Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The nationally reported revision rate for primary rhinoplasty ranges from 8% to 15%. Unfortunately, there will likely never be a shortage of patients requiring revision rhinoplasty. Experienced surgeons consistently achieve a high level of satisfaction among their patients. Still, complications can occur despite technically well-performed surgery. All surgeons have complications.
Success in rhinoplasty is based on well-developed judgment, wisdom, and accumulated knowledge and experience. Similar to most surgeries, rhinoplasty is a science and an art. Skill comes from experience and wisdom, combined with a measure of talent, and the surgeon must have a detailed understanding of the multiple anatomic variants encountered. The surgeon also must have accumulated the appropriate surgical techniques and experience. Specifically, the surgeon must acquire knowledge of the surgical alternatives, and how healing forces will affect the final surgical outcome. This skill set is only acquired by careful follow-up of patients operated over time.
There is no “standard” rhinoplasty. Each operation is unique in that it must be tailored to the specific anatomic components involved and the desires of the patient. By developing a consistent, meticulous routine in which the patient's nose is analyzed with regard to its anatomic components and their complex interrelationships, the surgeon can best select the appropriate incisions, approaches, and techniques for the patient's nose. These concepts are discussed in the first part of this chapter.
Having the opportunity in practice to examine numerous revision rhinoplasty patients from across the United States and around the world, the senior author has observed a wide range of problems. By carefully studying the problems encountered in a revision practice, the rhinoplasty student can improve their ability to address problems encountered during both primary and revision rhinoplasty. With this in mind, for the second part of this chapter the senior author selected problems encountered in the course of his revision practice which warrant highlighting. The selected problem patterns are either encountered frequently or illustrate specific surgical techniques that may be particularly useful in the rhinioplasty surgeon's armamentarium.
Although the anatomy of the nose has been fundamentally understood for many years, only relatively recently has there been an increased understanding of the long-term effects of surgical changes upon the function and appearance of the nose. A detailed understanding of nasal anatomy is critical for successful rhinoplasty. Accurate assessment of the anatomic variations presented by a patient allows the surgeon to develop a rational and realistic surgical plan. Furthermore, recognizing variant or aberrant anatomy is critical to preventing functional compromise or untoward aesthetic results.
The development of nasal and facial analysis skills is an important part of the effort to reduce the risk of complications. Nasal and facial analysis requires an understanding of the concept of the “aesthetic ideal.” A nose that is considered “ideal” is one that is harmonious with a patient's other favorable facial features. This of course will vary to a certain degree depending upon a patient's gender and ethnicity. Indeed, our perception of beauty helps define what makes an ideal shape for a female or male nose, so there is also always a slight artistic element to this concept. While the “aesthetic ideal” cannot be completely boiled down to simple lines and numbers alone, guidelines or proportions do exist that represent an aesthetic ideal. Examples include the nasolabial angle, the nasofrontal angle, the nasomental angle, and others. Artists have long made studies of beauty and aesthetic proportions and, today, facial plastic surgeons must similarly understand beauty in order to make changes that can enhance their patients' facial harmony and beauty. A detailed study of nasal and facial anatomy, and the ideal aesthetic proportions, is recommended.
Detailed anatomic analysis of the nose is an essential first step in achieving a successful surgical outcome. The study of nasal anatomy in the unoperated and in the operated nose is a lifetime learning endeavor. The surgeon constantly seeks to add to his or her knowledge of the anatomic variants, and the problems that can occur. The senior author's approach to nasal analysis in a primary and secondary rhinoplasty is described ( Tables 9-1 and 9-2 ). The preoperative analysis in revision rhinoplasty carries the additional layer of complexity of a prior surgical intervention, with subsequent distortion of the preexisting anatomy.
| General |
|
| Frontal View |
|
| Base View |
|
| Lateral View |
|
| Oblique View |
|
| General |
|
| Frontal |
|
| Base |
|
| Lateral |
|
| Oblique |
|
Studying all standard preoperative photographic views for rhinoplasty (frontal, base, lateral, oblique) allow a systematic, detailed anatomic analysis that complements the physical examination process.
