Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
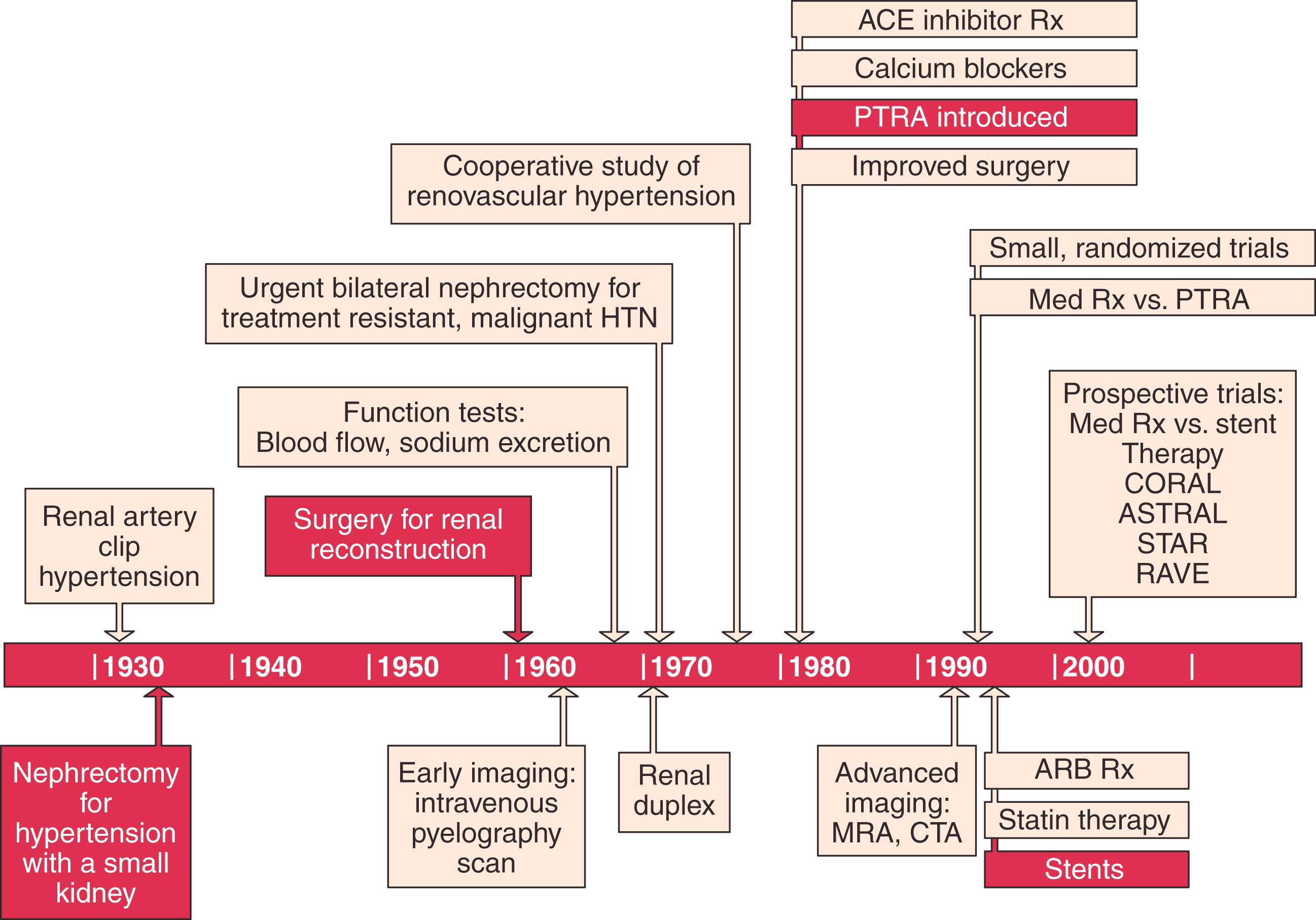
Following Goldblatt’s innovative work defining the causal relationship between renovascular disease and hypertension in 1934, the surgical management of renovascular disease evolved through three eras: nephrectomy, open surgical correction, and finally renal artery angioplasty with or without stenting ( Fig. 128.1 ). Each era was met with initial enthusiasm, which was soon tempered by the modest results of each treatment. Nephrectomy is now rarely indicated in the management of renovascular disease, and recent randomized clinical trials comparing renal artery stenting with best medical management have demonstrated no advantage of catheter-based intervention (see Ch. 129 , Renovascular Disease: Endovascular Treatment). This chapter reviews patient selection for open repair of renovascular disease and then describes specific surgical approaches and their expected outcomes in contemporary practice.
