Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Understand the importance of food intake to clinical medicine.
Discuss the role of the nervous system in the regulation of food intake.
Explain the role of the endocrine system in the regulation of metabolism and food intake.
Discuss the role of the gastrointestinal (GI) system in the regulation food intake.
Understand how input from the nervous, endocrine, and GI systems is integrated to regulate food intake and metabolism.
Discuss the various treatments for obesity.
The human species evolved during a time when the source of the next meal was highly uncertain. As a result, the gastrointestinal (GI) tract evolved to optimize the processing of ingested material when it became available. Receptive relaxation allows the stomach to accommodate large volumes with minimal increases in gastric pressure. Digestive enzymes are secreted in great excess. The secretion of pancreatic lipase, for example, must be reduced by at least 80% before steatorrhea occurs. There is significant overlap in the specificity of transport proteins or carriers for the absorption of most amino acids. Indeed, even the absorptive surface of the small intestine can be reduced 60% to 70%, as long as sufficient ileum remains to reabsorb bile acids and to absorb vitamin B 12 , before increased amounts of nutrients appear in the stool.
The result is that virtually all ingested carbohydrate, protein, and fat are broken down and absorbed. It is impossible to saturate the digestive and absorptive capacities of the GI tract. This situation was advantageous when acquiring a meal was uncertain and also required an expenditure of calories in the form of exercise, but now that the nearest meal is available by opening the refrigerator door or, worse, pulling into the parking lot of the nearest convenience store or fast food restaurant, the result is an epidemic of obesity with its sequelae of diabetes, cardiovascular disease, and some forms of cancer.
At present, more than two-thirds of Americans are overweight, and one-third can be classified as obese. The prevalence of obesity in children has increased markedly. Obesity has now displaced cigarette smoking as the number one health problem in the nation. In the United States approximately 300,000 deaths per year are directly attributed to obesity. In rare cases obesity can be caused by a gene mutation, but in an overwhelming majority of instances obesity is the result of a long-term imbalance between intake and expenditure of calories. These two quantities must remain equivalent to maintain body weight. Although a certain amount of weight control can be effected by increasing caloric expenditure in the form of exercise, the fact of the matter is that most of us overeat.
In view of the recognized importance of normal body weight for maintaining health, an understanding of the mechanisms regulating food intake seems imperative. Current knowledge of the regulation of food intake is far from complete, however, and only in the past few years has sufficient evidence been accumulated for inclusion in a textbook of GI physiology. In fact, knowledge about this aspect of the field lags far behind that on the topics covered in other chapters of this book. Another significant difference between this subject and those of the other chapters is that the regulation of food intake depends heavily on contributions from systems other than the digestive system—namely, the endocrine and nervous systems.
Signals affecting food intake are integrated in the brain. These signals include emotions and learned behavior, as well as hormonal and neural input from the endocrine system and the GI tract. Input provides information regarding total energy stores and the presence of nutrients within the digestive tract. In addition, the vagus nerve relays input regarding gastric distention, secretory activity, and the release of various hormones from the stomach and duodenum.
