Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Trauma is the most common cause of death and disability for children in the United States, with up to half of injuries resulting in long-term sequelae. Children with multiple injuries present particular challenges to both their families and the medical teams that care for them. The rehabilitation goal for children with multiple injuries is to maximize function and return them to their home and community as soon as possible. The purpose of this chapter is to review the important aspects of rehabilitation treatment in this setting.
Multidisciplinary care and early rehabilitation are essential to optimize outcomes of children with polytrauma, spinal cord injury, or traumatic brain injury.
Criteria for inpatient rehabilitation include the need for moderate/maximum assistance, the ability to participate in 3 hours of therapy per day, the ability to follow at least simple commands, and the need for at least two different therapies.
Spasticity should be classified as localized or generalized and graded by severity.
Psychologic rehabilitation of an injured child is as important as the physical rehabilitation.
Inpatient rehabilitation plays an integral role in the recovery of patients following a severe trauma or a disabling illness. Admission to an inpatient rehabilitation facility is indicated for patients requiring moderate to maximum assistance due to deficits in mobility, function, cognition, and/or speech. The majority of patients meeting criteria have sustained severe head injuries. Admission is also considered for patient with multiple fractures but no central nervous system involvement to become facile with orthoses and adaptive equipment. Patients must be able to participate in 3 hours per day of therapy and follow at least simple commands, although patients with lower levels of function may be admitted to specialized disorders of consciousness programs. Patients must also be medically stable before transfer from the hospital.
Candidates for inpatient rehabilitation need at least two different therapies, such as physical therapy, occupational therapy, speech therapy, or cognitive therapy, for insurance companies to provide approval. Insurance authorization typically takes 3 days for commercial insurance and 7 days for public insurance. Thus, patients with private insurance are more likely to receive inpatient rehabilitation and have a shorter hospital stay before admission. Although children are often transferred a long distance to trauma centers for acute care, efforts should be made to find a rehabilitation facility close to the family’s home. However, some trauma centers also have inpatient rehabilitation services, and the continuity between patients and their initial care team is likely beneficial.
The rehabilitation team consists of members from physiatry, physical therapy, occupational therapy, speech therapy, orthotics, nutrition, psychology, psychiatry, social work, and case management. The team is usually led by a physiatrist. Communication between the rehabilitation team and the orthopedist is critical, particularly at the beginning of therapy, to define weight-bearing or range and motion restrictions. Fractures do not have to be completely healed before admission, but achieving the benefits of therapy is facilitated by greater fracture stability. If a child is non-weight-bearing on more than two limbs, it is often better to delay rehabilitation until this restriction is lifted.
The goals of inpatient rehabilitation are to increase the child’s level of function to transition to outpatient rehabilitation. Programs also teach families how to care for their injured child and facilitate integration back into the community. Length of stay is influenced by the underlying condition, functional status, insurance, and psychosocial factors. The median length of stay in rehabilitation is 32 days for spinal cord injury (SCI), 26 days for traumatic brain injury (TBI), and 13 days for orthopedic conditions. A lack of available stepdown (subacute or chronic) rehabilitation facilities may contribute to longer lengths of stay.
Although inpatient rehabilitation leads to improvements in quality of life and function for the majority of patients, residual disability requiring further care (particularly in patients with SCI or TBI) is often present at discharge. The transition from inpatient rehabilitation to outpatient management is stressful, and families may be overwhelmed by the complexity of care for their previously healthy child. Families may even feel abandoned by the healthcare system. Therefore, proper discharge from inpatient rehabilitation is essential. Phone calls after discharge from a rehabilitation nurse can facilitate difficulties with appointments, medications, and equipment.
Successful rehabilitation not only results in returning the child to their home but also into their school and community. In adolescents who are of driving age, a driver’s capacity evaluation should be done to assess the patient’s safety and ability to drive. Children who require prolonged rehabilitation will have their schooling interrupted, in many cases for an extended period. This interruption in schooling may put them significantly behind the level of their peers, which adds to their problems when they are ready to return. It is important to initiate schooling and tutoring as soon as the patient’s condition allows while recognizing that the duration of tutoring may be lengthy. Potential barriers for attending school are identified and addressed by the rehabilitation team in advance, and communication with the school regarding the child’s needs is essential.
Fractures are typically immobilized during the protection phase of rehabilitation to allow adequate healing. However, it is important to consider fracture and fixation stability to avoid excessive immobilization that delays rehabilitation. Therapy then progresses to controlled range of motion (ROM). Although isolated fractures in children often return to full ROM on their own, ROM and physical therapy are critical for patients with head injuries, spine injuries, or multiple fractures to avoid joint contractures. Communication between the orthopedist and therapist facilitates rehabilitation at the proper pace.
Active ROM exercises (movement generated by the patient) are performed if possible. These are facilitated by active-assistive ROM exercises that consist of having the child actively move through as much of the range as possible and then passively completing as much movement as possible through the normal range. The use of body weight often increases the effectiveness of ROM exercises. For example, the best stretch of the gastrocnemius muscles is obtained when the patient is standing. Children are encouraged to participate in their ROM exercise program, and young children may be able to perform simple stretches if properly supervised. Passive ROM is performed if the child is too young, weak, or unable to cooperate. Standards for full and functional ROM have been established ( Table 22.1 ).