Analysis begins by examining all four views and making an assessment of the overall stature of the patient, the facial skin quality, and the symmetry of the face. The principle of dividing the face into horizontal thirds and vertical fifths is a useful tool to obtain a general sense of any areas of the face that may play a key role in nasal appearance and the outcome of nasal surgery. It is essential that these incongruent areas or asymmetries be recognized and discussed with the patient preoperatively. Thickness and quality of the facial skin–subcutaneous tissue complex must be determined, as it plays a critical role in dictating the limitations of what can and cannot be accomplished with aesthetic nasal surgery.
After completing the general assessment, the surgeon should note and highlight the most striking characteristics of the nose. These are typically the characteristics that bring the patient for rhinoplasty, such as excessive size, deviation, or a dorsal hump. These primary patient concerns must be recognized, highlighted, and addressed above all else.
As the surgeon reviews each photographic image, the major aesthetic and technical points that can be evaluated on a given view are noted first. Subtleties in analysis are then addressed. It is important to recognize both the characteristics of greatest concern to the patient and the more subtle findings. The patient may not notice these other subtle abnormalities if they are left unaddressed by the surgeon. Postoperatively, the scrutinizing patient may notice and point out these abnormalities. Stepwise, methodical analysis of the patient and all photographic views allows the well-trained surgeon to identify key anatomic and aesthetic points to be addressed.
As the preoperative analysis proceeds in revision rhinoplasty, a critical question that guides examination of each area is, “Was it underresected, overresected, asymmetrically resected, or appropriately treated?” Any unoperated areas of the nose are identified. Also, the presence of possible grafts or implants is considered throughout the examination. For a detailed discussion of analysis, further reading and study are recommended.
Anterior rhinoscopy should be undertaken in the rhinoplasty patient and may identify abnormalities such as deviated septum, inferior turbinate hypertrophy, synechiae or scar bands, septal perforation, and other abnormalities. Examination also includes nasal endoscopy when there are functional nasal complaints, such as nasal obstruction ( Figure 9-1 ). If indicated, a sinus computed tomography scan may also be obtained.

Pownell et al. described diagnostic nasal endoscopy in the plastic surgical literature. They trace the historical development of nasal endoscopy, explain its rationale, review anatomic and diagnostic issues including the differential diagnosis of nasal obstruction, and describe the selection of equipment and correct application of technique, emphasizing the potential for advanced diagnostic potential.
Levine reported that 39% of patients with a complaint of nasal obstruction had findings on endoscopic examination that were not identified with traditional rhinoscopy. Many of Levine's patients had seen other physicians for this problem and had not received appropriate treatment.
Becker et al. described that, in patients seeking cosmetic nasal surgery who also had nasal obstruction, nasal endoscopy allowed the diagnosis of additional pathology not seen on anterior rhinoscopy, including obstructing adenoids, enlarged middle turbinates with concha bullosa, choanal stenosis, nasal polyps, and chronic sinusitis ( Figure 9-2 ). In their series, additional surgical therapy was undertaken in 28 of 96 rhinoplasty patients due to findings on endoscopic exam. Thirteen patients underwent endoscopic sinus surgery. Nine patients had a concha bullosa requiring partial middle turbinectomy. Three patients—all revision surgeries—had persisting posterior septal deviation requiring endoscopic septoplasty. Two patients underwent adenoidectomy. One patient required repair of choanal stenosis.
