Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
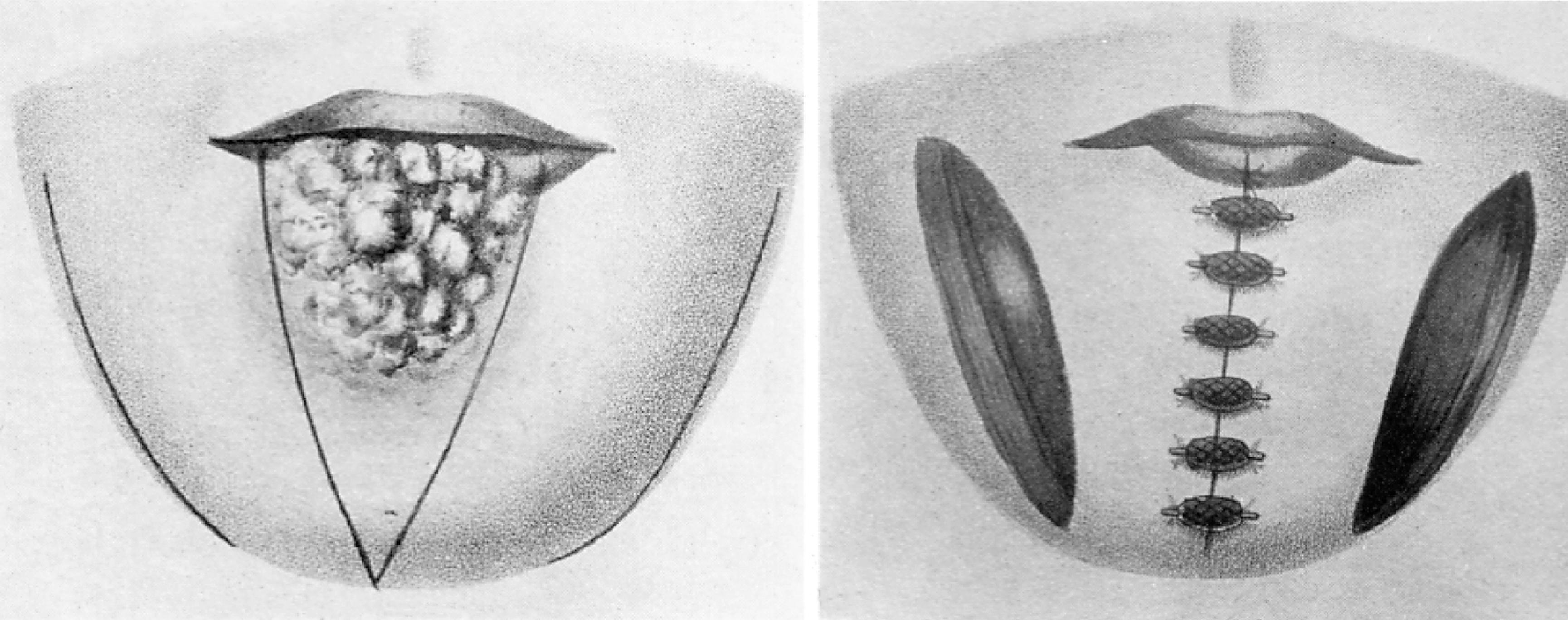
The upper and lower lips comprise a distinct anatomic unit that is the principal feature of the lower face. The lips play a major role in facial appearance and function. Reconstruction of the lip can present a challenge to the reconstructive surgeon who seeks excellence in restoration of the aesthetics and functioning of this unique structure. Descriptions of lip reconstruction date back to at least 1000 BC in the eastern Sanskrit writings of Susruta. , Early reports of lip reconstruction in the western literature date back to at least the first century ( Fig. 19.1 ). A description of the classic V-shaped excision of the lip and primary repair has been credited to a writing by Louis in 1768, although this method of treating lip neoplasms was certainly performed for many centuries before that. A large variety of methods for reconstructing the lips were developed and reported in the medical literature of the 19th century, from which most of the procedures performed today have some derivation.
Lip tissue is a composite of skin, muscle, and mucosa ( Fig. 19.2 ). The most distinguishing feature of the lip is the vermilion, which is modified mucosa that covers the free margin of the lips and is adapted for external exposure. There are relatively few glands beneath the vermilion, in contrast to the multitude of minor salivary glands found immediately deep to labial and buccal mucosa. The well-defined line where the anterior limit of the vermilion adjoins the adjacent lip skin is referred to as the mucocutaneous or anterior vermilion line . It represents a very important landmark in lip reconstruction. The posterior vermilion line is defined as the innermost line of contact between the upper and lower lips when the mouth is closed. Labial vermilion is usually red in color on those who have light skin and dark in color on those who have dark skin. Fullness of the rounded vermilion, particularly in females, is considered a mark of beauty in many cultures.

The body of the lips is made up principally of the orbicularis oris muscle. Orbicularis muscle fibers of the upper and lower lip interconnect or decussate as they meet together at the oral commissures. This arrangement allows the muscle to function as a sphincter that regulates the opening and closing of the lips. The muscles of facial expression that influence the lips are distributed in a radiant fashion about the orbicularis muscle in bilaterally paired sets. The facial expressive muscles are attached at specific locations along the outer margin of the orbicularis muscle. Selective contractions of the muscles serve to create the varied shapes that can be demonstrated by the lips. Because there is no internal skeleton, lip tissue is very elastic and can be stretched to a remarkable degree, offering a trait that can be very useful in reconstructive surgery.