The rationale for the treatment of renovascular disease by any method is to improve event-free survival. Our experience with 500 consecutive patients treated for atherosclerotic renovascular disease suggests that severe hypertension can be viewed as a key preoperative characteristic favoring clinical benefit, whereas renal function after operation can be considered the key clinical response. An early incremental increase in excretory renal function has been the primary determinant of dialysis-free survival for all atherosclerotic patients. ,
Unfortunately, once renovascular disease is identified in combination with severe hypertension, discriminating predictors of blood pressure and renal function response are lacking. Lateralizing renin assays have predicted blood pressure benefit but not blood pressure cure. , Moreover, renal function response in patients with ischemic nephropathy is uncertain after renal artery intervention. Studies have also described a significant correlation between parameters derived from segmental renal artery Doppler spectral analysis (i.e., resistive index) and response to intervention as well as progression to dialysis dependence. , However, we have not been able to reproduce these results for open operative management of renal artery disease. Rather, in our clinical experience with more than 1000 patients with atherosclerotic renal artery disease submitted to open operative repair, factors favoring the recovery of renal function after operation have included severe preoperative hypertension, bilateral or global atherosclerotic renovascular disease due to high-grade (>90%) stenosis or renal artery occlusion, and rapidly deteriorating renal function before surgery. , , When each of these favorable features was expressed in patients considered permanently dialysis dependent, 70% of those submitted to open operative repair were permanently removed from dialysis. ,
The quality of studies designed to define the natural history of the atherosclerotic renal artery has varied widely. , Most commonly, authors have considered anatomic progression of atherosclerotic renovascular disease a certainty, one associated with an inevitable decline in kidney size and kidney function. This view has been cited to support intervention for renal artery disease whenever it is discovered, even in the absence of hypertension or renal insufficiency.
On the basis of a prospective, population-based study of progression of atherosclerotic renovascular disease in the elderly, we do not recommend “prophylactic” intervention for asymptomatic renovascular disease. This longitudinal cohort study included 119 Cardiovascular Health Study participants, with 235 kidneys for study, and no kidney progressed to a renal artery occlusion during a mean follow-up of 8.5 years. Among participants with mild to moderate hypertension in the Cardiovascular Health Study, progression to hemodynamically significant renal artery stenosis was observed in only 4%, or an annualized rate of 0.5% per year.
When a patient has bilateral renal artery stenosis and severe hypertension, the decision for empiric open renal reconstruction is based on the severity of the hypertension and the anatomy of the renal artery lesions. When disease consists of severe stenosis of one renal artery and only mild to moderate contralateral disease, it is treated as a unilateral lesion. If both renal artery lesions are moderately severe (60%–80% diameter-reducing stenosis), revascularization is undertaken only if associated hypertension is severe. In contrast, if both renal artery lesions are severe (>80% stenosis) and the patient has severe hypertension, bilateral simultaneous renal revascularization is performed, especially when excretory renal insufficiency is present. However, because the degree of azotemia usually parallels the severity of hypertension, a patient who presents with severe excretory renal insufficiency but only mild hypertension usually has concomitant renal parenchymal disease from another cause (e.g., diabetes). Characteristically, renovascular disease contributing to severe azotemia or dialysis dependence is associated with severe hypertension and severe bilateral stenosis or renal artery occlusion. , , ,
The presence of severe hypertension is considered a prerequisite for renal artery intervention, and functional studies are used to guide the management of unilateral lesions. Empiric renal artery repair is performed without functional studies when hypertension is severe, renal artery disease is bilateral, or the patient has ischemic nephropathy. , , Prophylactic renal artery repair in the absence of hypertension, whether as an isolated procedure or in combination with aortic reconstruction, is not recommended. During surgical reconstruction, all hemodynamically significant renal artery disease is corrected in a single operation with the exception of disease requiring bilateral ex vivo reconstructions, which are staged. Nephrectomy is reserved for a nonfunctioning kidney (i.e., ≤10% function by renography) with unreconstructable renal artery disease, or a kidney acting as a pressor kidney. , , Direct aortorenal reconstructions are preferred to indirect methods because concomitant disease of the celiac axis is present in 40% to 50% of patients and bilateral repair is required in half. , Failed renal artery repair is also associated with a significantly increased risk of dialysis dependence. To minimize these failures, intraoperative duplex ultrasonography is used to evaluate the technical results of surgical repair before closure.
