Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The rectus abdominis muscle (RAM) flap and its variations are some of the most important flaps used in reconstructive surgery. Its popularity is explained by the location of its skin island in the inferior abdomen, which results in a skin resection similar to that of conventional abdominoplasties, especially in women undergoing breast reconstruction.
The RAM flap was first described by Holmstron in 1979, who based the flap on its inferior pedicle, the deep inferior epigastric artery (DIEA). The RAM flap gained popularity with the work of Hartrampf, with its utilization as a pedicled flap based on its superior pedicle, the superior epigastric artery (DSEA), in breast reconstructions.
With the objective of reducing the sequelae resulting from harvesting it from the abdominal wall, Koshima in 1989, proposed its use with complete preservation of the rectus muscle and its innervation, a flap that is now termed the deep inferior epigastric artery perforator (DIEP) flap. Currently, the DIEP is considered the gold standard in breast reconstructions in which large flaps are required (see Ch. 16 ).
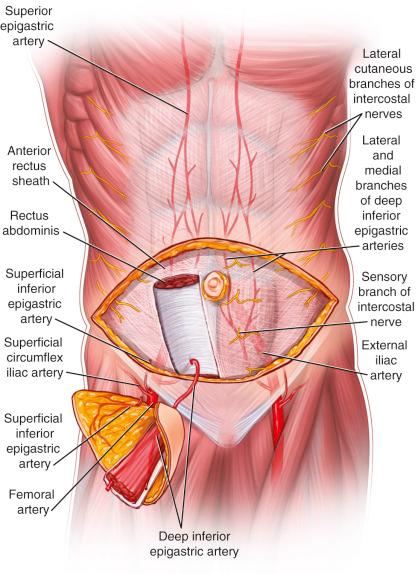
The rectus muscle exhibits double nourishment (type III Mathes/Nahai) and is supplied superiorly by the superior epigastric artery, a branch of the internal thoracic artery, and by the deep inferior epigastric artery, a branch of the external iliac artery. These two vessels comprise an intramuscular anastomotic network with each other above the level of the umbilicus. This vascular system also anastomoses with the intercostal branches. Along its course, these arteries emit perforating branches that supply the overlying skin.
deep inferior epigastric artery
Length: 7 cm (range 6–8 cm)
Diameter: 3.5 mm (range 3–5 mm)
The inferior epigastric artery is a branch of the external iliac artery. It arises superior to the inguinal ligament and passes superomedially in the layer superficial to the peritoneum but deep to the transversalis fascia. Medially it passes deep to the conjoint tendon. At the level of the arcuate line (4–6 cm above the pubic bone), it passes superiorly and superficially to perforate the posterior leaflet of the rectus sheath. Clinically the arcuate line is important as the site of entry of the inferior epigastric artery into the rectus sheath. The DIEA enters the rectus muscle in its lateral third and divides into a medial and lateral branch. These branches provide perforators to the skin at various locations. Within the rectus sheath, the inferior epigastric artery passes superiorly and ramifies to anastomose with the superior epigastric artery. It lies within the neurovascular plane of the transversalis fascia and transversus abdominis aponeurosis.
Two types of perforating vessels from the medial and lateral branches are visible:
Perforators with a straight and perpendicular intramuscular path located in the intermuscular septum in the direction of the subcutaneous tissue. In this case the intramuscular course of the vessel is short and perpendicular to the muscle fibers.
Perforators with an oblique intramuscular course. The perforating vessel crosses two or more septa on its way to the subcutaneous tissue, making dissection difficult but increasing pedicle length. In the lateral row, 79.2% of the vessels display a rectilinear course, whereas in the middle row only 18.2% of the vessels present this pattern.
deep superior epigastric artery
Length: 3 cm (range 2–4 cm)
Diameter: 1.5 mm (range 1–2.5 mm)
The superior epigastric artery is a continuation of the internal mammary artery, which branches at the sixth intercostal space into the musculophrenic artery and the superior epigastric artery. It then emerges beneath the chest wall along the posterior and medial aspect of the muscle. The superior epigastric vessels run inferiorly deep to rectus abdominis and superficial to the fibrous layer that forms the posterior leaflet of the rectus sheath. Within this layer they ramify to widely anastomose with the inferior epigastric artery.
When a cutaneous component is harvested such as in a musculocutaneous flap or a perforator flap, the deep inferior epigastric vessels provide a more robust blood supply. The superficial inferior epigastric artery also contributes to the blood supply of the anterior abdominal skin.
subcostal and intercostal arteries
Length: 2 cm
Diameter: 0.5–1 mm
Branches from the thoracic aorta, inferior vena cava, and intercostal pedicles run immediately below each corresponding rib. At the anterior portion of each costal arch, the vascular pedicles, associated with the intercostal nerves, perforate the transversalis fascia, in its lateral aspect. These pedicles anastomose with the superior epigastric artery and vein within the deep surface of the rectus muscle. Although there is a real vascular anastomosis between these vessels, they play a smaller role in the nourishment of the rectus muscle.
superficial superior epigastric artery and the superficial circumflex artery
Both arteries play a small role in the nourishment of the rectus flap and no focus will be given to those vessels in this chapter.