Upper and lower labial arteries are the principle vascular supply to the lips. Both arteries are derived from the facial artery on either side of the face. The labial arteries course horizontally across the lip in the submucosal plane, immediately posterior to the orbicularis muscle at approximately the same level as the anterior vermilion line. Although the labial artery of the lower lip tends to remain in the same horizontal plane as it crosses the lip, the upper lip labial artery may rise slightly as it passes medially toward the center of the lip. Some labial arteries may have a tortuous course through the muscle. The course of the labial artery can be detected with gentle palpation and is typically easy to map out with use of a Doppler. In studies of arterial anatomy of the lower face, a variable pattern of vessels anastomosing across the lower lip and chin was found with one or more vertically oriented labiomental branches descending to the chin region. A horizontally oriented mental branch was noted in many cases. , Multiple anastomoses between the vertical and horizontal branches were observed when both were present. In the central region of the upper lip the superior labial artery gave rise to multiple septal and alar branches. The exact pattern for venous drainage is less well defined and has commonly been considered to be largely by venae comitante. Superior and inferior labial veins have been described. Both veins typically drain into the ipsilateral facial vein and are less distinct than the arteries and difficult to identify. In a cadaver study, Park and his associates identified a deep venous system of the upper lip that was considered to be independent of the arterial system. An understanding of the vascular supply of the lips is important in the planning of many reconstructive lip flaps.
The limit of the superior border of the upper lip centrally is the nasal base. The limit of the inferior border of the lower lip centrally is the mental crease, which separates the lip from the chin. The lateral borders of the upper and lower lips are marked by the melolabial and labiomandibular creases, which separate the lips from the cheeks. Although these peripheral defining lines may not be so obvious in young children, they are more pronounced with age and are recognized natural lines of the face. The melolabial and mental creases mark the sites where muscles of facial expression attach to the orbicularis muscle, providing the muscle with an indirect connection to the facial skeleton. These crease lines are strongly favored sites for making incisions required for excision of lip tumors and for the outline of many reconstructive flaps.
The relaxed skin tension lines (RSTLs) for the lips course in a radiant fashion about the oral stoma in a manner analogous to the spokes of a wheel and reflect the wrinkle lines of older patients ( Fig. 19.3 ). These lines are vertical in the central region of the lips and are progressively more oblique or slanted in lateral regions of the lips. The orientation of the lines is perpendicular to the underlying orbicularis muscle fibers. The philtrum is an embryologically derived structure with two parallel raised ridges that have no functional significance but do have aesthetic importance to the central region of the upper lip. Incisions of either lip create less unsightly scars when made parallel to the long axis of the philtrum or to the labial RSTLs.

The lips exhibit multiple motor functions, which include various facial expressions, oral retention of food and liquids, articulation of speech, and the acts of whistling and kissing. The lips also have important sensory functions of touch, pain, and temperature, which enable the monitoring of materials that enter the mouth and provide some pleasures. The most ideal lip reconstructions are those that best preserve or restore these different functions. Restoration of the orbicularis muscle sphincter is highly desirable, particularly of the lower lip. As a general rule it is best if reconstruction of the lip is accomplished from within the lip complex, except when that would result in excessive microstomia. In most cases, reconstruction of slightly more than half of either lip can be accomplished using tissue from within the respective aesthetic region of the lips. When additional tissue is required, most reconstructions involve the use of local flaps harvested from the adjacent regions of the cheek or chin. With current designs, any flap harvested from outside the lip complex to repair full-thickness lip defects fails to restore a complete functional orbicularis muscle sphincter. To a limited degree, tightness in a reconstructed lip may help compensate for deficiency of the muscle sphincter.
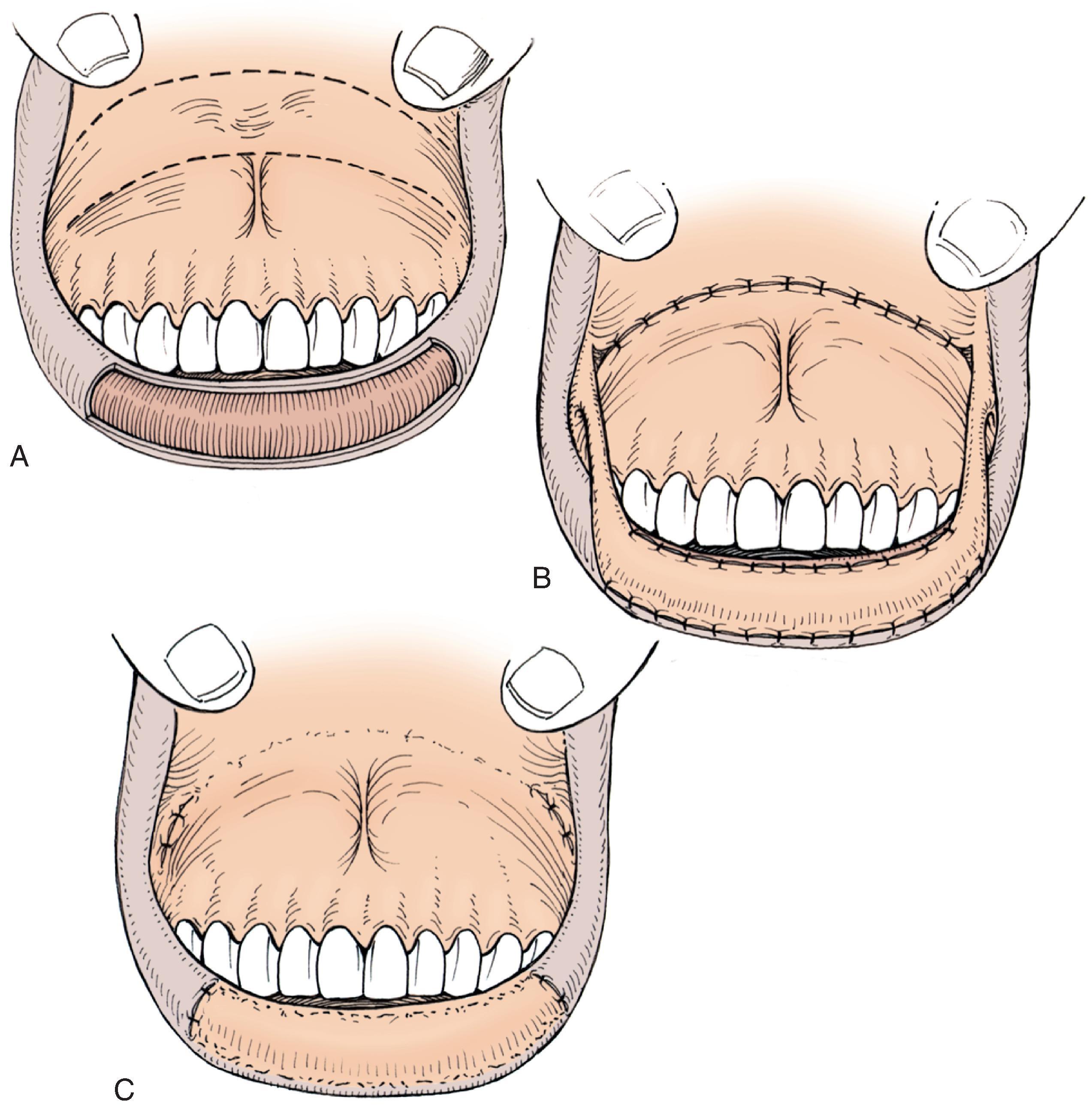
The most favored method of restoration of the vermilion is anterior advancement of the mucosa that lines the inner surface of the lip ( Fig. 19.4 ). A mucosal flap is created by undermining beneath the labial mucosa in a plane that is deep to the minor salivary glands and superficial to the posterior surface of the orbicularis oris. If necessary, dissection may extend the entire vertical height of the lip to the apex of the gingivolabial sulcus. The flap is advanced forward over the free margin of the lip to the desired point, which is usually the anterior vermilion line. Because the vermilion is actually a modified mucosal surface, reconstruction with labial mucosa offers a very close substitute. In most cases, a slight prominence of the soft tissue at the mucocutaneous junction is considered to be a favorable feature of lip contour. It is difficult to restore this fullness, however, in areas reconstructed by mucosal advancement flaps. This may in part be related to contraction of the mucosal flap as the wound heals. There is less flap retraction when dissection of the flap requires limited undermining of the mucosa of the lip.