In our experience, percutaneous management does not improve hypertension and renal function as effectively as open operative repair. Consequently we continue to advocate open operative repair for select patients. These include children with hypoplastic lesions (see Ch. 132 , Renovascular and Aortic Developmental Disorders), adults with dysplastic lesions other than medial fibroplasia, and patients with medial fibroplasia involving branch and segmental renal arteries complicated by a renal artery aneurysm. We also recommend open operative repair for atherosclerotic renovascular disease in good-risk patients, younger than 65 years of age, who demonstrate global renal ischemia manifested by critical renal artery stenosis or occlusion, especially when severe hypertension is associated with excretory renal insufficiency and rapidly deteriorating excretory function. , , Selection criteria for the repair of renal artery aneurysms are discussed in Chapter 131 (Renovascular Disease: Aneurysms and Arteriovenous Fistulae), but we have continued to consider open operative repair as opposed to coiling, stenting, or stent-grafting of these lesions.
Certain measures are used in almost all open renal artery operations. Although the data to support the use of mannitol is mixed, we favor using mannitol, and administer it intravenously in 12.5-g doses early in the operation during aortic and renal artery dissection. Repeated doses are administered before and after periods of renal ischemia, up to a total dose of 1 g/kg of patient body weight. Just before renal artery cross-clamping, 100 U/kg of heparin is given intravenously, and systemic anticoagulation is verified by activated clotting time. Unless it is required for hemostasis, protamine is not routinely administered for reversal of heparin at completion of the operation.
See Chapter 56 for Abdominal Vascular Exposures.
A midline abdominal incision is made for operative repair of atherosclerotic renal artery disease when bilateral renal artery repair or combined aortic and renal repair is planned. The patient is positioned supine with the umbilicus at the level of the table break, with the operating table flexed 10 to 15 degrees. To obtain full exposure of the upper abdominal aorta and renal branches, it is important that the last 1 or 2 cm of the proximal incision be made coursing to one side of the xiphoid, in order to release the costoxiphoid ligaments ( Fig. 128.2A ). Some type of fixed mechanical retraction is also advantageous, particularly when combined aortic and renal procedures are required. Otherwise, extended flank and subcostal incisions are reserved for correction of unilateral branch renal artery lesions or splanchnic–renal bypass.
