Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Reconstruction of the auricle presents a significant reconstructive challenge, the ultimate goal of which is to achieve as normal an appearance and position of the auricle as possible. The orientation, size, and shape of the reconstructed ear should closely approximate the opposite ear. The postauricular sulcus should be preserved, and the relationship of the postauricular skin to the scalp should be maintained. There is an unusually high ratio of cartilage to skin surface area. This fact, coupled with the intricate three-dimensional features of the auricle and its subtle topographic details, adds to the complexity of any reconstructive effort.
Many defects involve both the skin and underlying cartilage. Auricular reconstruction requires thin, well vascularized skin flaps. Poorly vascularized, noncompliant skin, such as that found in the scar tissue that forms during healing by secondary intention, is suboptimal for reconstruction because it decreases the likelihood of achieving an adequate final three-dimensional structure. After oncologic surgery, surgical plans are influenced by the location and size of the ablative defect, the vascularity of the portion of the auricle adjacent to the defect, and the extent to which the field has been exposed to radiation therapy.
In planning auricular reconstruction, anatomic landmarks including the vermilion border, eyebrow, and nasal alar margin are considered. These structures offer only modest resistance to distortion from wound-closure tension created by surgical procedures in adjacent soft tissue sites such as the periauricular area. Auricular cartilage is very supple and may not adequately resist distortion secondary to scar contracture. Moreover, healing forces tend to distort the ear if meticulous attention is not directed toward a method of wound repair that minimizes wound closure tension.
The presence of adjacent hair-bearing scalp must be considered. When possible, it is preferable to avoid placing hair-bearing skin over the auricle. Ordinarily, the hairline above the site of the planned reconstruction is high enough not to interfere with accurate positioning of the ear. Nevertheless, occasionally proper positioning of the reconstructed segment of the ear requires the use of hair-bearing skin. In these cases, the hair can be permanently eliminated later using depilation techniques.
When auricular reconstruction is poorly planned or executed, the endeavor will be frustrating and disappointing. In such instances a cascade of poor results may include multiple revision surgeries, increased scar tissue, and decreased skin vascularity at each stage. With adherence to well-established reconstructive surgery principles, however, the results of auricular reconstruction can be extremely rewarding.
The ear is morphologically unique. The skin of the lateral surface is densely adherent to the perichondrium and is devoid of subcutaneous tissue. The fascial layer between the skin and perichondrium contains a subdermal plexus of vessels. The medial surface of the ear has loosely attached skin containing subcutaneous fat. As a