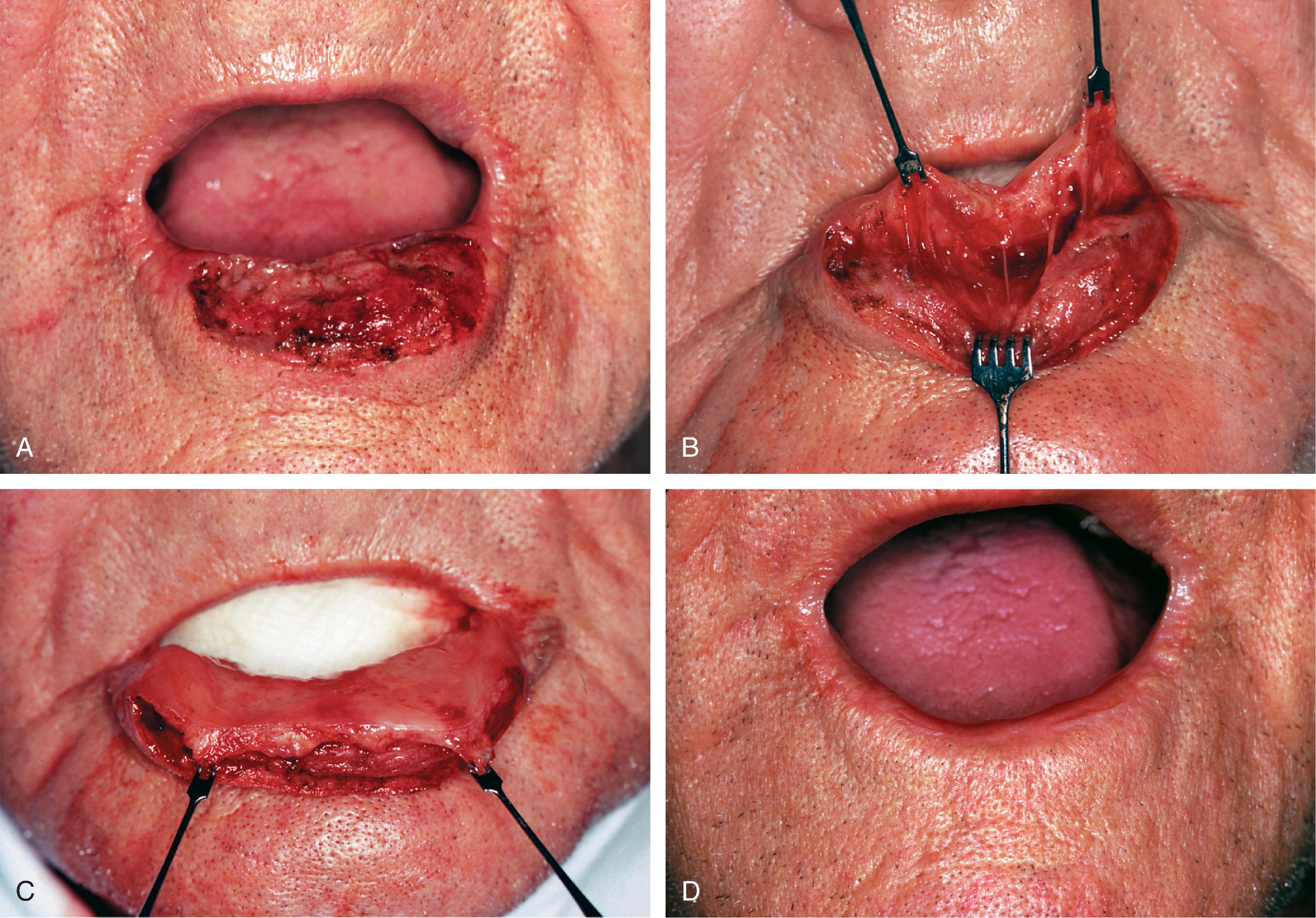
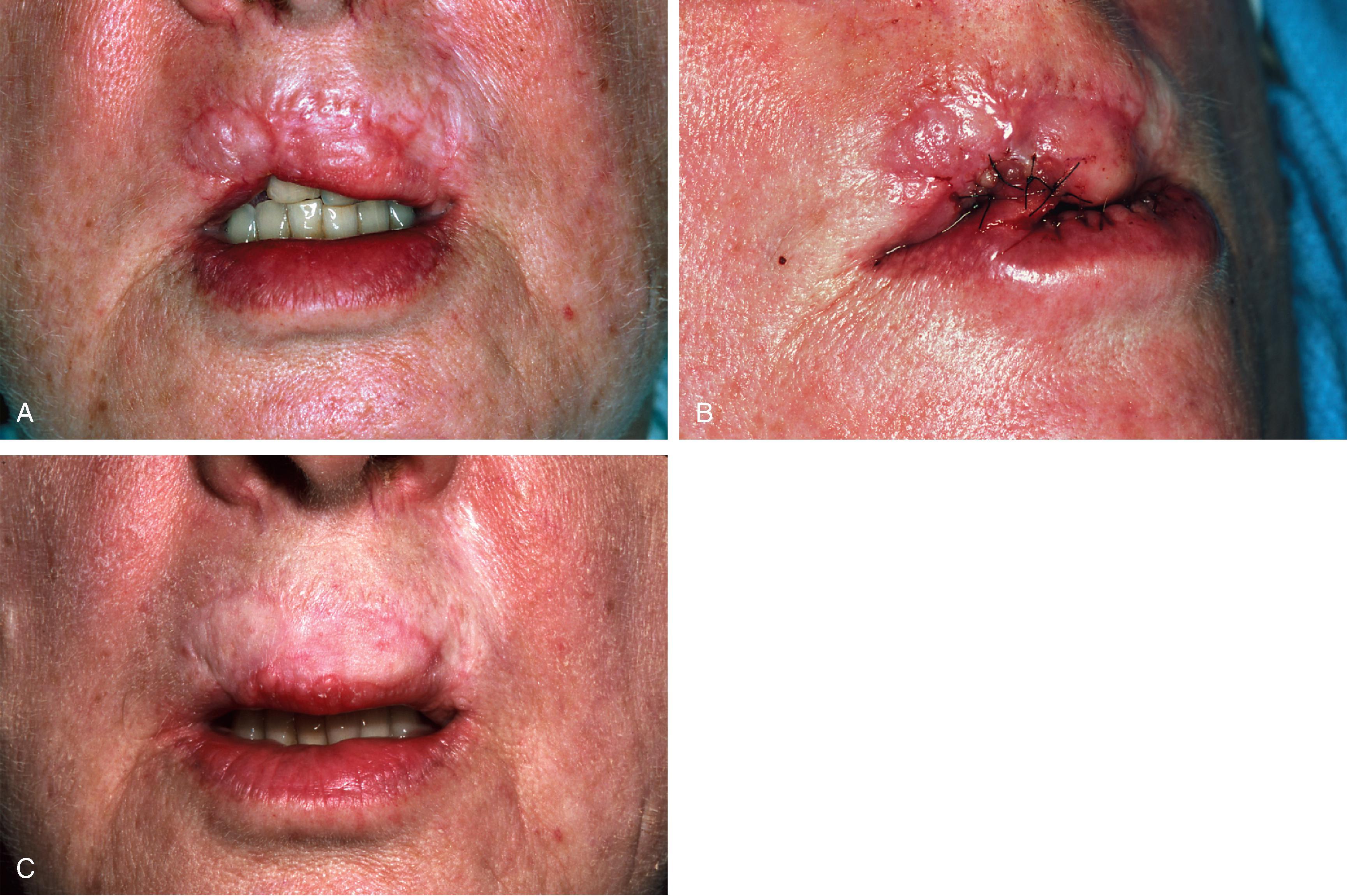
Reconstruction of the vermilion with a mucosal advancement flap may produce a pleasing aesthetic restoration of either lip. Nevertheless, several difficulties may be encountered with this technique. An early difficulty is restoring accurate positioning of the anterior vermilion line when there is an adjacent skin defect at the lip margin. In such instances, wound contraction inherent to wound maturation may influence the position of the vermilion line. If distortion or displacement of the anterior vermilion line occurs, repositioning of the reconstructed line may be possible with revision surgery. Another difficulty encountered when using mucosal advancement flaps is that the flaps tend to display a slightly deeper red color than that of the natural vermilion, especially in those with more “weathered” lips. In some cases, the darker red color can impart a slightly feminine appearance to the reconstructed vermilion, particularly when the flap covers a large surface area ( Fig. 19.5 ).

Because greater scar contraction occurs when mucosal advancement flaps cover a large surface area, eventual wound contraction may cause the body of the lip to assume a more rounded appearance. As the vermilion line is pulled posteriorly by wound contraction, adjacent whisker hairs may begin to turn up slightly and become a source of irritation to the opposing lip when the mouth is closed. This may require repositioning of the anterior vermilion line of the reconstructed lip.