| Joint | Degrees of Normal (and Functional) Range of Motion |
|---|---|
| Shoulder | |
| Abduction | 180 (120) |
| Adduction | 45 (30) |
| Flexion | 180 (120) |
| Extension | 60 (40) |
| Internal rotation (arm in abduction) | 80 (45) |
| External rotation (arm in abduction) | 90 (45) |
| Elbow | |
| Flexion | 140–160 (130) |
| Extension | 0–5 (−30) |
| Supination | 80–90 (50) |
| Pronation | 70–80 (50) |
| Wrist | |
| Flexion | 75 (15) |
| Extension | 70 (30) |
| Radial deviation | 20 (10) |
| Ulnar deviation | 35 (15) |
| Hip | |
| Flexion | 125–128 (90–110) |
| Extension | 0–20 (0–5) |
| Abduction | 45–48 (0–20) |
| Adduction | 40–45 (0–20) |
| Internal rotation | 40–45 (0–20) |
| External rotation | 45 (0–15) |
| Knee | |
| Flexion | 130–140 (110) |
| Extension | 0 (0) |
| Ankle | |
| Plantar flexion | 45 (20) |
| Dorsiflexion | 20 (10) |
| Inversion | 35 (10) |
| Eversion | 25 (10) |
After additional fracture healing is well established, therapy then transitions to strengthening exercises. These exercises usually involve extremely simple equipment such as a ball, putty, or exercise band. Strengthening programs may also include isometric exercises, which maintain muscle length with increasing tension during contraction, or isotonic exercises with muscle shortening and steady tension. Isotonic exercises include open kinetic chain exercises, such as with free weights, and closed kinetic chain exercises, such as with pulley systems. Closed kinetic chain exercises are often favored in the early postinjury period because they provide a more predictable path of movement. During this phase, progress is also made with balance and proprioception exercises. Sports-specific and functional training are also helpful before return to activities. Return to play is not allowed until pain relief, full strength, and full ROM have been restored.
Casts and braces for fracture healing are discontinued as soon as possible to facilitate recovery. Lower extremity orthoses are often prescribed for abnormal gait dynamics in patients with associated spinal cord or TBI. These orthoses are named according to the region of the body that they help control, such as ankle-foot orthoses and knee-ankle-foot orthoses. Generally, the more joints controlled by the orthosis, the bulkier it becomes and the greater the potential to interfere with balance, gait, and function.
Adaptive devices can be helpful in extending reach, providing grasp, reducing force, and improving safety. Examples include reachers, sock aids, a long-handled sponge or shoe horn, grooming aids, built-up feeding utensils, a rocker knife, a raised toilet seat, tub chair, and built-up door handles ( Fig. 22.1 ). Velcro or elastic shoe closures also may be helpful. Such devices can provide increased independence in activities of daily living including feeding, dressing, bathing, grooming, and toileting. Evaluation by an occupational therapist is valuable for problem-solving to increase independence and quality of life during recovery.
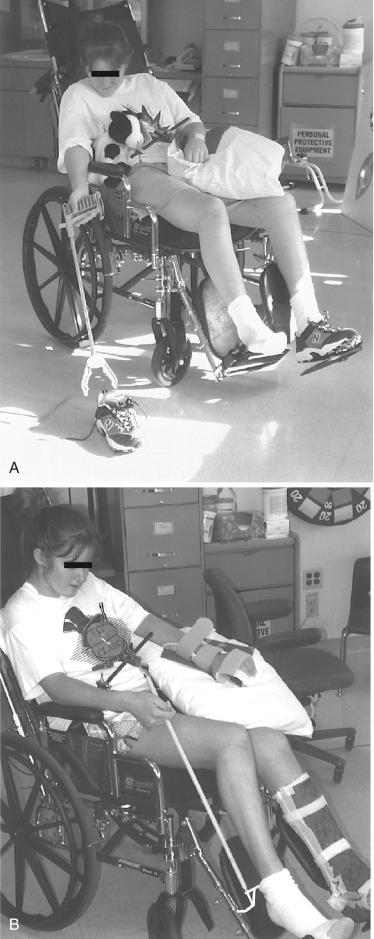
Gait aids are prescribed taking into account the child’s function and any cognitive or balance limitations. These aids may be useful for a child with weight-bearing restrictions on the lower extremity. Initial crutch training is needed to prevent axillary irritation and injury from falls. A child who requires additional support because of instability or reduced lower extremity strength may require a walker. For patients with concurrent wrist or hand injuries, the walker or crutches can be modified with an upper extremity platform support to distribute the weight through the forearm and elbow. Wheelchairs are used if both lower extremities are involved or the patient cannot comply with weight-bearing restrictions. A sliding board may be helpful in increasing a child’s independence in transfers for children who can weight bear on more than two limbs. Otherwise, a lift is prescribed, and caregivers are taught how to perform transfers.
Adequate pain control in children after sustaining multiple fractures is required for successful rehabilitation. Providing a description of their pain is difficult for preschool-age children who do not possess the language ability or the understanding to correctly identify the location and characteristics of the pain. Pain management is facilitated by using age-specific objective measurement scales based on expressive capability to quantify pain levels. The Children’s Hospital of Eastern Ontario Pain Scale and the Objective Pain Scale are used in infants and very young children. For children 3 to 6 years of age, visual progression of happy to sad faces such as the McGrath Facial Affective Scale and Beyer Oucher Scale are frequently used. Older children have improved abstract and numeric reasoning and may be able to use more adult measures, such as the visual analog scale. Inadequate pain control should be included in the differential diagnosis of unexplained agitation or vital sign changes such as tachycardia or hypertension in patients who are uncommunicative because of age or neurologic insult.
Pain relief should not be achieved with the indiscriminate use of narcotics. It has been shown that nonopioid analgesics such as acetaminophen and ibuprofen are as effective as opioids for acute fracture pain management. In addition, ibuprofen is also as effective as morphine for postoperative management following minor orthopedic procedures. However, for a multiply injured child, pain may be an ongoing problem such that narcotics are required. In this setting, efforts are made to slowly wean the child from the opioids while managing their side effects. Weaning is often started by switching to longer-acting medications.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here