Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
After reading this chapter you should be able to assess, diagnose and manage:
chronic cough
wheezing illnesses
lower respiratory tract infection
cystic fibrosis presentation
sleep disordered breathing
life-threatening events including sudden unexpected death in infancy
and
select and interpret appropriate respiratory investigations
understand the indications for long-term ventilation and respiratory support
Values for carbon dioxide and pH do not differ markedly between arterial and venous samples and both will provide important information for clinical care ( Table 17.1 ). Oxygen results from venous and capillary samples reflect values after tissue perfusion and are therefore ignored in clinical practice.
| abnormality | primary disturbance | effect on | base excess | compensatory response | |
|---|---|---|---|---|---|
| pH | pCO2 | ||||
| respiratory acidosis | ↑ pCO2 | ↓ | ↑ | negative | ↑ [HCO3-] |
| metabolic acidosis | ↓ [HCO3-] | ↓ | N or ↓ | negative | ↓pCO2 |
| respiratory alkalosis | ↓ pCO2 | ↑ | N or ↓ | positive | ↓[HCO3-] |
| metabolic alkalosis | ↑ [HCO3-] | ↑ | N or ↑ | positive | ↑pCO2 |
Radiological investigation of respiratory disease is commonly used in clinical practice. The posterior-anterior (PA) film is preferable where possible so as to facilitate assessment of cardiac size, although an anterior-posterior (PA) film may be practicable in the acutely ill or small child. Lateral films expose the child to significantly more radiation and rarely add clinically useful information.
The correlation between peripheral saturation measurement and arterial saturation is sufficient for most clinical assessments. Since the technique measures absorbance in haemoglobin, it may provide normal values in anaemic individuals even though the oxygen carrying capacity is significantly reduced and it may also give low saturation values in individuals with poor peripheral perfusion.
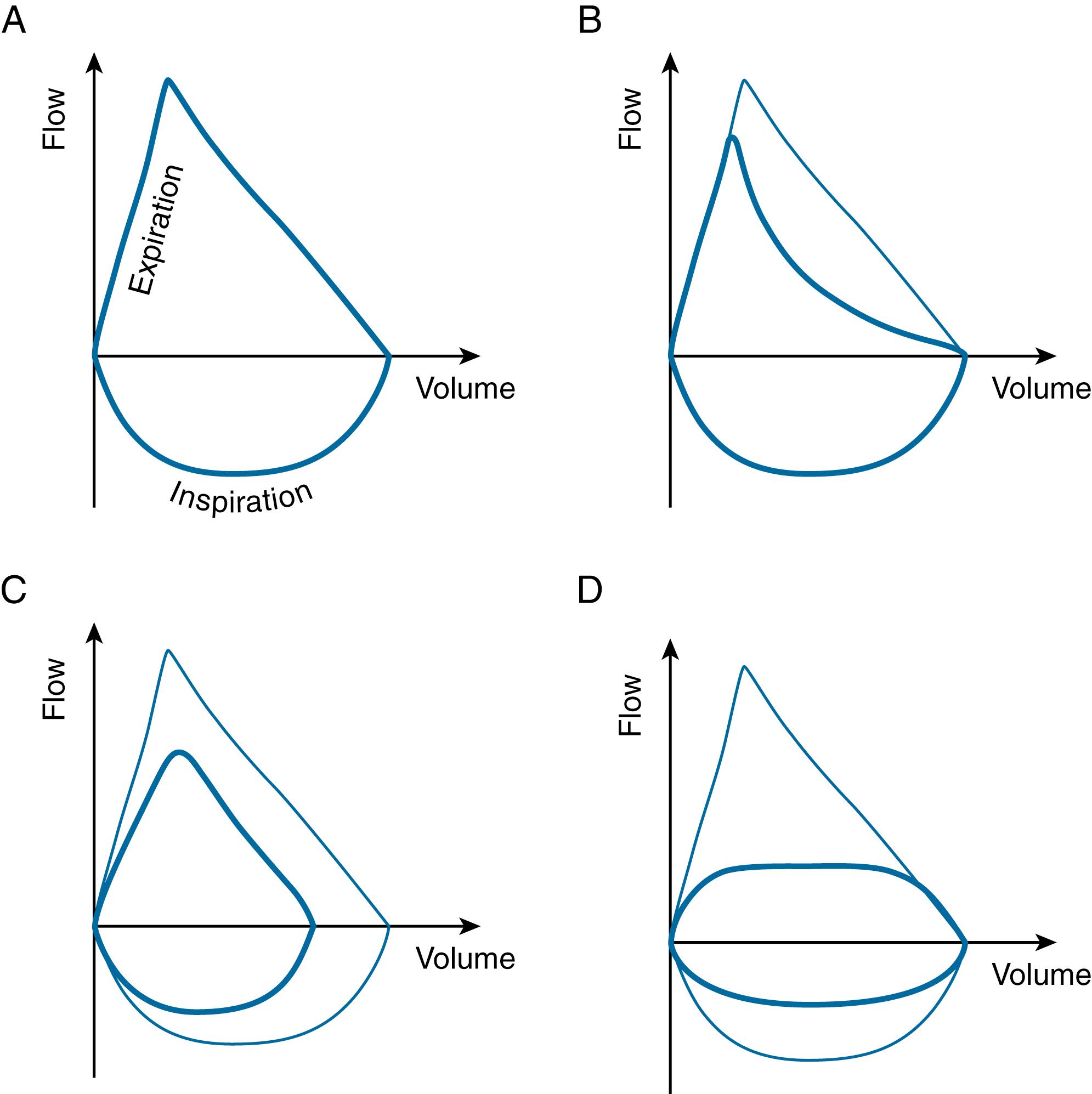
Spirometry measures lung volumes, usually during a forced exhalation and inhalation manoeuvre, and the test is usually possible in children over the age of 5 or 6 years ( Figure 17.1 ). In forced manoeuvres such as the Forced Expiratory Volume in 1 second (FEV 1 ), the increased intrathoracic pressure during forced exhalation is transmitted to the bronchi, acting to decrease the diameter of the lumen and so limiting the rate of flow—this is termed ‘dynamic airway narrowing’.
During spirometry, a variety of volumes are measured, and there are recognisable patterns of these ( Table 17.2 ). Reference values allow the spirometry measurements of a child to be compared to the average measurements for their age, sex, height and race and these can be expressed in the form of a percentage predicted or a Z score.