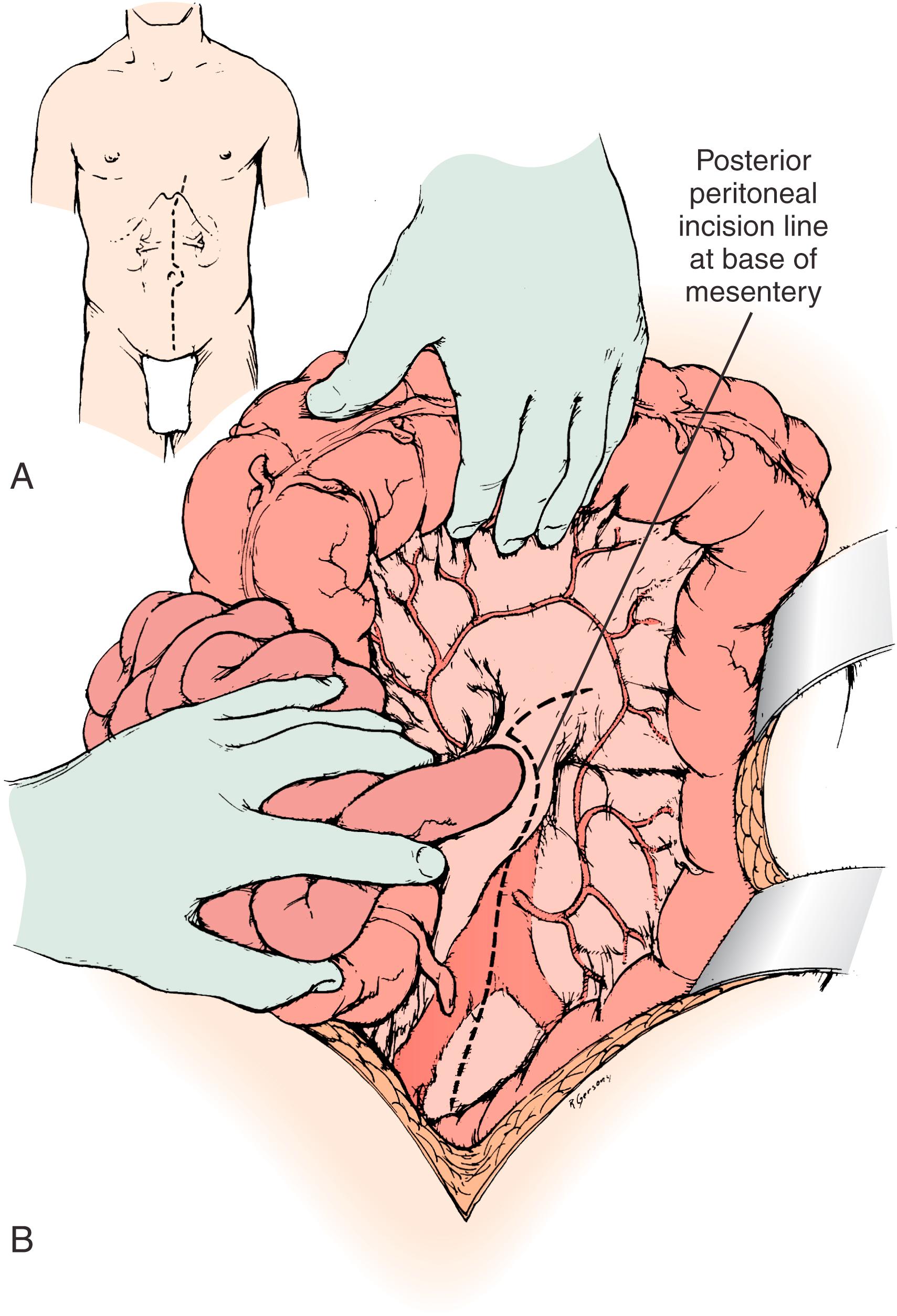
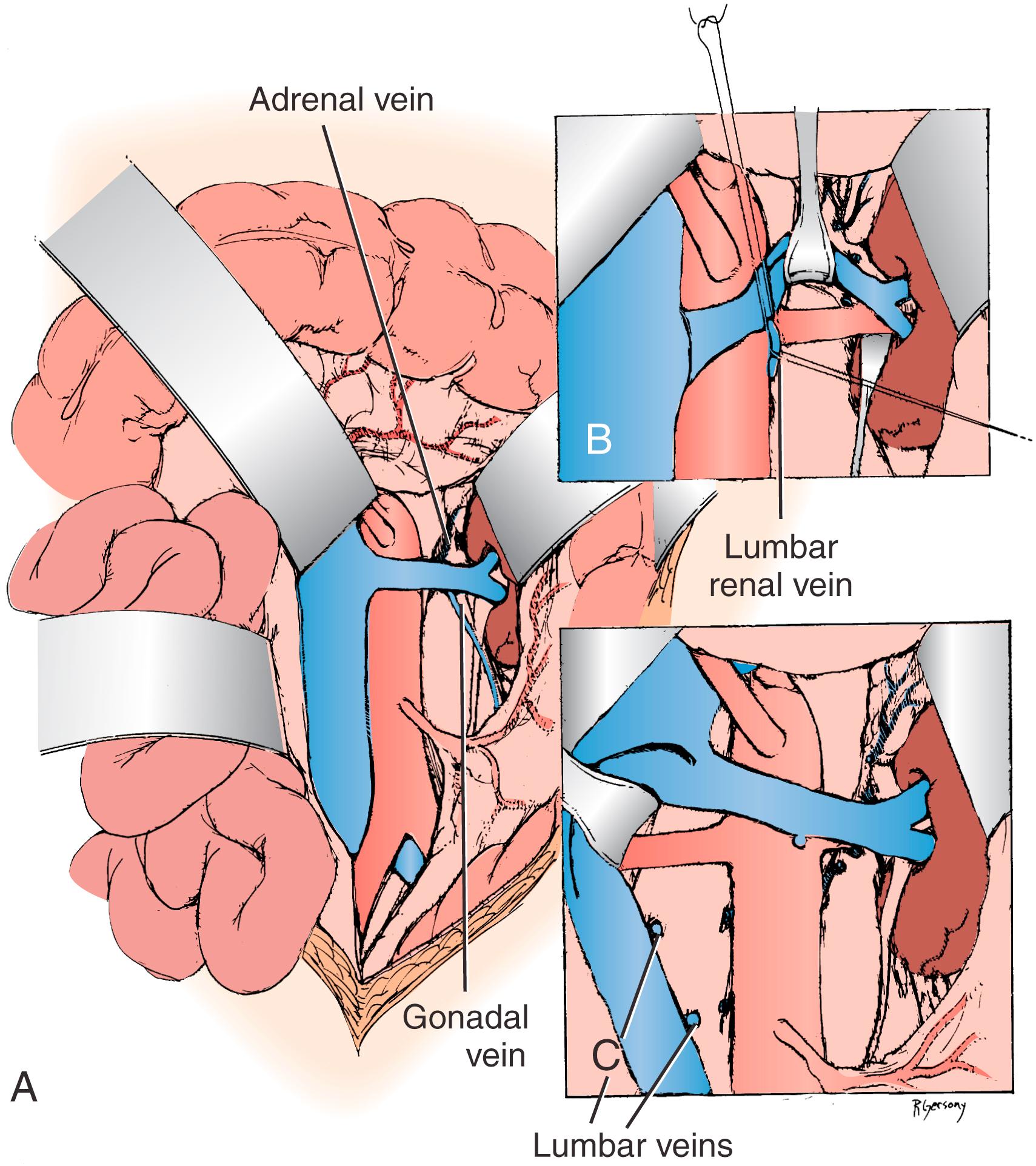
When the midline xiphoid-to-pubis incision is used, the posterior peritoneum overlying the aorta is incised longitudinally and the duodenum mobilized at the ligament of Treitz (see Fig. 128.2B ). The inferior mesenteric vein may need to be ligated to allow proximal exposure. During this maneuver, it is important to identify and spare the meandering mesenteric vessel that may be found at this level. Finally, the duodenum is reflected to the patient’s right to expose the left renal vein. By extending the posterior peritoneal incision to the left along the inferior border of the pancreas, an avascular plane posterior to the pancreas can be entered (see Fig. 128.2B ) to expose the entire left renal hilum. This exposure is of special importance when there are distal renal artery lesions to be managed ( Fig. 128.3A ). The left renal artery lies posterior to the left renal vein. In some cases, the vein can be retracted cephalad to expose the artery; in other cases, caudal retraction of the vein provides better access. Usually, the gonadal and adrenal veins, which enter the left renal vein, must be ligated and divided to facilitate exposure of the distal artery. Frequently, a lumbar vein enters the posterior wall of the left renal vein; it can easily be injured unless special care is taken (see Fig. 128.3B ). For full mobilization of the left renal vein, ligation and division of the lumbar branch is required. The proximal portion of the right renal artery can be exposed through the base of the mesentery by retracting the left renal vein cephalad and the vena cava to the patient’s right (see Fig. 128.3C ). However, mobilizing the duodenum and right colon medially best exposes the distal portion of the right renal artery; the right renal vein is mobilized and usually retracted cephalad to expose the artery.