Although a majority of patients regain some degree of touch, pain, and temperature sensation to the reconstructed vermilion within a matter of several months after the employment of mucosal advancement flaps, there are individuals in whom sensory return is inadequate. Influenced by Karapandzic’s concept of lip flap design, this author performs dissections with a selective spreading technique in an attempt to preserve the small neural and vascular structures that are encountered as the mucosal advancement flap is dissected (see Fig. 19.4, B ). , , These neurovascular structures are then gently stretched forward with advancement of the mucosal flap.
In some cases, small volume deficiencies of the vermilion may be restored with V-to-Y advancement flaps of labial or buccal mucosa ( Fig. 19.6 ). The advancement flap is created by a V-shaped incision with the apex of the incision positioned toward the gingivolabial sulcus. Mucosal V-to-Y advancement flaps may also be created as island flaps used to repair small adjacent vermilion defects. Incisions are made to the level of the orbicularis oris, creating an island flap that is pedicled on the underlying deep tissue. The triangular-shaped island is advanced into the adjacent recipient site, maintaining sufficient deep tissue attachments to ensure its viability. The donor site is closed primarily by direct approximation of the adjacent wound margins resulting in a Y-configuration to the wound closure. Closure of the donor site assists with securing the position of the advancement flap. Most V-to-Y island advancement flaps of the lip are designed to advance in a vertical or near-vertical orientation. There are some cases in which horizontal tissue movement is employed, using either a single island flap or bilateral opposing island flaps. Mucosal V-to-Y island advancement flaps are best suited for repair of small defects of the vermilion.