A: in a well child, the loop proceeds in a clockwise manner initially with a rapid rise of flow over a small volume, reaching the Peak Expiratory Flow Rate (PEFR). Over the remaining lung volume, the patient expires to the end of vital capacity. The downward reflection of the loop below the zero line, back to the origin, represents the inspiration after the forced expiration.
B: an ‘obstructed’ loop. Note the concavity of the downward phase of expiration.
C: a ‘restrictive’ pattern. Note that the volume is decreased—the flow rate may be more normal.
D: extra-thoracic fixed obstruction (e.g. vascular ring around the trachea or mediastinal mass). Note that the peak inspiratory and expiratory flows are both reduced.
| FEV1 | FVC | FEV1/FVC ratio | Interpretation |
|---|---|---|---|
| normal | Normal | Normal | normal |
| reduced | normal | reduced | obstruction (e.g. asthma, cystic fibrosis) |
| normal/reduced | reduced | normal/increased | restriction (e.g. pulmonary hypoplasia, scoliosis, interstitial lung disease) |
Assesses children and young people (from age of 5 years) for bronchial hyperreactivity by recording spirometry values before and after the administration of a bronchodilator (usually salbutamol). An improvement in FEV1 of 12% or more is regarded as a positive response.
The bronchoprovocation test assesses whether a child with initially normal pulmonary function tests may actually produce abnormal results when an inhaled irritant is given. The typical agents used to challenge the airways are methacholine, histamine and adenosine. The concentration of the agent which induces a 20% fall in FEV 1 is recorded and the lower the dose then the greater the degree of airway hyperreactivity. Exercise can also be used as a ‘provocation test’. Both these investigations should be undertaken by teams competent in their administration.
FeNO can be measured in most school-aged children and is an indicator of airways inflammation. It is useful where the history suggests asthma but spirometry is normal or an obstructive pattern is not reversible. Levels of >35 parts per billion are abnormal in children aged 5–18 years.
Bronchoscopy uses either a rigid or flexible bronchoscope and allows direct visualisation of the internal airway structure and allows for microbiological sampling or biopsy. Inhaled foreign may be located and extracted.
This measures thoracic gas volumes, including air that is not directly communicating with the airway opening (such as ‘trapped gas’ or lung cysts).