When a branch renal artery repair is required, especially when ex vivo technique is used or when the supraceliac aorta is used as an inflow source for aortorenal bypass, an extended flank incision is useful. With the ipsilateral flank bumped, the incision extends from the opposite semilunar line into the flank, bisecting the abdominal wall between the costal margin and iliac crest. A left or right visceral mobilization allows access to the renal vasculature and the aortic crus. The crus can be divided, and an extra-pleural dissection of the descending thoracic aorta can provide access to the T9–10 thoracic aorta for proximal control and anastomosis. ,
Whether right or left branch renal artery exposure is required, the key is creation of the correct dissection plane between the mesentery anteriorly and Gerota’s fascia posteriorly. The renal vein is identified first and mobilized from inferior vena cava (IVC) origin to renal hilum. On the right, small venous branches at the junction with the vena cava require ligation. The adrenal, gonadal, and lumbar branches on the left may be sacrificed to facilitate exposure.
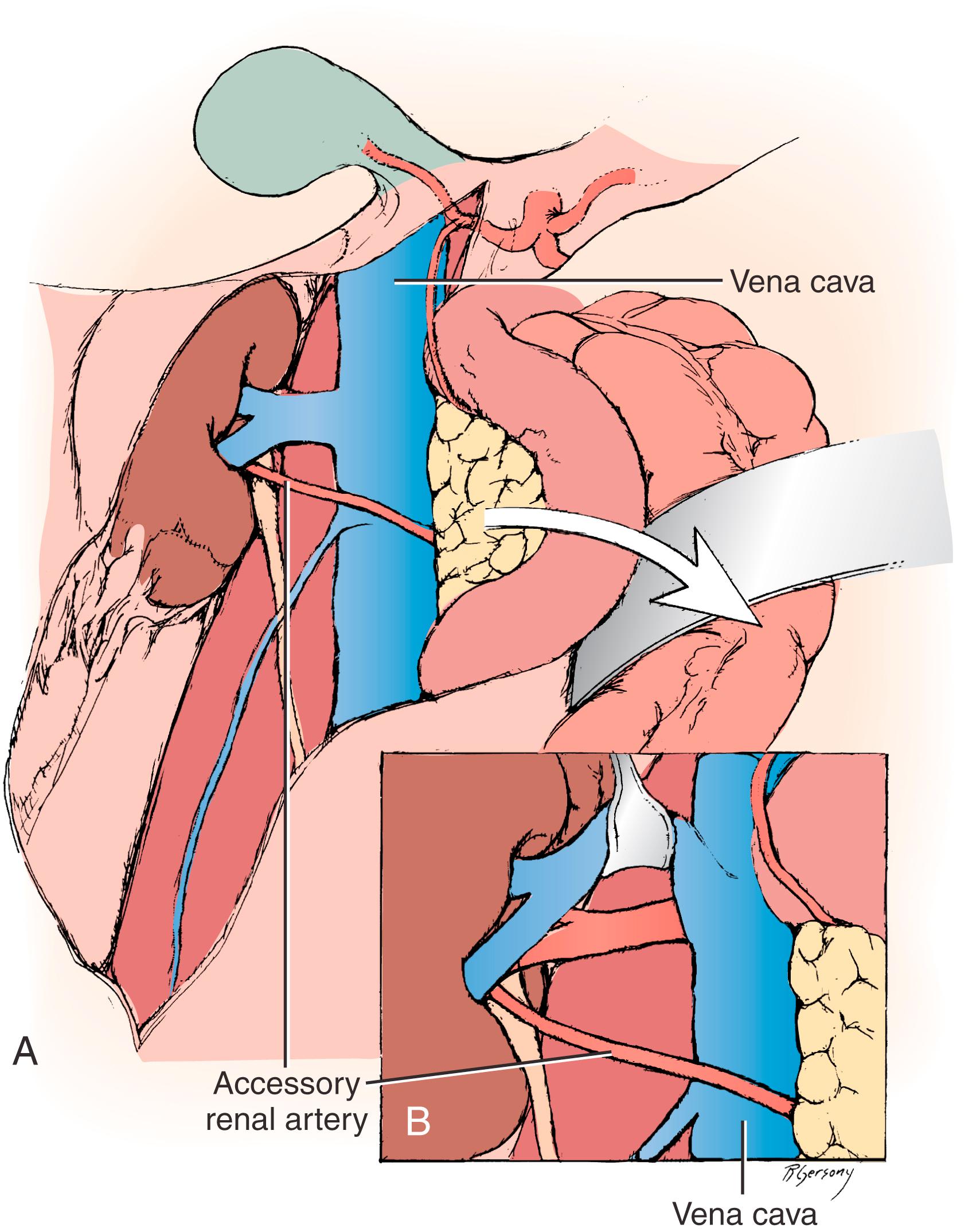
Branch renal artery exposure on the right is achieved by colonic and duodenal mobilization. First, the hepatic flexure is mobilized at the peritoneal reflection ( Fig. 128.4 ). With the right colon retracted medially and inferiorly, a Kocher maneuver mobilizes the duodenum and pancreatic head to expose the IVC and right renal vein (see Fig. 128.4A ). Typically, the right renal artery is located just inferior to the accompanying vein, which can be retracted superiorly to provide the best exposure. Although accessory vessels may arise from the aorta or iliac vessels at any level, all arterial branches coursing anterior to the IVC should be considered accessory right renal branches and carefully preserved (see Fig. 128.4B ).
