Middle-aged men | Longitudinal | IC projected |
| Reykjavik Study | Ingolfsson, 1994 21 | 9141 | Iceland | Men only | Longitudinal | IC |
| Honolulu Heart Program | Curb, 1996 37 | 3450 | United States | Japanese American men | Cross-sectional and longitudinal | ABI<0.9 |
| Limburg PAOD Study | Hooi, 2001 25 | 2327 | Netherlands | Longitudinal | ABI<0.95 | |
| Women's Health and Aging Study | McDermott, 2000 38 | 930 | United States | Women aged 65+ | Longitudinal | ABI<0.9 |
| Physicians' Health Study | Ridker, 2001 39 | 14916 | United States | Male physicians | Nested case-control | IC or PAD surgery |
| San Diego Population Study | Criqui, 2005 40 | 2343 | United States | Multiethnic | Cross-sectional | ABI<0.9, abnormal waveform, PAD revascularization |
| National Health and Nutrition Examination Survey | Pande, 2011 41 | 7458 | United States | American men | Longitudinal | ABI<0.9 |
| and women aged 40+ | ||||||
| Health Professionals Follow-Up Study | Joosten, 201 2 42 | 51529 | United States | Male health professionals | Longitudinal | Clinical PAD † |
∗ Where multiple articles were published, this refers to the article most frequently referenced herein.
† lncludes limb amputation or revascularization, angiography with vascular obstruction >50%, ABI<0.90, or physician-diagnosed PAD.
Clinical examination showing reduced or absent femoral pulses can indicate AIOD as the main territory contributing to PAD. Other vascular systems should be examined, including for carotid artery bruit or abdominal aortic aneurysm. Patients with AIOD can present with IC, most often affecting the calf muscles, with thigh or buttock claudication suggestive of more extensive AIOD. Symptoms of buttock claudication that occur in association with erectile dysfunction in patients with absent femoral pulses is recognized as Leriche syndrome. This syndrome occurs when either preocclusive stenosis or complete occlusion of the infrarenal aorta is present as a result of severe aortic atherosclerosis.
After a patient is identified with symptoms consistent with PAD it is important to rule out other potential etiologies that can mimic PAD symptoms, especially neurogenic claudication. Measurement of the ABI is the most widely used initial investigation for establishing a diagnosis of PAD. An ABI of <0.90 has been demonstrated to have high sensitivity and specificity for the identification of PAD.
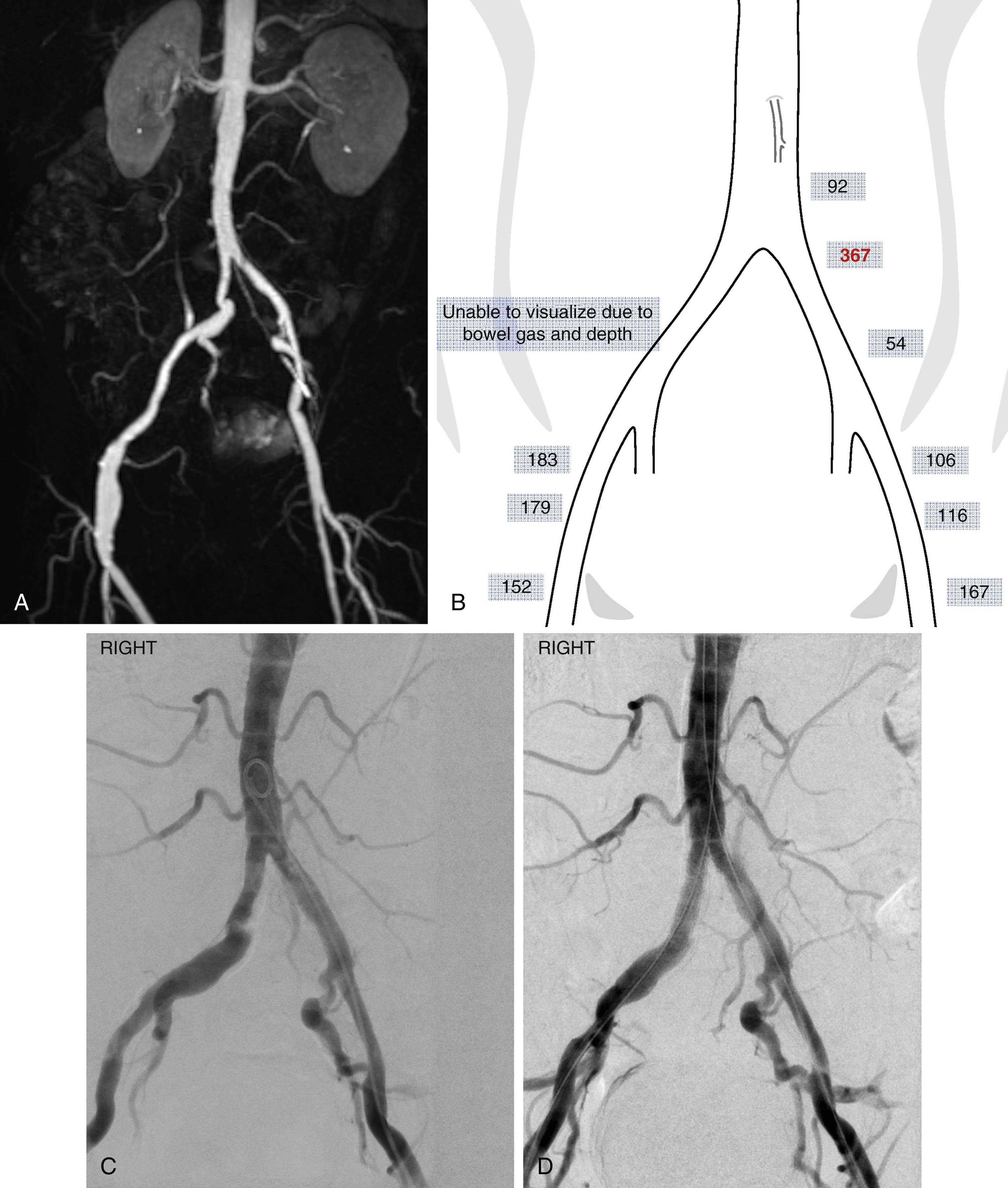
Duplex arterial mapping is still widely used in vascular laboratories for initial imaging of AIOD. For most patients it can provide a safe and inexpensive means of assessing the location and extent of hemodynamically significant stenosis in the aortoiliac territory with high sensitivity and specificity compared with computed tomographic (CT) angiography (CTA) and conventional catheter angiography. The presence of significant arterial calcification, overlying bowel gas, and large body habitus can exclude some patients from assessment with ultrasound. The need for highly trained vascular technologists can also limit access to duplex arterial mapping.