The rate of oxygen diffusion across the alveolar membrane can be assessed by measuring diffusing capacity of carbon monoxide, but the test can only be done in cooperative older children.
Cough is a reflex which removes mucous and other material from the lungs and is less effective in glottic dysfunction, tracheostomy and neuromuscular weakness.
Cough can be the cardinal feature of both acute, life-threatening and chronic, life-limiting respiratory disease and the causes can be categorised by the age of the child ( Table 17.3 ), the duration of the cough and the character of the cough.
| Infant | Preschool | School age/adolescent |
|---|---|---|
| primary ciliary dyskinesia cystic fibrosis infections (viruses, bacteria, chlamydia, pertussis) congenital malformations (tracheoesophageal fistula) |
foreign body infection cystic fibrosis primary ciliary dyskinesia bronchiectasis immunodeficiency asthma passive cigarette smoke aspiration |
asthma postnasal drip infection cystic fibrosis primary ciliary dyskinesia immunodeficiency bronchiectasis smoking air pollution tic cough aspiration |
The character of the cough can be described as ‘wet’ or ‘dry’ with the former suggestive of excessive secretions. In infants and children, a cough associated with sputum production is rarely ‘productive’ as the sputum is usually swallowed rather than expectorated. A wet cough implies infection and, if chronic, suggests protracted bacterial bronchitis, suppurative lung disease or bronchiectasis. A wet cough might also feature in gastro-oesophageal reflux and aspiration. An acute viral cough can last 3 to 4 weeks whilst the ‘postinfectious cough’ can last much longer, especially in pertussis.
This is the most common cause of a prolonged cough over 4 weeks duration in preschool children. The child usually looks well, has no other clinical signs and has normal growth. It is typically associated with infection by M. catarrhalis, S. pneumoniae and H. influenzae and can be treated effectively with a prolonged (2–4 week) course of an oral antibiotic, such as coamoxiclav. The diagnosis is confirmed by the resolution of symptoms after the trial of therapy. If the cough does not resolve after 4 weeks of antibiotics, then chronic suppurative lung disease or bronchiectasis should be considered.
A cough should be investigated thoroughly if any of the following are present:
sudden onset cough after choking
night sweats
haemoptysis
poor weight gain or weight loss
cough which progressively worsens
signs of lung disease—clubbing, barrel-shaped chest, Harrison’s sulci
For a chronic wet cough, a typical approach would involve chest radiographs, bacterial cough swab and viral swabs, a sweat test and an initial immune panel (immunoglobulins, functional antibodies, full blood count and lymphocyte subsets). If primary ciliary dyskinesia is suspected, patients are referred for ciliary studies to a national referral diagnostic centre whilst, if bronchiectasis is suspected, a CT scan should be undertaken. Bronchoscopy may also be indicated.
Treatment is directed at the underlying cause. There is no role for over-the-counter ‘cough medicines’ which usually contain opiate-derived compounds to suppress the cough. When a cough is felt to be benign, a watch-and-wait approach is appropriate.
Young children inherently have narrow airways and consequently generate wheeze with only minimal reduction in the diameter of the bronchi and bronchioles. Most wheeze occurs in the expiratory phase as the increased intrathoracic pressure required for expiration will also lead to external pressure on the smaller airways. A biphasic wheeze or a very localised wheeze suggest a fixed area and warrants further consideration ( Table 17.4 ).
| Cause | Examples |
|---|---|
| infective | mycoplasma pertussis viral induced wheeze—adenovirus, respiratory syncytial virus, human metapneumovirus, parainfluenza, influenza |
| inflammatory | hypersensitivity pneumonitis irritant inhalation—smoke, illicit drugs sarcoidosis vasculitis |
| physical compression | foreign body aspiration granulation tissue in airway lymph node enlargement tumour—lymphoma vascular ring, vascular compression tracheo-bronchomalacia bronchogenic or pulmonary cyst |
| complex pathophysiological | primary ciliary dyskinesia cystic fibrosis bronchiectasis aspiration and gastro-oesophageal reflux disease. hyperventilation. |
| upper airway | vocal cord palsy vocal fold dysfunction angioedema |
The key clinical features of asthma are episodic wheeze that is present during exacerbations along with breathlessness and cough. Some patients have interval symptoms, which include breathlessness, cough and wheeze that may be exacerbated by exertion, changes in environmental temperatures, damp air, emotion and laughter. Nocturnal cough may also be present. Between attacks many children may be symptom free with normal lung function. Those patients with poorly controlled asthma may have a hyperinflated chest and develop Harrison’s sulci ( Figure 17.2 ) which are fixed inward grooves in the chest wall where the diaphragm inserts into the internal surfaces of the ribs.