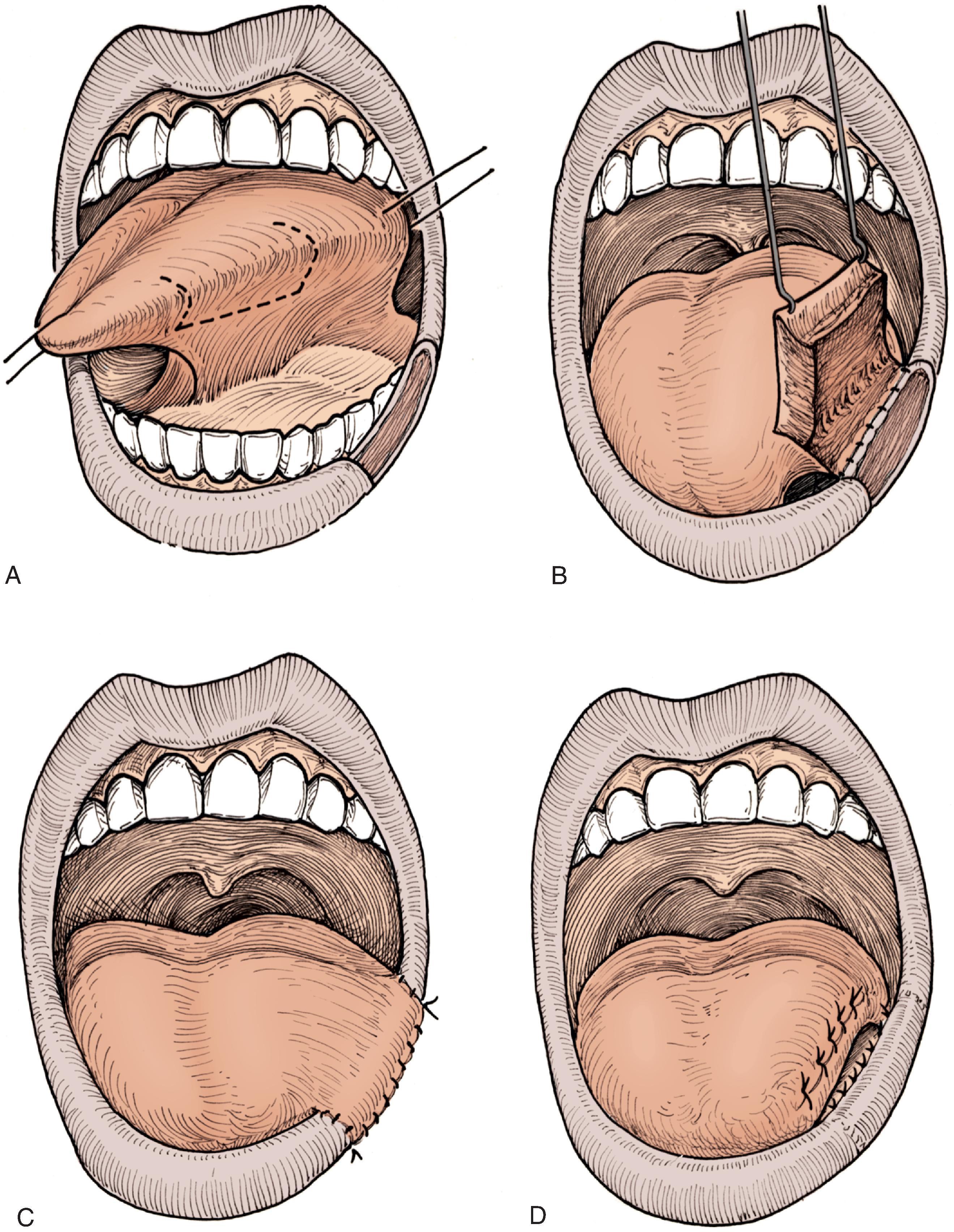
A vermilion defect may in some cases be restored with an interpolated cross-lip transfer of labial mucosa or vermilion along with some underlying soft tissue ( Fig. 19.7 ). Cross-lip transfer may be accomplished using a single pedicle flap for small defects or a bipedicle flap (“bucket handle”) for wider defects that extend horizontally across the lip ( Fig. 19.8 ). A cross-lip mucosal flap is typically designed as a linear band of mucosa, harvested from the region immediately posterior to the posterior vermilion line of the donor lip. The width of the band is determined by the width of the vermilion defect and by what will allow for donor site wound closure. The mucosal flap is most often elevated in the plane immediately superficial to the orbicularis muscle, although some muscle may be included in the flap when it is necessary to fill a soft tissue defect of the recipient lip. The labial artery may be incorporated into larger flaps providing an axial circulation and ensuring a greater likelihood of flap viability. Once dissected, the flap is transferred across the oral aperture to the vermilion defect and sutured in place ( Fig. 19.9 ). The donor site is closed primarily. Division of the pedicle and flap inset is performed 3 weeks later as a second-stage procedure.