A variety of open operative techniques have been used to correct renal artery disease, but three basic operations have been used most frequently: aortorenal bypass, renal artery thromboendarterectomy, and renal artery reimplantation. No single approach provides optimal repair for all types of renovascular lesions in all patients. Aortorenal bypass using saphenous vein is probably the most versatile technique; however, transaortic thromboendarterectomy is especially useful for orificial atherosclerosis involving multiple renal arteries, or in association with juxtarenal aortic procedures. On occasion, the renal artery will demonstrate sufficient redundancy to allow reimplantation; this is probably the simplest technique and one that is particularly appropriate to hypoplastic renal artery lesions in children (see Ch. 132 , Renovascular and Aortic Developmental Disorders). ,
Three types of materials are typically used for aortorenal bypass: autologous saphenous vein, autologous hypogastric artery, and synthetic graft. The decision as to which graft should be used depends on a number of factors. In most instances, the authors prefer the saphenous vein for older adults. However, if the vein is small (<4 mm in diameter) or sclerotic, the hypogastric artery or a synthetic graft may be preferable. In addition, vein enlargement can be anticipated in virtually all young adults. Although structural immaturity has been cited for enlargement and aneurysmal degeneration when saphenous vein is used for renal artery reconstruction in children, the normal renal blood flow in the young resembles that of an arteriovenous fistula with continuous forward flow. This fact alone may account for vein enlargement in the young patient with normal renovascular resistance. In lieu of vein, a 6-mm thin-wall polytetrafluoroethylene (PTFE) graft is satisfactory when the distal renal artery is of sufficient caliber (≥4 mm). Although we do not use them in our practice, polyethylene terephthalate (Dacron) grafts (6 mm) have also been used with success. Hypogastric artery autograft is preferred for aortorenal bypass in children when reimplantation is not possible. , , ,
End-to-side distal anastomoses are occasionally used to include polar renal arteries. In this instance, an end-to-side anastomosis between the polar renal artery and the graft is performed after the proximal aortic anastomosis. After the end-to-side anastomosis has been completed, the most distal main renal artery reconstruction is made in an end-to-end fashion ( Fig. 128.5 ).