An acute asthma attack is associated with breathlessness and a feeling of a ‘tight’ chest, with a characteristic nonproductive cough. Clinical signs include:
tachypnoea
intercostal recession
chest indrawing
‘tracheal tug’
prolongation of the expiratory phase of breathing
wheeze which may be audible without a stethoscope
In more severe asthma, patients use their accessory muscles of respiration. Oxygen saturations are often maintained during an attack and when patients do deteriorate, they are usually hypoxic prior to becoming hypercapnic as the latter finding is a late feature, and indicates a severe, or life-threatening episode ( Table 17.5 ).
| Mild-moderate | Severe | Life threatening |
|---|---|---|
| oxygen saturation 92% and above in air PEFR > 50% predicted of best |
cannot complete sentences in one breath or too breathless to talk or eat/feed oxygen saturation < 92% in air PEFR < 50% predicted or best |
cyanosis silent chest poor respiratory effort fatigue or exhaustion agitation or reduced level of consciousness raised carbon dioxide |
| under 6 years heart rate < 140/min respiratory rate < 40/min |
under 6 years heart rate > 140/min respiratory rate > 40/min |
|
| 6 years and over heart rate < 125/minrespiratory rate < 30/min | 6 years and over heart rate > 125/min respiratory rate > 30/min |
Asthma is often associated with other atopic conditions, in particular hay fever, food allergies and eczema. There is often a strong history of familial atopy.
Wheeze in the under 5-year olds
A current challenge is that many children wheeze in the preschool period and such children are often diagnosed with ‘pre-school wheeze’ rather than asthma. This can be categorised as either:
recurrent viral-induced wheeze—evidence of a viral infection with each occurrence of wheeze
multi trigger wheeze—episodic wheeze after exposure to pollen, moulds or house dust mite
In reality, many children will move between the two groups and the current NICE guidelines recommend treating them based on observation and clinical judgment along with regular reviews.
No single test is diagnostic of asthma, but a history of recurrent wheeze which responds to treatment is useful. Spirometry is the key diagnostic test and can be performed in most children who are 5 years and older. The FEV 1 , FEV 1 /FVC ratio and the FEF 25–75 are all reduced.
Administration of a bronchodilator (usually salbutamol) should result in an improvement, and an increase in FEV 1 volume of 12% over the baseline is considered reversible airflow obstruction. Peak expiratory flow is highly effort dependent and it alone should not be relied upon.
Exercise challenge tests are useful and spirometry is undertaken before and after exercise. A decrease of 10% of FEV 1 is usually considered diagnostic of exercise-induced asthma.
There are several stepwise approaches to increasing asthma treatment but central to all the guidelines is regular review of symptoms and the stepping down of therapy when appropriate. A further key component of treatment is the avoidance of cigarette smoke ( Table 17.6 ).
The major challenge in asthma is adherence to medication and it is well recognised that many patients take only around half their prescribed doses of inhalers. Therefore, rather than automatically ‘stepping up’ treatment, a careful, sensitive discussion around adherence is often more helpful if patients have frequent exacerbations or loss of control of daily symptoms.
| Situation | Therapy |
|---|---|
| if infrequent, short-lived wheeze and normal lung function | consider SABA as reliever therapy alone |
| if asthma-related symptoms 3 times a week or more, or causing waking at night or uncontrolled with a SABA alone | consider low-dose ICS as the first-line maintenance therapy |
| if uncontrolled on a paediatric low dose of ICS | consider LTRA in addition to the ICS and review the response to treatment in 4 to 8 weeks |
| if uncontrolled on a low dose of ICS and an LTRA as maintenance therapy | consider stopping the LTRA and starting a LABA in combination with the ICS |
| if uncontrolled on a paediatric low dose of ICS and a LABA as maintenance therapy | consider changing the ICS and LABA maintenance therapy to a MART regimen with a paediatric low-maintenance ICS dose |
| if uncontrolled on a paediatric low-maintenance ICS dose with LABA | consider increasing the ICS to a paediatric moderate maintenance dose (either continuing on a MART regimen or changing to a fixed dose of an ICS and a LABA, with a SABA as a reliever therapy) |
| if asthma is uncontrolled in children and young people (aged 5 to 16) on a paediatric moderate maintenance ICS dose with LABA (either as MART or a fixed-dose regimen) | seek advice from a healthcare professional with expertise in paediatric asthma management |
Guidelines for the pharmacological management of asthma are published by NICE, BTS/SIGN and GINA (Global Initiative for Asthma Management and Prevention). There are some differences between these guidelines but all follow a similar approach to management.