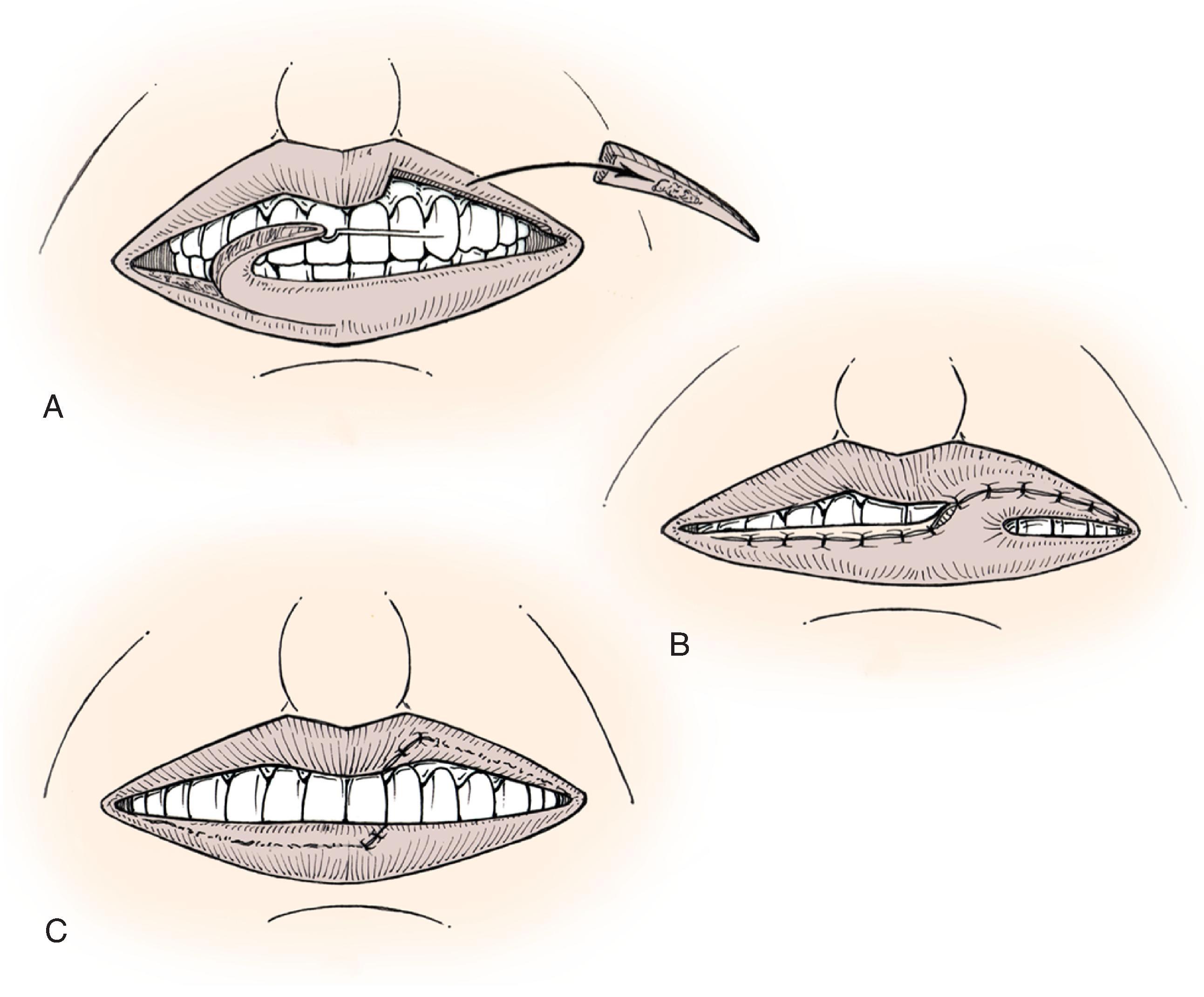
An alternative design of a cross-lip mucosal flap that does not require an axial pattern vascular supply is a broad flap pedicled on the free margin of the donor lip that can be separated after 16 days. Use of this flap causes greater restriction of mouth opening when the pedicle is in place.
Portions of the mucosal surface of the anterior tongue may be transferred to the lip to repair a vermilion defect. A mucosal flap in the form of an interpolated tongue flap is constructed for this purpose ( Fig. 19.10 ). , Mucosa transferred to the lip from the dorsal surface of the tongue will maintain the many fine filiform papillae that are characteristic of the glossal surface. Use of a tongue flap to restore the vermilion will likely create a red-colored vermilion that can be surprisingly satisfactory. A glossal flap is usually harvested from the ventral surface of the tongue for lower lip repair and from the dorsal surface of the tongue for repair of the upper lip. It is also possible to design a flap from the lateral margin of the tongue. In nearly all cases the pedicle is created at or near the free margin of the tongue. The leading edge of the flap is sutured to the anterior border of the vermilion defect in the best possible manner, anticipating that there will be considerable pulling with tongue movements. Attachment of the flap to the posterior border of the defect is accomplished during a second stage after division of the pedicle and flap inset. The second stage is usually performed 3 weeks after the initial flap transfer. The tongue donor site wound may be closed partially or allowed to granulate and the pedicle of the flap remains attached to the recipient lip. Tongue flaps are awkward and difficult for the patient. For this reason, tongue flaps are not considered as a first choice for vermilion reconstruction.
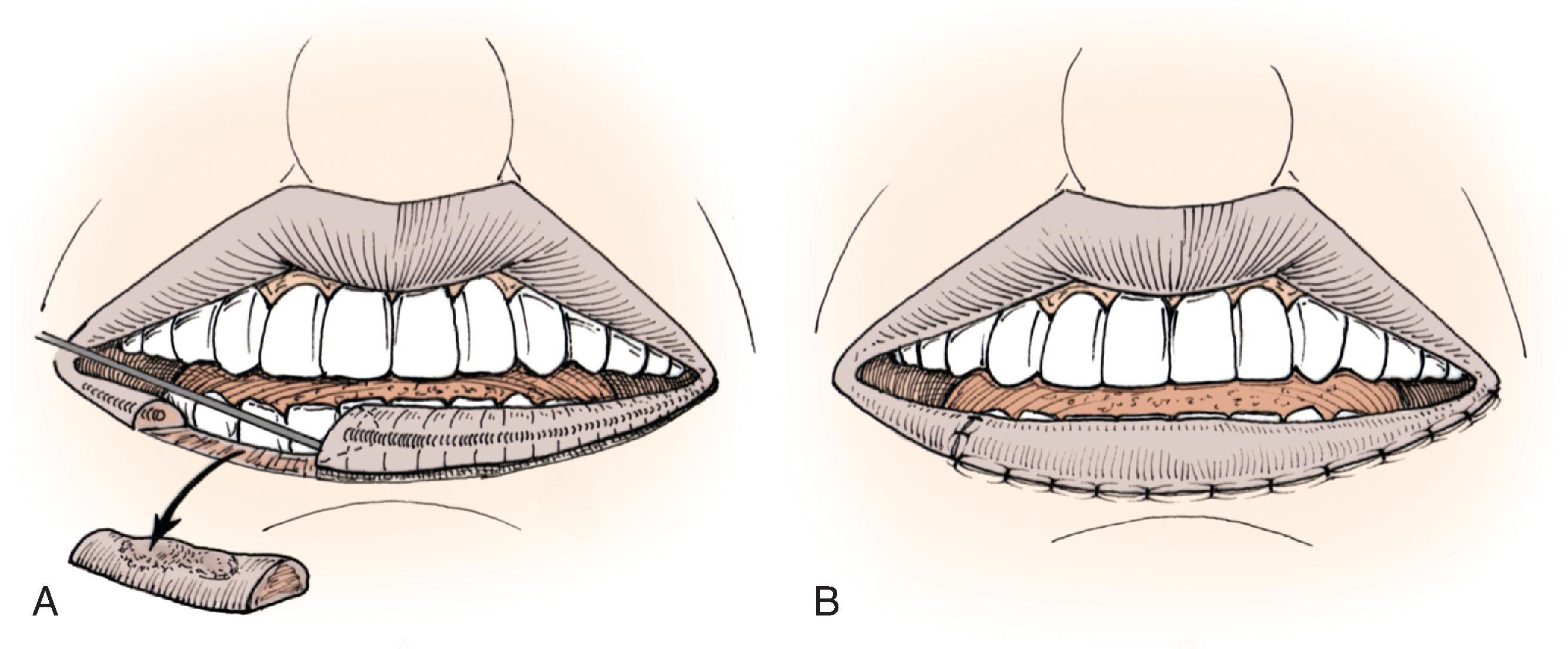
A full-thickness loss of vermilion and immediate underlying muscle may be a difficult defect to reconstruct. If the defect involves less than one-third of the width of the lip vermilion, it is possible to repair the defect by creating an advancement flap of the remaining vermilion ( Fig. 19.11 ). , A full-thickness incision is made along the anterior vermilion line inferior to the labial artery. The flap includes the vermilion portion of the orbicularis muscle. Flap dissection may require a lengthy incision to allow for adequate stretch. A meticulous wound closure is necessary to minimize visible scars in this aesthetically sensitive region.
