Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
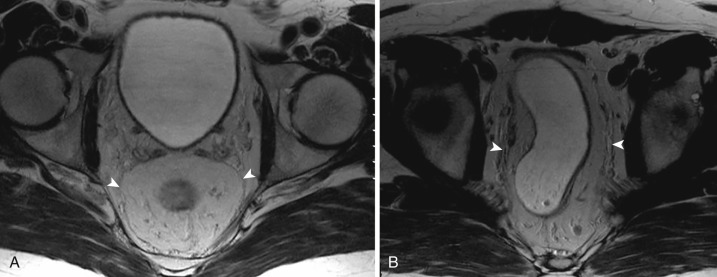
The rectum and anal canal form the terminal part of the intestine. The rectum varies in length from 10 to 15 cm and extends from the rectosigmoid junction at the level of the S3 sacral vertebra to the anorectal line. The surgical anorectal junction is at the upper edge of the anorectal muscle ring located about 4 cm from the anal verge. The anatomic anorectal junction called the dentate line marks the junction of the endodermal primitive gut with ectodermal proctodeum. It is located about 2 to 3 cm from the anal verge. The rectum is predominantly retroperitoneal, and only its proximal 1 to 2 cm has a peritoneal extension along its anterior and lateral walls. The depth of peritoneal reflection is variable between men and women. This peritoneal reflection in men (between the rectum and bladder) is called the rectovesical recess, and in women (between the rectum and uterus), the rectouterine recess. The depth of the rectovesical recess in men is deeper than the rectouterine recess in women. The rectum has three lateral curvatures or flexures with corresponding indentations on the opposite-side wall produced by crescent-like projections of mucosa, submucosa, and circular musculature of the rectal wall called rectal valves. The superior and inferior rectal valves are on the left side and located about 4 cm below the rectosigmoid junction and 2 to 3 cm above the dentate line, respectively. The middle rectal valve is on the right side about 6 to 7 cm above the dentate line. The rectal wall is composed of mucosa, submucosa, and muscularis propria comprising inner circular and outer longitudinal muscle layers. The rectum is surrounded by variable amounts of mesorectal fat limited peripherally by mesorectal fascia (MRF), which is a condensation of the visceral layer of the endopelvic fascia. The mesorectal fat has perirectal lymphatics, vessels, and lymph nodes. Posteriorly the MRF fuses with the presacral fascia, which separates it from the presacral space; anteriorly it fuses with the Denonvilliers fascia, separating it from the prostate and seminal vesicles in males and the vagina in females. The MRF forms an important local barrier for the spread of rectal carcinoma and an important plane for surgical resection. High-resolution T2-weighted MRI demonstrates the MRF as a thin hypointense layer surrounding the high-signal-intensity mesorectal fat ( Fig. 51-1 ).
The anal canal has an inner internal sphincter and an outer external sphincter. The internal sphincter is composed of obliquely oriented smooth muscle fibers that are contiguous with the inner circular muscle layer of the rectum. The external sphincter is composed of striated muscle fibers arranged in subcutaneous, superficial, and deep portions. The deep portion of the external sphincter blends with the puborectalis portion of the levator ani muscle.
The rectum and upper anal canal are supplied by the inferior mesenteric artery through the superior rectal artery. The internal iliac artery, through its middle and inferior rectal arteries, supplies the lower anal canal. Lymphatic and venous drainage of the rectum and anal canal follows the corresponding arteries. The immediate lymphatic drainage is to regional perirectal lymph nodes and later follows the major lymph nodes along the superior rectal and inferior mesenteric vessels. There is also lateral lymphatic drainage along the middle rectal vessels to the internal iliac lymph nodes.
Colorectal cancer is the third most common cancer in the United States, and approximately 39,610 cases of rectal cancer were expected to be diagnosed in the year 2015. Adenocarcinoma is the predominant rectal malignancy. Other rare types include neuroendocrine, squamous cell, adenosquamous, spindle cell, and undifferentiated carcinomas. The epidemiology, etiology, and pathogenesis of rectal carcinoma are similar to colon cancer. Diagnosis is established by digital rectal examination followed by proctoscopy and tissue diagnosis. Advances in surgical technique and adjuvant preoperative chemoradiation treatment of rectal carcinoma have led to significant improvement in disease-free survival. Accurate staging is vital for treatment planning. Imaging is mainly used for staging and treatment planning. Table 51-1 outlines the American Joint Committee on Cancer's (AJCC's) tumor-node-metastasis (TNM) staging of rectal carcinoma.
| Primary Tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of tumor |
| Tis | Carcinoma in situ: intraepithelial or invasion of lamina propria |
| T1 | Tumor invades submucosa |
| T2 | Tumor invades muscularis propria |
| T3 | Tumor invades through the muscularis propria into the perirectal fat |
| T4a | Tumor penetrates to the surface of visceral peritoneum |
| T4b | Tumor directly invades or is adherent to other organs or structures |
| Regional Lymph Nodes (N) | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in 1-3 regional lymph nodes |
| N1a | Metastasis in 1 regional lymph node |
| N1b | Metastasis in 2-3 regional lymph nodes |
| N1c | Tumor deposit(s) in the subserosa, mesentery, or nonperitonealized pericolic or perirectal tissues without regional nodal metastasis |
| N2 | Metastasis in 4 or more regional lymph nodes |
| N2a | Metastasis in 4-6 regional lymph nodes |
| N2b | Metastasis in 7 or more regional lymph nodes |
| Distant Metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| M1a | Metastasis confined to one organ or site (e.g., liver, lung, ovary, nonregional node) |
| M1b | Metastases in more than one organ/site or the peritoneum |
EUS has the ability to demonstrate different layers of the rectal wall and is accurate in assessing the depth of tumor invasion into the rectal wall. EUS has a sensitivity, specificity, and accuracy of 96% to 97% in detection of muscularis propria invasion in early-stage rectal carcinoma. Sensitivity, specificity, and accuracy of EUS in detection of positive regional perirectal lymph nodes in early-stage rectal carcinoma are 53%, 77%, and 72%, respectively. EUS has several limitations, including inability to image high rectal and stenosing carcinoma, a limited field of view (FOV) that makes it difficult to assess the extent of perirectal invasion, inability to identify the MRF, and limited evaluation of the lateral pelvic wall and surrounding visceral invasion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here