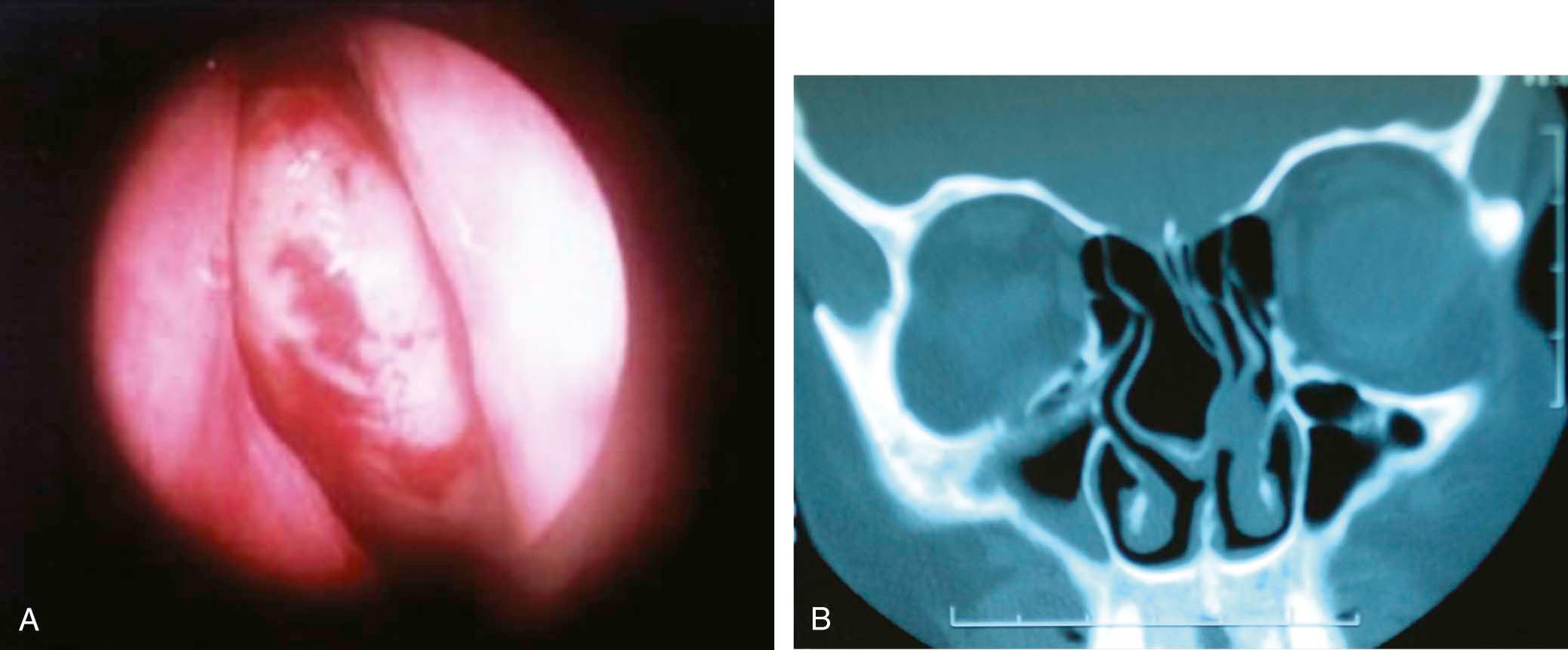
Static and dynamic nasal valve collapse are commonly encountered in revision rhinoplasty patients. In Becker et al.'s report, 19 of 21 patients with nasal valve collapse reported a past history of rhinoplasty.