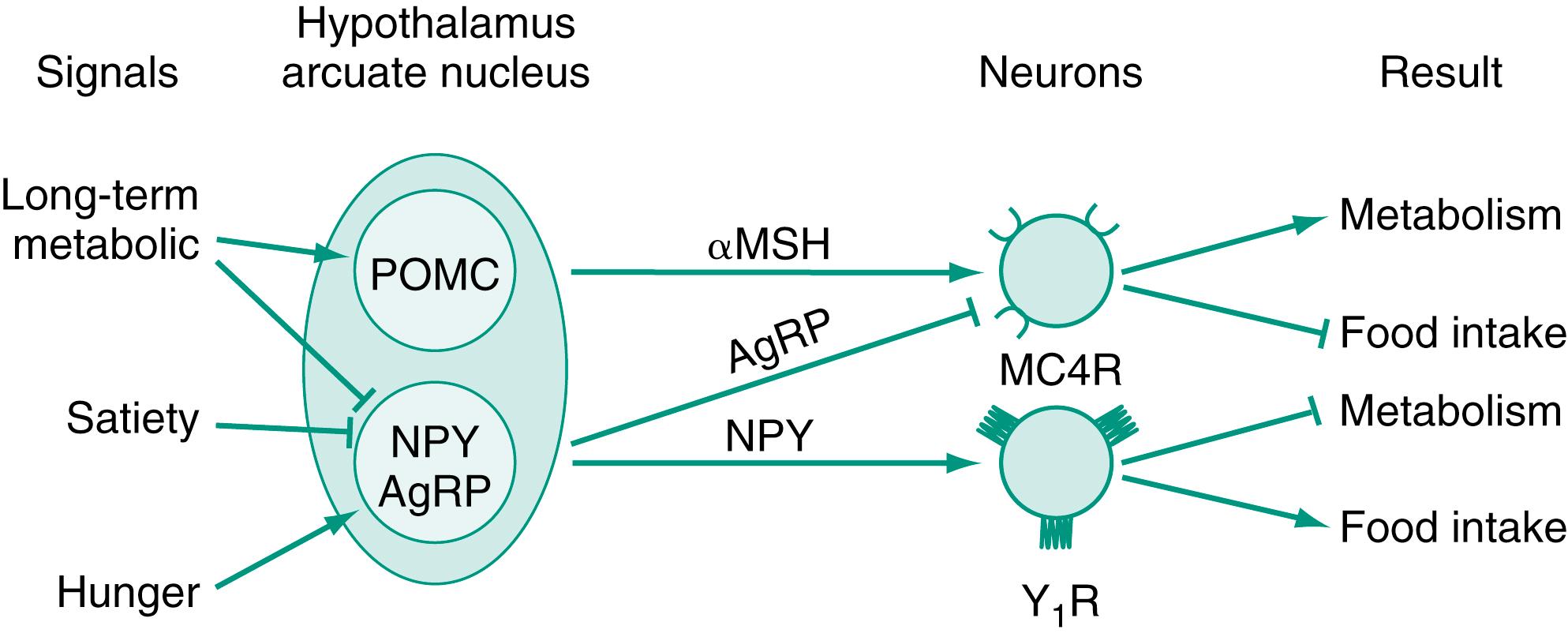
Most of the integration of signals affecting food intake takes place in the arcuate nucleus of the hypothalamus. Two pathways exist: one inhibiting food intake and increasing metabolism and the other stimulating food intake and inhibiting metabolism ( Fig. 13.1 ). The melanocortin pathway is made up of appetite-inhibiting neurons containing proopiomelanocortin (POMC), which releases α-melanocyte-stimulating hormone (α-MSH). α-MSH binds melanocortin receptors (MC4), present on second-order neurons, to inhibit food intake and increase the rate of metabolism. The stimulation of feeding is provided by the neuropeptide Y (NPY) pathway. Hunger signals stimulate the release of NPY, which binds to Y1 receptors to increase feeding behavior and the storage of calories. It would make little sense for both these pathways to be operating at the same time, and the NPY system also releases agouti-related peptide (AgRP), which is an antagonist of the MC4 receptor. In addition, peptides that stimulate the melanocortin system inhibit the NPY system. Some cases of obesity in humans have been traced to mutations in the POMC and MC4R genes. Approximately 5% of cases of childhood obesity have been linked to MC4R mutations.
The enteric nervous system plays a profound part in the regulation of GI motility and secretion. Its receptors sense different chemicals present in foodstuffs, changes in muscle tension, and various peptides released from endocrine cells and nerves present in the gut. Approximately 75% of vagal fibers are afferent, and much of this information is relayed to vagal nuclei in the brain. In some cases this input causes an efferent signal also relayed by vagal nerves that results in a change in gut function—a so-called vagovagal reflex.
Most afferent vagal fibers pass through the nodose ganglion and terminate in the nucleus tractus solitarius (NTS) of the hindbrain. The hindbrain is able to regulate food intake in response to peripheral signals if input from higher centers is surgically eliminated. Several peptides that stimulate satiety and decrease feeding are known to activate receptors present on vagal afferents . In addition, the vagus nerve relays signals initiated by distention of the stomach. Vagal signaling to the NTS is integrated with information received by the hypothalamus to produce the appropriate responses in feeding behavior and metabolism. Experiments in which vagal afferent activity was blocked either chemically or surgically demonstrated the importance of this pathway in the overall regulation of food intake. In these studies, the inhibition of sham feeding by nutrient infusion was prevented; the amount of material in the stomach no longer influenced meal size; and the effects of satiety hormones were eliminated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here