result, skin is relatively more abundant on the medial surface compared with the lateral surface of the ear and has greater mobility. Medial auricular skin provides an excellent donor site for grafts and flaps. The skeletal component of the ear consists of elastic cartilage. The unique property of this cartilage, in that it is flexible and yet maintains a complex topographic contour, distinguishes it from the more rigid cartilage of the nasal septum or rib. Consequently, reconstruction of the ear using rib or septal cartilage results in loss of flexibility of the reconstructed auricle.
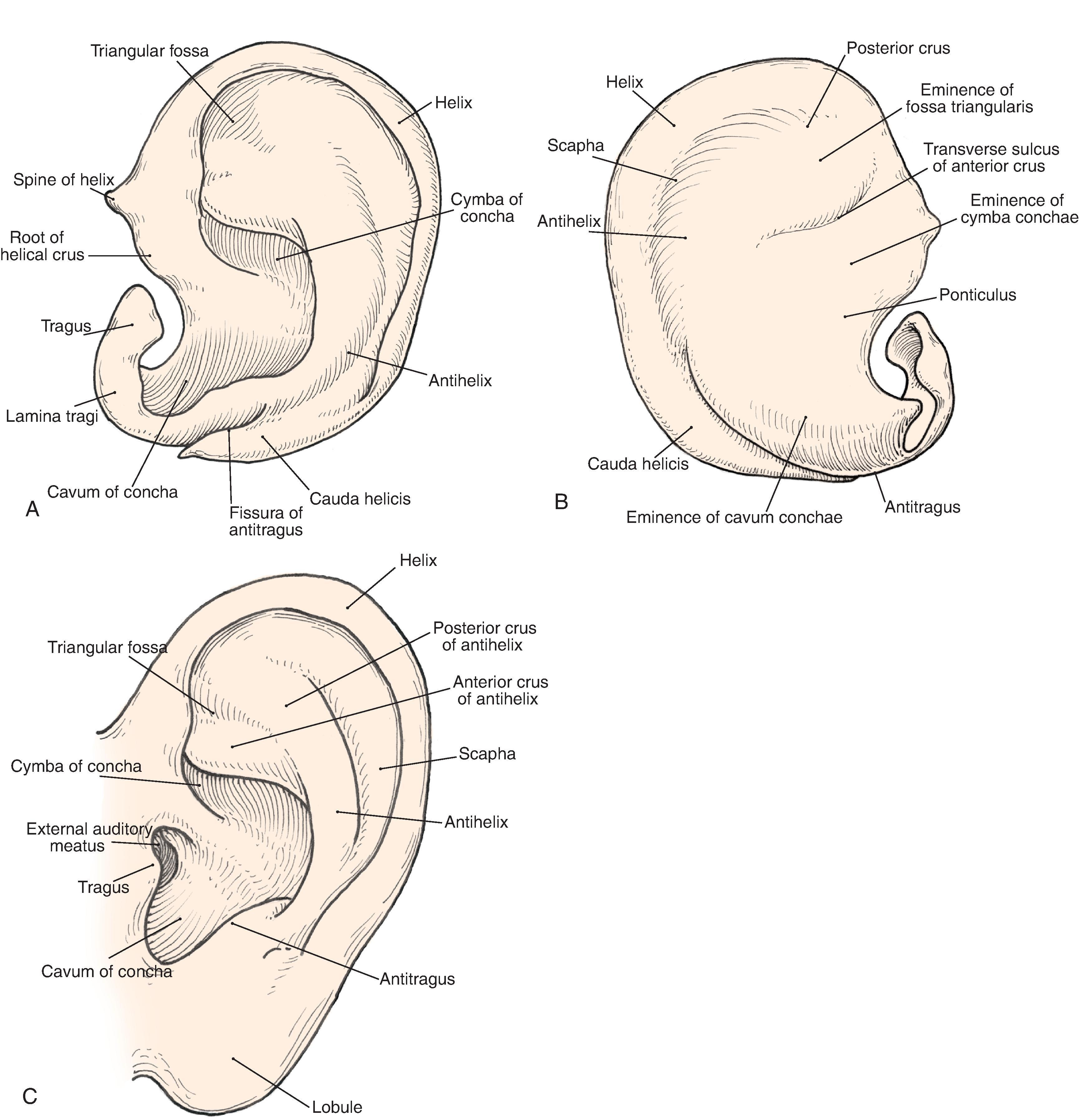
Topographic landmarks of the auricle are illustrated in Fig. 22.1 . The cartilaginous framework is composed of several distinct three-dimensional components. Laterally, these components are the conchal, antihelical, antitragal, helical, and lobular complexes. These units are critical in planning the reconstruction of defects involving cartilage replacement.
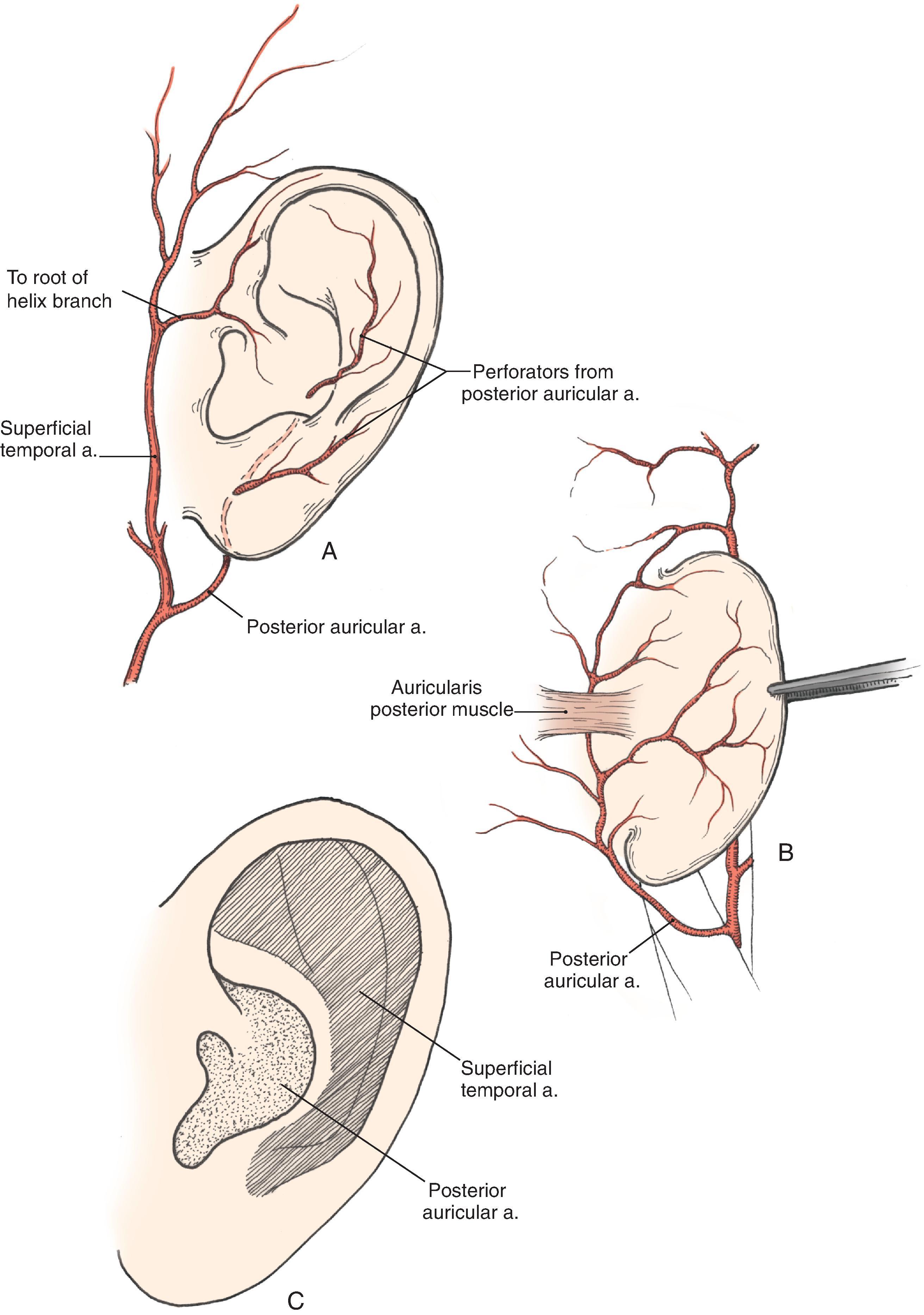
The arterial supply to the auricle is derived from branches of the superficial temporal artery and the postauricular arteries. Both vessels arise from the external carotid artery. The medial surface of the ear is supplied by the postauricular artery. The lateral surface is supplied by both the postauricular and superficial temporal arteries, creating two arterial networks. The triangular fossa and scapha network are supplied by the helical branch of the superficial temporal artery. The conchal network is supplied by the postauricular artery, which