Targeted Doppler ultrasound can also be used to clarify findings on magnetic resonance and CTA studies when there is uncertainty that the degree of stenotic disease is at a threshold for intervention ( Fig. 13.2 ).
Multidetector CT has rapidly evolved from 4-detector row systems in 1998 to 256-slice and 320-detector row CT systems with smaller detector element size and faster gantry rotation speeds. This allows a larger volume of coverage per gantry rotation, permitting rapid acquisitions of vascular anatomy over an extensive area. CTA of aortoiliac arteries are usually acquired as part of CTA of the thoracoabdominal aorta or as part of a peripheral CTA covering from the abdomen to the toes in a single acquisition. The increase in spatial resolution, with submillimeter isotropic acquisition, has seen an equally rapid development in image postprocessing and reconstruction from the acquired CTA three-dimensional (3D) dataset. Dedicated software can reconstruct the 3D data in any anatomic orientation with multiplanar reformatted, maximum intensity projection, and volume-rendered algorithms.
The improved spatial resolution and typical vessel size in the aortoiliac segment mean CTA is less affected by calcification than in the infrainguinal territory. The sensitivity of CTA for stenotic and occlusive disease may be higher than conventional angiography in AIOD, making it the diagnostic imaging of choice for many centers planning intervention of aortoiliac occlusive disease. Identification of extensive calcification in AIOD is important in planning intervention because it can be a predictor of complications, including rupture.
Magnetic resonance angiography (MRA) is a noninvasive technique that does not employ ionizing radiation or iodinated contrast material and has benefited from significant developments in technology since it was first reported in 1985. MRA of peripheral vascular anatomy now reports high sensitivities and specificities for the detection of angiographically proven arterial stenotic and occlusive disease. Contrast-enhanced MRA has similar accuracy to CTA for classifying TASC lesions in AIOD. Future MRA sequences may hold promise for demonstrating arterial calcification that could mitigate the previous limitation of poor visualization of calcium when planning intervention in AIOD. Time-resolved contrast-enhanced MRA gives a dynamic assessment of arterial flow, but this is more frequently used for imaging infrageniculate PAD. MRA of the pelvis is still limited by susceptibility artifacts in patients with metallic hip implants.