Veins accompany the arteries and are present in pairs.
deep inferior epigastric vein
Length: 6 cm (range 4–8 cm)
Diameter: 4 mm (range 2–5 mm)
deep superior epigastric vein
Length: 3 cm (range 2–4 cm)
Diameter: 2.5 mm (range 1.5–3 mm)
superficial inferior epigastric vein
Length: 6.4 cm (range 3.5–10 cm)
Diameter: 2.1 mm (range 1–3 mm)
This drains to the saphenous bulb and cooperates in skin drainage of the anterior abdomen.
The 7th–12th intercostal nerves enter the RAM at various points and divide into motor and sensory branches. The sensory branches join the perforators that supply the overlying skin.
Segmental motor branches of the 7th–12th intercostal nerves.
The flap can be dissected as a pure muscle flap; as a segmental muscle flap with preservation of part of the muscle; as a myocutaneous flap with a transverse, oblique, or vertical skin island flap; as a myocutaneous flap with muscle preservation; or as a perforator flap, with preservation of the muscle and its innervation.
The 7th, 8th, 9th, and/or 10th ribs can be included in a rectus abdominis flap. They are nourished by the 7th, 8th, and 9th intercostal vessels, which join the costomarginal artery along the inferior border of the costal margin. The costomarginal artery then forms an anastomosis with the superior epigastric artery along the deep surface of the rectus abdominis muscle. This flap is useful in three-dimensional reconstructions of bony and soft tissue defects of the face.
The position of this flap's skin island in the inferior abdomen, especially in women who have already been pregnant, is advantageous. Dissection of the flap can lead to a skin resection similar to a conventional abdominoplasty, resulting in not only a well -placed scar but also an improvement in body contour.
Since the flap is dissected in the supine position, reconstruction of defects in the anterior trunk as well as the upper and lower extremities can be performed without a change in position during the procedure.
The vascular anatomy is uniform and reliable. The pedicle is long and has large diameter vessels, simplifying microvascular anastomoses.
If it is transferred based on its superior pedicle, the whole length of the pedicle included in the rectus muscle will greatly increase its rotational arc.
The design of the skin island is very versatile. It can be transverse, vertical, and/or oblique.
In large three-dimensional defects, the flap can be folded on itself, providing good coverage particularly in complex head and neck resections.
A muscle flap, without a skin island, can be harvested through a low transverse abdominal incision
Weakening of the abdominal wall after flap harvest may be seen with variations of the flap that include a significant part of the anterior rectus sheath. If only a small part of the anterior fascia and the abdominal wall layers is closed appropriately, weakening of the abdominal wall and bulgings or hernia will be less likely to happen.
The removal or denervation of the RAM can create a slight functional deficit, especially upon flexing the trunk. However, utilizing the perforator form of the flap minimizes this deficit (see Ch. 57 ).
In obese patients, the myocutaneous form of the rectus flap is very likely to be bulky for resurfacing objectives.
This muscle does not function well as a functional muscle transfer since its excursion is minimal and its innervation is segmental.
Preoperative evaluation is of fundamental importance. A detailed history and physical examination can reveal important aspects of the surgical procedure. Previous abdominal or pelvic surgeries can damage the vascularization of the flap. Previous irradiation of the internal thoracic vessels can diminish its blood flow. If one suspects injury of the pedicles, additional studies should be performed.
One should be aware of prior abdominal scars, especially transverse ones, which can indicate previous injury to the pedicle. For instance, the Kocher (subcostal) incision usually divides most of the rectus muscle, so that the superiorly based RAM flap may be contraindicated, though Doppler ultrasonography may be used to check the integrity of the pedicles.
Prior undermining of the skin flap of abdominoplasties is a relative contraindication. Although reports in the literature mention that patients with prior abdominoplasties have been subjected to harvesting of myocutaneous RAM flaps without complications, we do not recommend it. If one still wants to use an abdominal skin flap, a thorough history and discussion with the previous surgeon may aid in determining the level and extent of dissection during the abdominoplasty. CT angiography can help determine availability and location of perforators. Also, careful delay procedures can be helpful.
In obese patients, fat necrosis is a major probability when the superiorly based pedicled form is utilized. Supercharging and superdraining, microsurgical inferiorly based flaps or delay procedures can be indicated in this situation.
If the proposed flap requires dissection of its perforators, prior location of the pedicles with duplex ultrasound or CT angiography is recommended. Handheld unidirectional Doppler can be used, although its sensibility and specificity are lower. Although not mandatory, knowledge of the pedicles' exact location permits a speedier and accurate dissection of the flap.
A detailed physical examination should be performed in every patient. One should look for abdominal muscle weakness or herniations that should be dealt with intraoperatively. At this time, the cutaneous island flap planning begins. If the patient has enough skin laxity to allow a transverse skin island (especially in patients who have been pregnant), the transverse rectus abdominis muscle – TRAM flap is our first choice. Otherwise, a vertical skin island must be used with the vertical rectus abdominis muscle – VRAM flap.