provides septal perforators to the conchal floor ( Fig. 22.2 ). Flap planning and design should give due consideration to these arterial networks. Venous drainage is via the postauricular vein, which drains into the external jugular system. There is supplemental venous drainage from the superficial temporal and retromandibular veins. Lymphatic drainage of the auricle is primarily to the preauricular, infra-auricular, and mastoid lymph nodes.
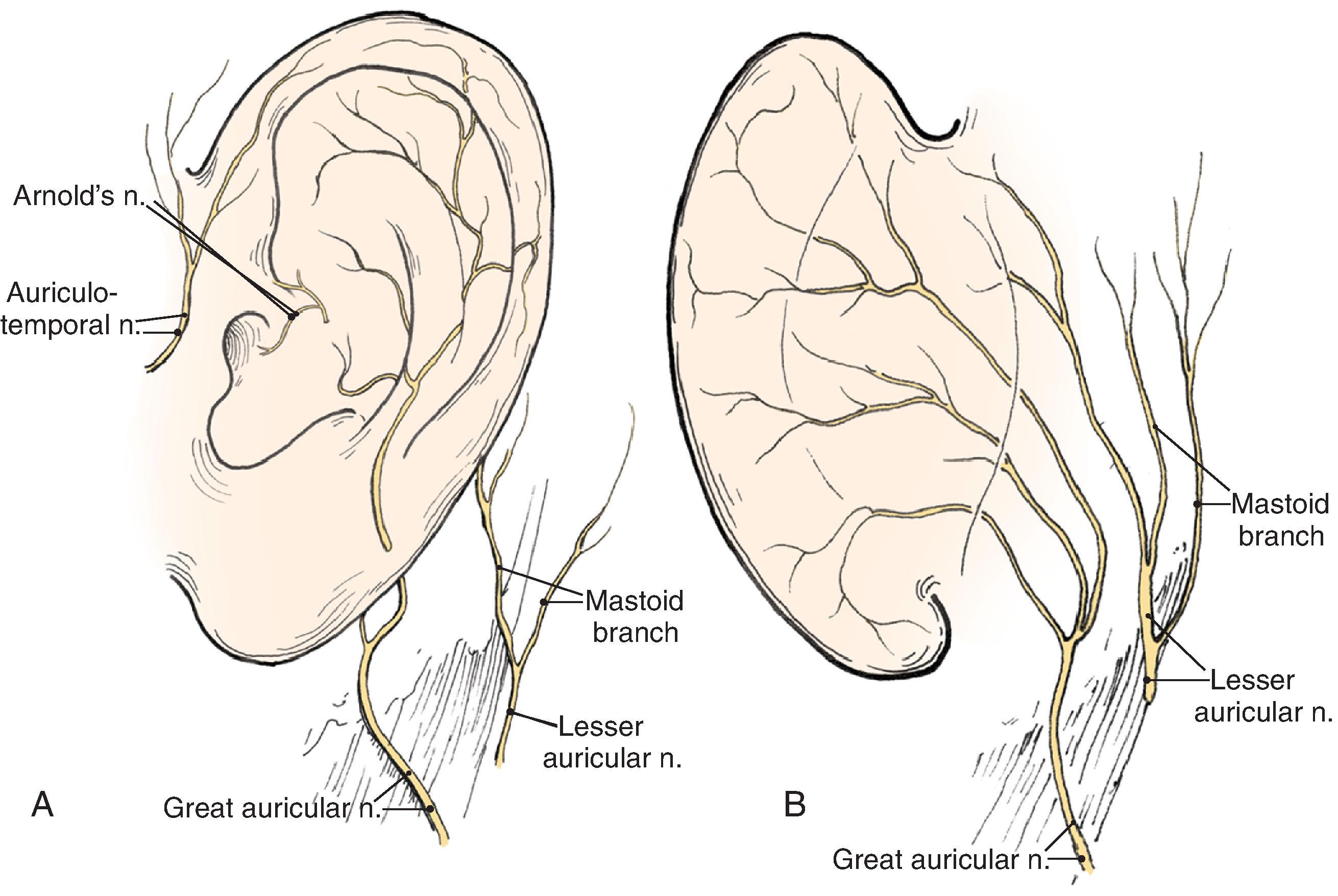
The auricle is innervated by contributions from both cranial and spinal nerves. They include the great auricular nerve (C2-3), the auriculotemporal nerve (V3), the lesser occipital nerve (C2-3), and a branch of the vagus nerve (X; Arnold’s nerve; Fig. 22.3 ). The great auricular nerve divides into an anterior and posterior branch. The anterior branch supplies the lower half of the lateral aspect of the auricle. The posterior branch supplies a similar area on the medial surface of the auricle. The auriculotemporal nerve supplies the superolateral surface of the auricle. The lesser occipital nerve supplies the superior aspect of the ear on the medial side. The concha is supplied by Arnold’s nerve.
Embryologically, the auricle arises from the first and second branchial arches. Hillocks appear in these arches during the sixth week of gestation. The anterior hillock gives rise to the tragus, the root of the helix, and the superior helix, whereas the posterior hillock becomes the antihelix, tragus, and lobule. The first branchial groove forms the external auditory meatus and concha.