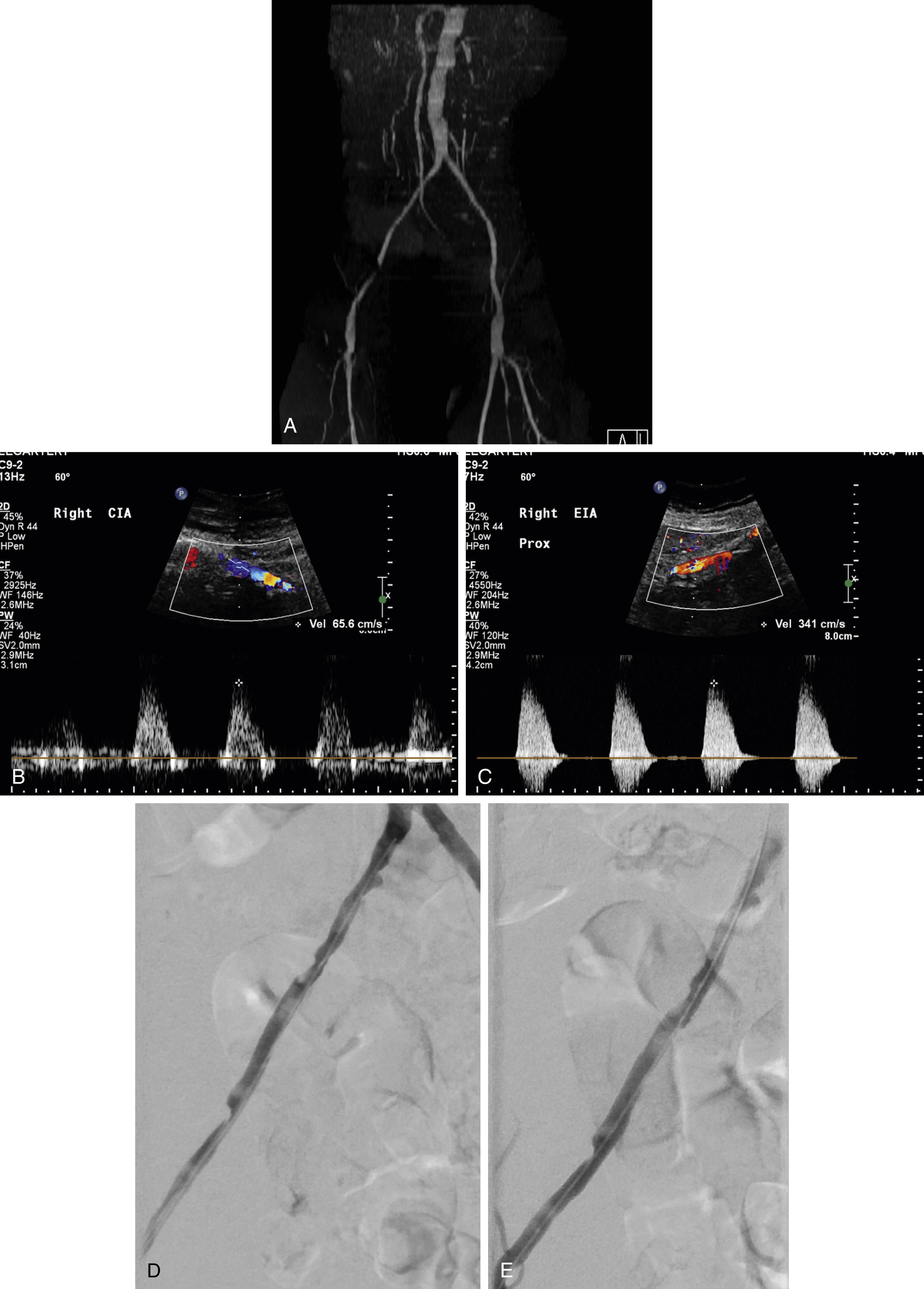
Non–contrast-enhanced MRA avoids the potential risks of nephrogenic systemic fibrosis and contrast-induced nephropathy, as well as ionizing radiation. Recent developments in non-contrast MRA sequences have overcome the previous limitations resulting from long acquisition time, flow and movement artifacts, and saturation effects as occurred with time-of-flight sequences. Quiescent interval single-shot MRA (QISS) appears best placed for imaging the lower extremities because the technique allows for large anatomic coverage in short imaging times. Although overall image quality is lower than CTA, Wu et al. reported high sensitivity (>93%) and specificity (>96%) for assessment of stenoses. They suggested this may be due to currently better spatial and temporal resolution for CTA (1 mm × 1 mm ×0.625 mm) than QISS MRA (1 mm ×1 mm ×3 mm). However QISS had significantly higher sensitivity for stenoses in heavily calcified vessels compared with CTA, which may be more relevant in AIOD ( Fig. 13.3 ).
Only a very small cohort of patients with AIOD may be considered appropriate for diagnostic catheter angiography. Almost all patients are able to have noninvasive imaging of the aortoiliac arteries by either CTA, MRA, or Doppler ultrasound, allowing patients to be planned for direct intervention for AIOD at the time of angiography. Patients with end-stage renal failure may not be suitable for intravenous gadolinium or iodinated contrast, but stenotic and occlusive disease can be mapped with Doppler ultrasound and unenhanced CT may have a role in demonstrating aortoiliac calcification before proceeding to intervention. CO 2 angiography can be performed with no recognized risk of causing renal impairment. It can be performed easily and safely, with minimal risk of air contamination, by a number of automated systems (Angiodroid SRL, San Lazzaro di Savena, Italy; CO2mmander CO 2 Injector, AngioAdvancements, Ft. Meyers, FL; INSPECT 3005R and 2005R, Malek Medical GmbH, Wismar, Germany). CO 2 angiography requires familiarity with the technical details of injection, and specific risks including vapor lock that can lead to nonocclusive mesenteric ischemia. Diagnostic catheter angiography can be performed via common femoral or radial artery approach, the latter allowing for rapid recovery and mobilization. Advancing developments in image fusion allow noninvasive diagnostic imaging to be fused with real-time fluoroscopic acquisition to help guide interventional procedures. This can reduce radiation exposure and contrast dose and will likely take a greater role in guiding interventional procedures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here