Children and young people with asthma are at risk of acute attacks which may progress rapidly and become life threatening. Presentation requires prompt assessment and administration of high flow oxygen through a tight-fitting mask when the SpO 2 is less than 94% or there is any suggestion of respiratory compromise.
Those with a mild to moderate episode should be given inhaled ß 2 -agonist and, if there is a failure of response, inhaled ipratropium bromide should be added via a nebuliser. Oral steroids should be administered at an early stage when possible although their effect will not be immediate.
If reassessment after a short interval reveals a poor response, then an initial single bolus dose of intravenous salbutamol is given followed by intravenous magnesium sulphate if there is a minimal response. Discussions with colleagues from anaesthetics and paediatric intensive care should be undertaken.
A 15-year-old girl was referred for evaluation of recent onset of cough and wheeze. She had been well previously, had no history of atopy and she was not a smoker. She was, however, a high performing runner but would develop symptoms as soon as he started sprinting on the field. She described an inspiratory stridor, dry cough, tightness of chest and throat. She would stop running and the coughing would cease. She had been on high-dose combination of inhaled steroids and long-acting beta agonists without any benefit.
Her spirometry was entirely normal at baseline; however, after strenuous exercise on treadmill there was marked decrease in inspiratory flow volume. There was associated inspiratory wheeze. Continuous nasolaryngoscopy whilst on treadmill demonstrated severe adduction of laryngeal structures in parallel with severe respiratory distress. Psychological evaluation did not reveal any obvious contributing factors.
A pH study demonstrated frequent gastro-oesophageal reflux and endoscopy indicated that this may be long standing.
A diagnosis was made of exercise-induced laryngeal obstruction secondary to chronic gastro-oesophageal reflux.
Treatment with proton-pump inhibitor was commenced and a referral made to speech therapy with the aim of controlling laryngeal dysfunction. Following this intervention, she had a marked improvement in symptoms and her inhaled medications were withdrawn. She was able to return to high performance running.
A microbiological diagnosis is not made in most children with pneumonia but the organisms likely responsible depend on the age of the child. In older children Streptococcus pneumoniae and Mycoplasma pneumoniae are commonly implicated with the latter more common in school-age children. In those under 2 years, the commonest bacterial cause of pneumonia is Streptococcus pneumoniae which causes around a third of radiologically confirmed pneumonia in this age group. A viral cause is more common in younger children—commonly respiratory syncytial virus (RSV) or human metapneumovirus. Infections caused by group A streptococcus and Staphylococcus aureus are more likely to cause necrotising pneumonia and children with these infections are more likely to require intensive care.
The physical signs of pneumonia will help make a clinical diagnosis and also assign the degree of severity and guide management. Although some factors differ between infants and young children, the common findings are fever, tachypnoea, respiratory distress, chest pain, abdominal pain and headache. Cough may be absent initially. Wheeze is uncommon in children with pneumonia.
| Airway and breathing sleep-related disorders | ||
|---|---|---|
| obstructive sleep apnoea and hypoventilation | ||
| high-risk children | ||
| Down syndrome | ||
| neuromuscular disease | ||
| craniofacial syndromes | ||
| mucopolysaccharidoses | ||
| achondroplasia | ||
| Prader Willi syndrome | ||
| congenital central hypoventilation syndrome | ||
| Nonrespiratory sleep disorders/disorders with daytime sleepiness | ||
| insufficient night sleep | ||
| narcolepsy | ||
| idiopathic CNS hypersomnia | ||
| chronic fatigue syndrome | ||
| delayed sleep phase syndrome | ||
| restless leg syndrome | ||
| non-REM arousal disorders | sleep terror, sleep walking, confusional arousals | |
| sleep–related movement disorders | ||
| REM parasomnias | nightmares, REM movement disorders | |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here