The principles of cutaneous lip flap designs are similar to those applicable to other cutaneous surfaces. When reconstructing the lip, it is preferable to confine tissue movement within the aesthetic region of the lips unless this causes excessive distortion of adjacent structures such as the melolabial crease. Limitations are imposed on transfer of tissue within the lip complex because of the oral aperture and nasal base. In some cases of reconstruction of the cutaneous lip, it is necessary to include skin from the adjacent cheek or chin. Designing local flaps compatible with RSTLs and borders of facial aesthetic regions can provide maximum aesthetic results ( Fig 19.12 ).
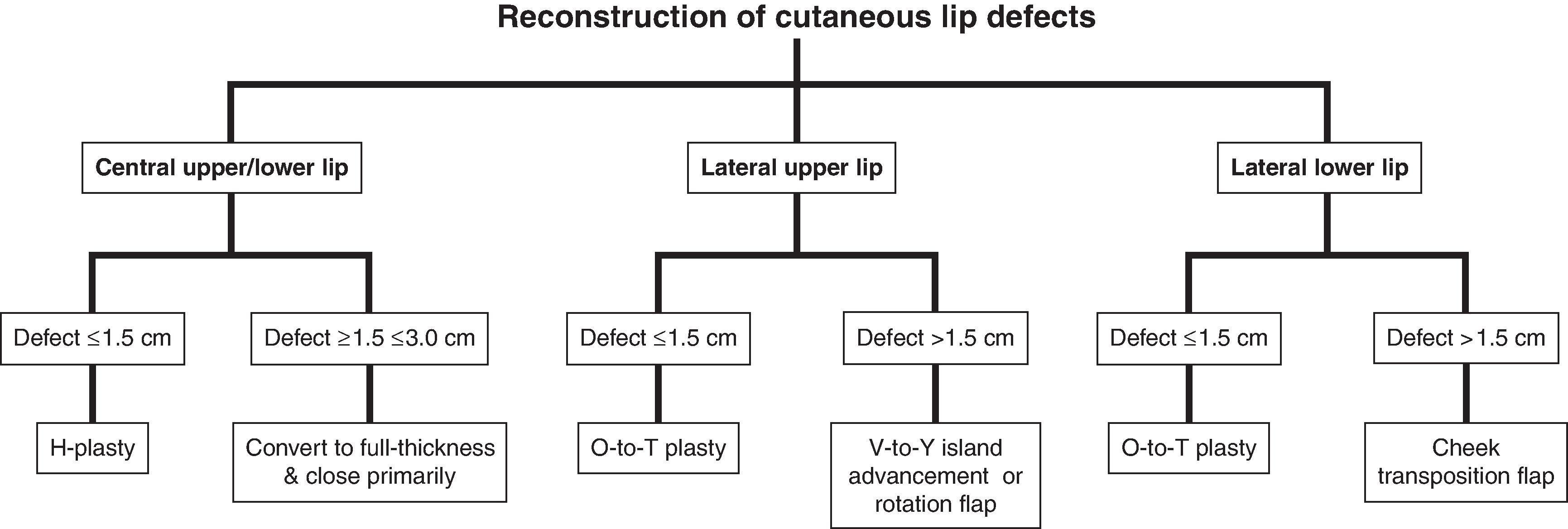
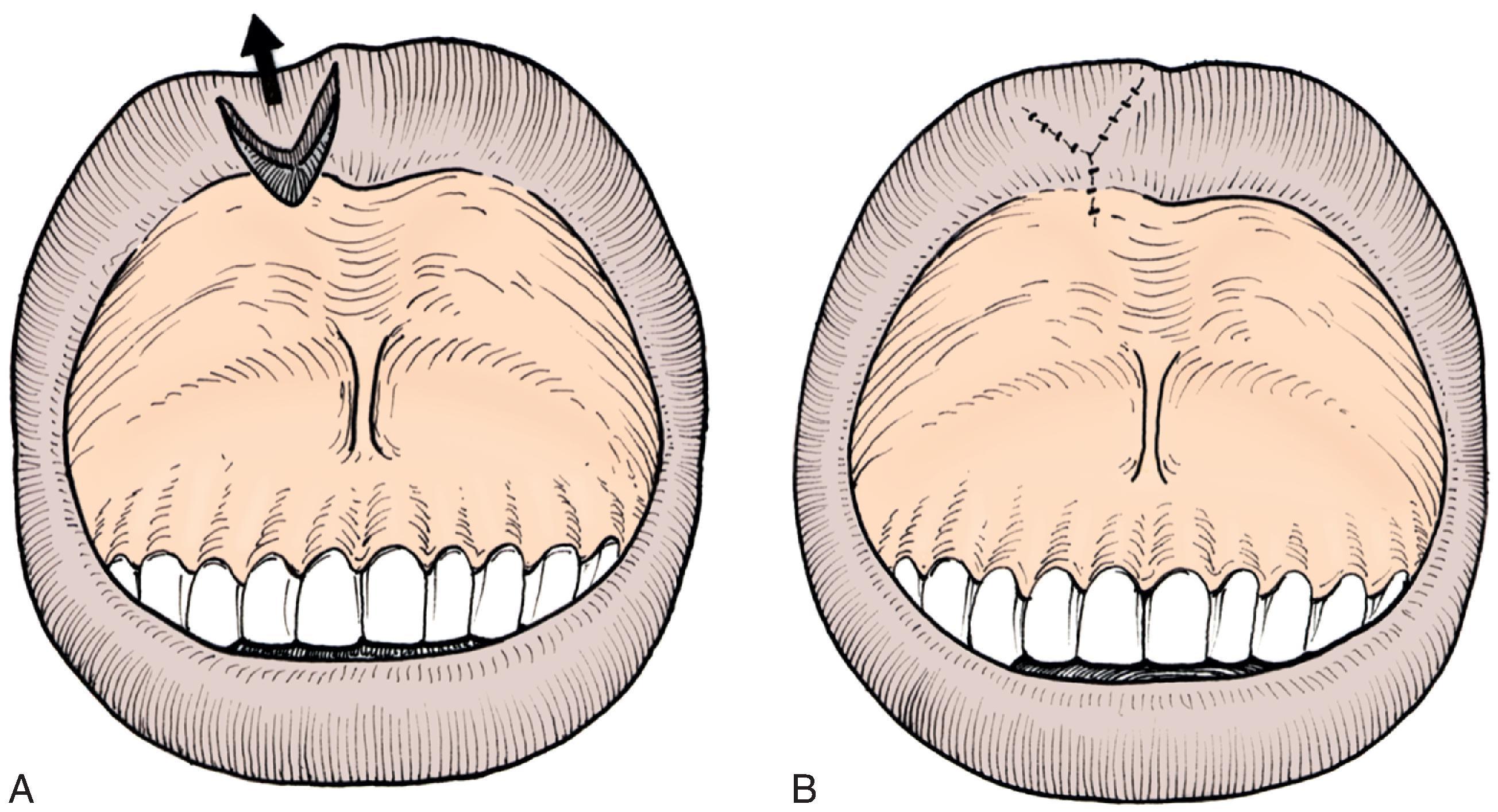
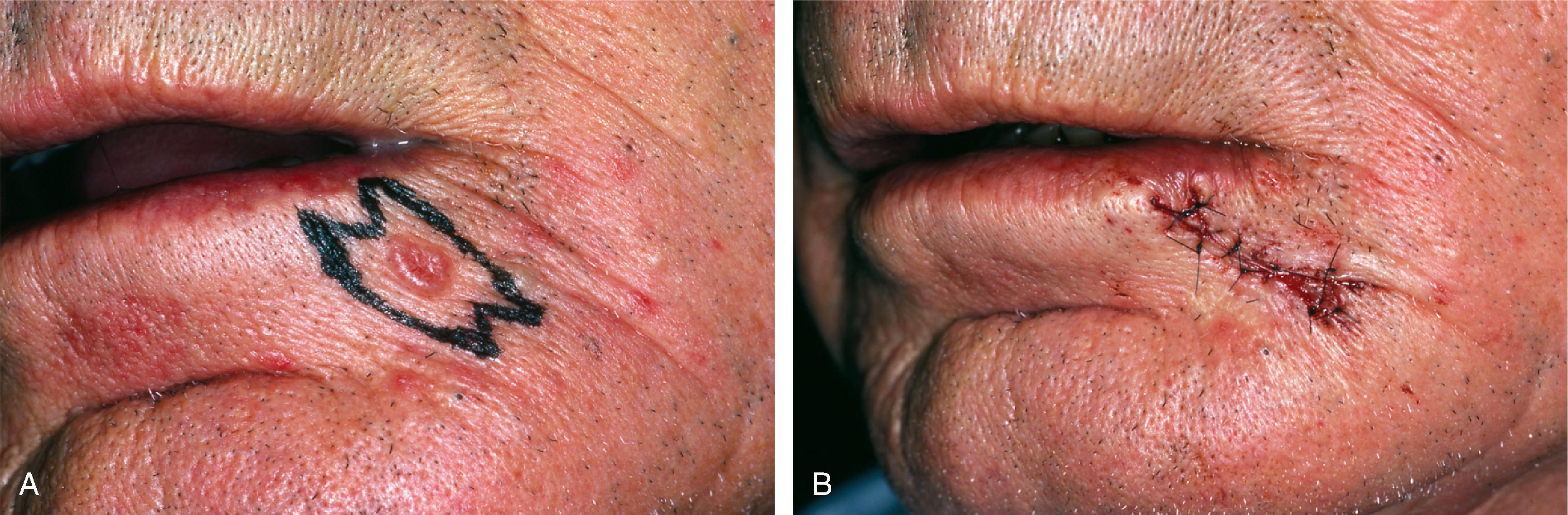
Fusiform excision and primary wound repair is the preferred method for dealing with most cutaneous tumors of the lip. When possible, the fusiform excision is oriented with its long axis parallel to RSTLs of that region of the lip. From an aesthetic viewpoint, it is preferable that fusiform excisions be confined within the boundaries of the lip, avoiding extension beyond the melolabial or mental crease lines. An M-plasty at the end of the excision line may be useful in avoiding the need to extend an incision beyond the aesthetic borders of the lips or into the vermilion ( Fig. 19.13 ). This will require closure of two small and slightly diverging incision lines near the involved end. M-plasty may also reduce tissue redundancies, particularly near the free margin of the lip.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here