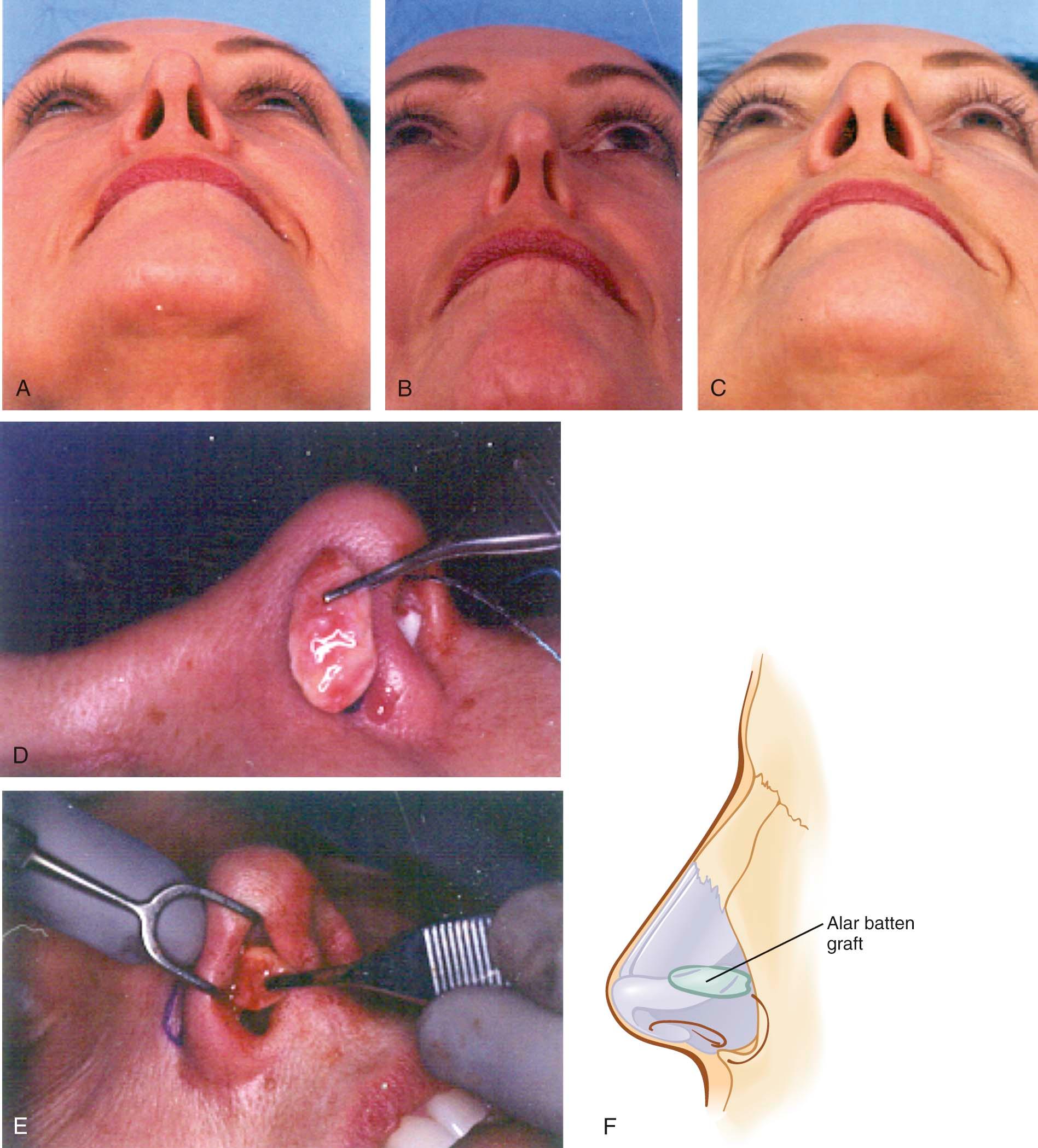
Pinching of the nasal sidewall and alar retraction are hallmarks of nasal valve collapse. Observing the patient performing normal and deep nasal inspiration may lead directly to the diagnosis of nasal valve collapse ( Figure 9-3 ). A “modified” Cottle maneuver, in which the lateral nasal sidewall is supported and elevated slightly with a cerumen curette or similar device, is strongly supportive of the diagnosis when the maneuver results in the patient's report of significant subjective improvement in nasal breathing.
Incisions are methods of gaining access to the bony and cartilaginous structures of the nose and include transcartilaginous, intercartilaginous, marginal, and transcolumellar incisions. Approaches provide surgical exposure of the nasal structures including the nasal tip and include cartilage-splitting (transcartilaginous incision), retrograde (intercartilaginous incision with retrograde dissection), delivery approach (intercartilaginous and marginal incisions), and external (transcolumellar and marginal incisions). After analyzing the individual patient's anatomy, appropriate incisions, approaches, and tip-sculpturing techniques may be selected.
The selection of the planned incisions, approaches, and surgical techniques for a particular patient is of course the central decision of the rhinoplasty process. An operative algorithm may provide a helpful starting point in selecting the incisions, approaches, and techniques used in nasal surgery. In every case, the patient's anatomy dictates the selection of an appropriate technique. As the anatomic deformity becomes more abnormal, a graduated, stepwise approach is taken. However, other factors, such as the need for spreader grafts, complex nasal deviation, surgeon preference, and other factors may also appropriately affect the ultimate selection of approach.