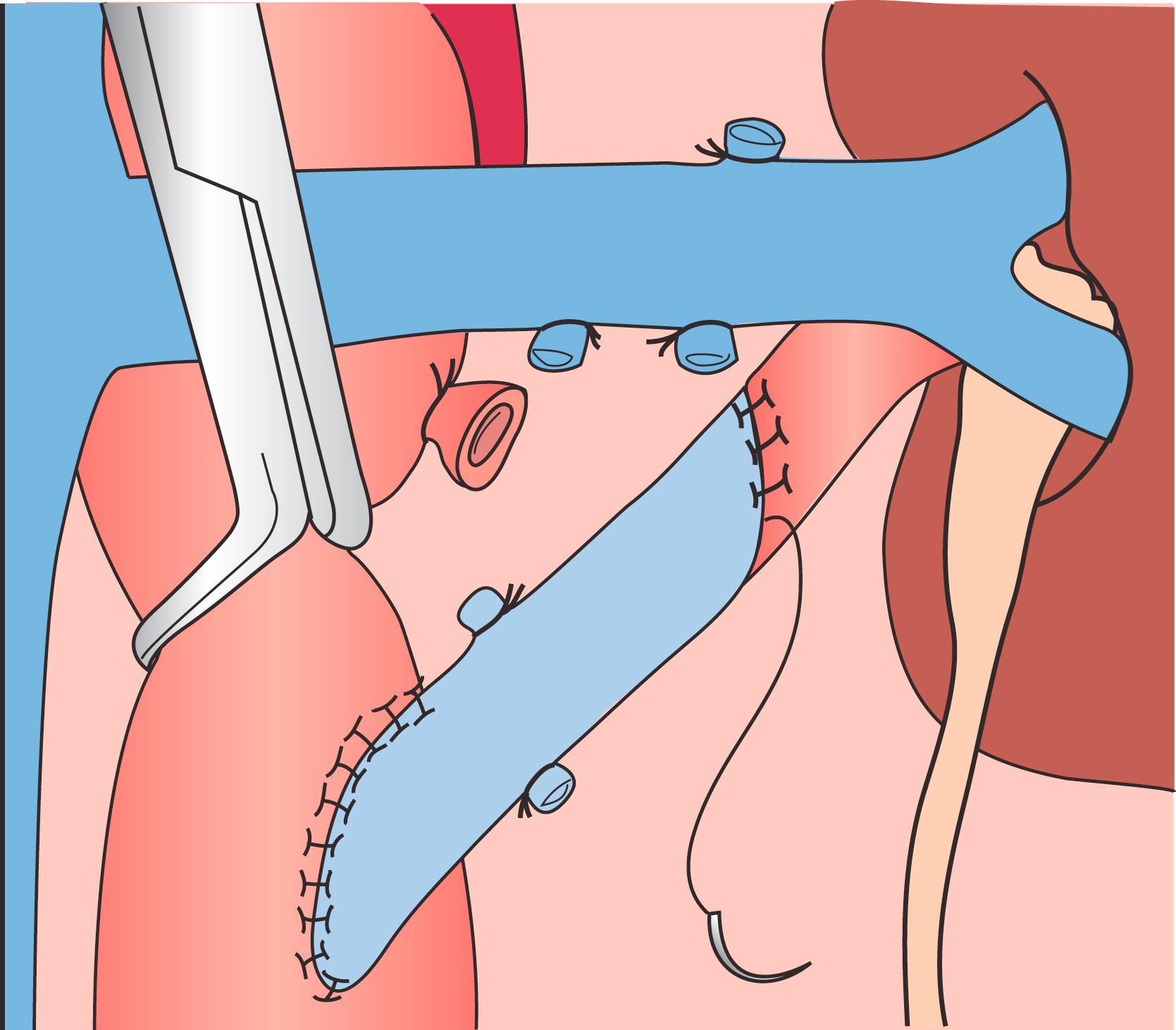
In creating the distal anastomosis, the length of the arteriotomy should be at least three times the diameter of the renal artery so as to reduce the complication of late anastomotic stenosis. An anastomosis with 7-0 monofilament polypropylene as a continuous suture is created with loupe magnification. Just before completion of the renal artery anastomosis, the occluding clamps are temporarily removed to flush air and small debris. When renal artery bypass can be accomplished in less than 40 minutes, cold perfusion preservation is not required. The aortic anastomosis is performed first, removing an ellipse of the anterolateral aortic wall. This is especially important when the aorta is relatively inflexible because of atherosclerotic involvement. A 4.0-mm aortic punch applied two or three times creates a satisfactory ellipse in most instances. In combined aortorenal reconstructions, the proximal anastomosis is performed first with a thin-wall 6-mm PTFE graft for renal artery bypass attached in end-to-side fashion to the larger polyester aortic graft. The distal aortic reconstruction is completed, and the distal renal anastomosis is created as the last step.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here