Patients in whom the internal mammary artery has been used for cardiac revascularization should not use a superiorly based flap. Although there is an anastomosis of the costomarginal artery with the superior epigastric artery, distal to the internal mammary artery, that may supply the rectus muscle, there are not currently sufficient data to show that this vessel can nourish the whole flap, particularly when a large skin island is included.
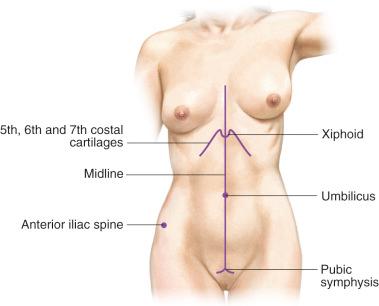
The RAMs are located in the anterior abdomen with their medial limits situated in the midline, except in multiparous women who present with diastasis of the rectus muscles, separating them from the midline. The superior limit is the rib cage, as the muscle arises from the fifth, sixth, and seventh costal cartilages and the inferior limit is its insertion at the pubis (see Fig. [4815]). Palpation of the contracted muscle easily determines its location in thin patients.
The design and size of the flap vary greatly depending on the surgical technique utilized and the characteristics of the donor and recipient areas. Therefore, each transfer will be explained individually.
Our preference is to include periumbilical perforators in the design of the skin paddle whenever possible. These perforators are larger and provide better supply to the skin of the abdominal wall. However, in some cases, in order to preserve a majority of periumbilical perforators, a supraumbilical incision should be used as the superior margin of the flap. Closure of the donor site in that situation may not allow for the inferior incision to be placed immediately above the pubic hairline. In those situations, the inferior incision is placed higher in the abdomen, in a visible location and can be improved in a future procedure through re-advancing the superior abdominal flap and repositioning the scar lower in the abdomen. The other alternative is to place the superior incision lower than the umbilicus and sacrifice some of the periumbilical perforators, allowing for a more aesthetically pleasing incision line.
The most commonly employed design of the skin portion of the flap is the transverse lower abdominal skin flap, similar to the skin resection of an abdominoplasty. The superior margin of the skin island is usually 2 cm above the umbilicus (in order to include the periumbilical perforators) and the inferior margin is above the pubic hairline. When the lower abdominal skin is harvested as a myocutaneous flap based on blood supply traversing the rectus muscle with inclusion of the muscle in the flap, this is called a transverse rectus abdominis myocutaneous (TRAM) flap. This design permits dissection of a thick flap, since it is a region that usually accumulates some excess fat, and it confers a pleasing aesthetic result to the donor area. Variations in flap design depend on the type of flap dissection utilized.
This kind of flap dissection provides a reliable blood supply to the ipsilateral skin and part of the contralateral skin. However, the remaining contralateral skin island should be resected to achieve abdominal symmetry.
If a large amount of tissue is required, the flap based on both RAMs may be employed. In this case a larger flap can be designed because there will be two vascular pedicles nourishing the flap. If necessary, the flap can be designed more proximally, although it should be borne in mind that in this case the resulting scar will also be higher up. We recommend that this bipedicled flap is not used as a routine since its morbidity to the donor site is higher than the unipedicled one.
When this type of reconstruction is employed, its vascularization is abundant and reliable, permitting the use of the entire inferior abdominal skin.
In other types of reconstructions, the flap design will depend on the defect to be repaired. Flaps with vertical or oblique skin islands can be utilized or even separate distinct skin islands, based on perforator pedicles. If the design is oblique, it is possible to utilize the skin portion above the rib cage that has the advantage of being thinner and consequently more suitable for modeling the flap. This flap is designed transversely over the anterior portion of the lower costal margin laterally all the way to the level of the midaxillary line. On the other hand, if volume is necessary, a major or minor portion of the rectus muscle can be included in the flap, always bearing in mind the fact that about 20–30% of the muscle volume is usually lost due to denervation of the muscle. If the planned flap is purely muscular, it can be dissected through a paramedian incision placed longitudinally and centered over the rectus muscle with a lateral extension in the caudal portion that aids in exposure of the DIEA, or alternatively, via a low transverse incision, followed by undermining of an abdominal flap and dissection of the muscle flap below it.
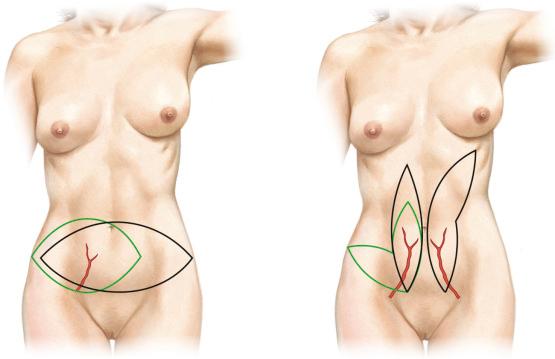
The placement of the skin island may differ slightly if a pedicled flap is to have an extended reach; otherwise, the principles are similar and the designs described can be used for both pedicled and free flaps.
For a free flap, usually, the pedicle is the DIEA. Although not impossible to perform a free flap based on the DSEA, it is very impractical, since the access to the thoracic internal vessels and the DSEA itself is not easy compared with the access to the DIEA.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here