The endonasal approaches may be generally preferred for patients requiring conservative profile reduction, conservative tip modification, selected revision rhinoplasty patients, and other situations in which conservative changes are being undertaken. Advantages of less invasive approaches include less dissection, less edema, and less “healing.” However, less invasive approaches provide by their very nature less exposure, which in some cases may be a disadvantage.
Indications for external rhinoplasty approach generally include asymmetric nasal tip, crooked nose deformity (lower two thirds of nose), saddle nose deformity, cleft-lip nasal deformity, secondary rhinoplasty requiring complex structural grafting, and septal perforation repair. Other indications may include complex nasal tip deformity, middle nasal vault deformity, and selected nasal tumors. Some surgeons prefer the open approach for less complex nasal tip deformities due to the precision that they believe it offers them, in their hands, compared to the endonasal approach.
Advantages of the external approach include the surgical exposure available, potentially allowing more accurate anatomic diagnosis. The external approach also provides the opportunity for precise tissue manipulation, suturing, and grafting. Disadvantages include the transcolumellar incision, wide field dissection resulting in potential loss of support, and nasal tip edema.
A central tenet of rhinoplasty decision-making has been the concept of a graduated approach. This concept is based on the idea that achieving the desired goals with the least amount of surgical dissection provides the best chance of success. However, the critical issue is how much exposure is needed for reliable execution of any specific technical maneuver. Adamson has astutely observed that there is no ideal approach—each surgeon will develop a unique approach based upon the concepts outlined and based on the techniques and experiences he or she has developed in the course of an eclectic training.
Perkins describes an evolution in his personal philosophy that reflects some of the issues involved in this decision-making process and provides valuable insight into the evolution in the decision making that has occurred over the past 15 to 20 years. While the concept of a graduated approach to achieve a pleasing aesthetic result has been foremost in his personal philosophy, the evolving need to achieve more refined results and prevent late complications has resulted in his increased use of the open approach, which allows the opportunity to use certain grafting techniques. Perkins continues to strongly advocate the philosophy that the approach selected should provide the least intervention in the shortest time to achieve a satisfactory result and satisfy the patient's goals. However, his choice of approach has changed due to late complications that he has seen occur. The two areas where he finds most commonly occurring late complications in rhinoplasty are the midnasal pyramid and lateral alar sidewalls. He emphasizes the paramount importance of providing a structural foundation for the middle vault (i.e., spreader grafts). While issues such as these can be addressed using the endonasal approach, Perkins indicates that it is sometimes far easier to place structural grafts via the external approach. Also, he maintains that when marked reduction of overprojection is required, it is often easier to use the external columellar approach.
Regardless of approach, one must be mindful of the need to maintain appropriate structural support. When the approach is disruptive of tip support, countermeasures, such as the placement of a columellar strut, are warranted. When the support to the upper lateral cartilages has been disrupted, spreader grafts may be appropriate.
It is important that the communication between patient and surgeon regarding the goal of surgery be a clear one. This is discussed in detail in other chapters in the book, as well as in other articles. Clear and thorough communication between patient and surgeon is extremely helpful in reducing complications in rhinoplasty. The authors recommend that the rhinoplasty surgeon give considerable and careful thought to his or her approach during the office consultation, with the goal of optimizing communication with the patient about their proposed procedure.
With this in mind, computer imaging warrants specific discussion. Computer imaging is a “video game.” It is simply a way to communicate a shared surgical goal. It does not generate an “after” picture. As the senior author explains to patients, it is not a guarantee and should not be taken to offer even the slightest implication of a guarantee. The senior author does not provide the patient with printouts of the computer imaging.
Having said this, the senior author finds computer imaging to be extremely useful. He routinely prints out the preoperative photos and shared-surgical-goal photographs and has them for intraoperative reference point. The senior author reviews his notes and these photographs preoperatively and also throughout surgery to keep the goal of surgery foremost in his mind as surgery progresses.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here