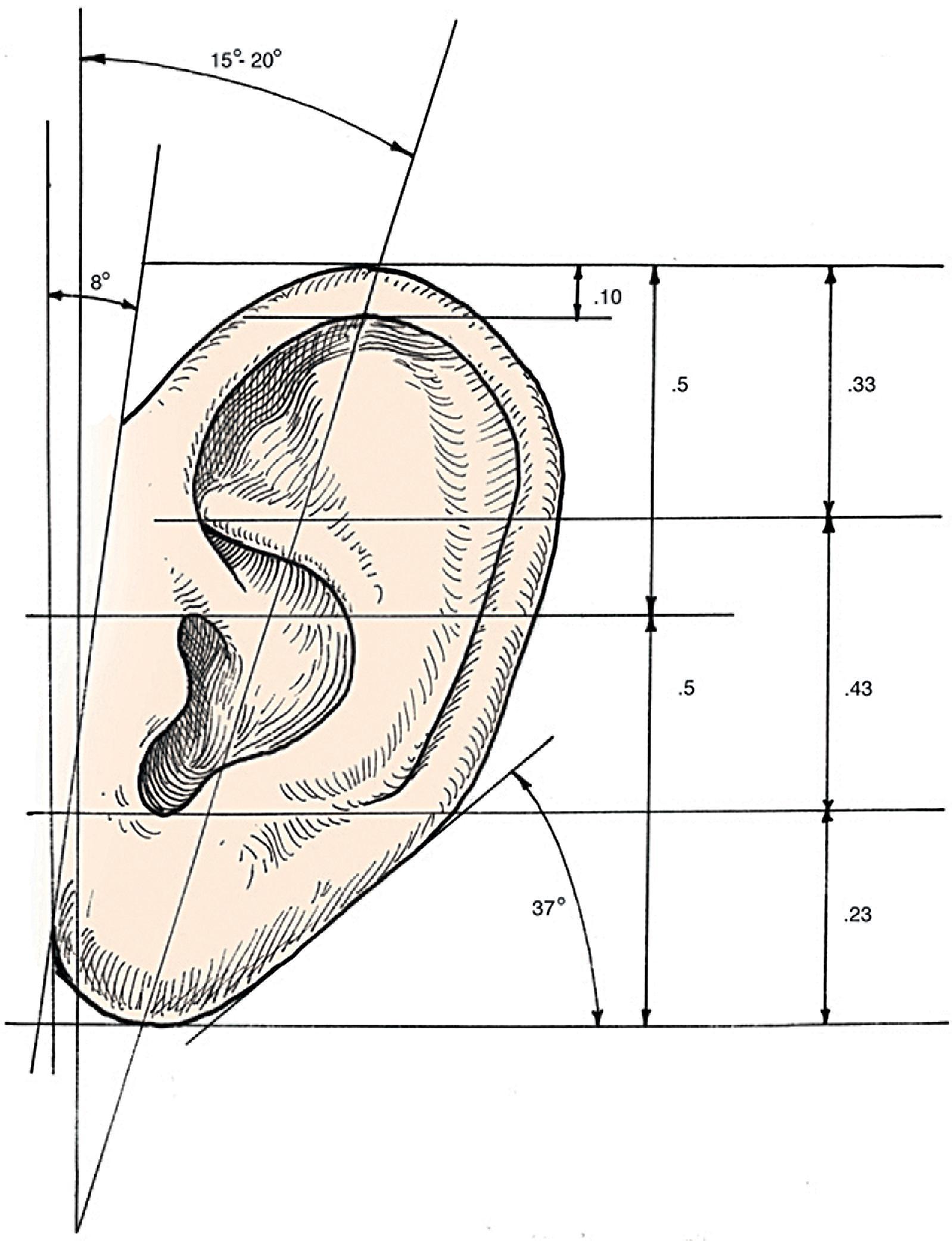
Analysis of the dimensions and proportions of the external ear are important for planning reconstructive procedures. The vertical height of the ear roughly matches the distance between the lateral orbital rim and the root of the helix at the level of the eyebrow. Ear width is approximately 55% of its length ( Fig. 22.4 ), and the helical rim protrudes 1 to 2.5 cm from the skull. The angle of protrusion from the skull typically ranges from 25º to 30º. The vertical axis of the ear is inclined posteriorly at an angle of approximately 15º to 20°. , The original anatomic descriptions of auricular orientation suggested that the long axis of the ear was roughly parallel to the dorsum of the nose, but it is now widely recognized that the ear is rotated 10º anterior to that plane. The superior level of the ear matches the level of the lateral eyebrow. To account for individual variations in topographic features, positioning, and symmetry, the contralateral ear is used as a template when planning reconstruction, rather than strict adherence to textbook-defined norms. The most important principal of auricular reconstruction is that the size, location, and orientation of the reconstructed ear is similar to the normal ear. The dominant features that make an ear recognizable are the helix, tragus, antitragus, and conchal bowl.
Auricular defects may be divided into defects of cutaneous coverage, with or without intact cartilage, and defects that are full-thickness. Small cutaneous defects of the helical rim may be reconstructed with primary wound closure and occasionally require small excisions of cartilage to avoid distortion. Defects of the densely adherent lateral auricular skin can rarely be closed primarily, whereas those of the more pliable medial surface can often be repaired primarily. The pliability of medial auricular skin permits the harvest of relatively large postauricular skin grafts with primary closure of the donor site. Lateral cutaneous defects that have intact cartilage are best treated with skin grafts, provided there is intact perichondrium over the exposed cartilage. The contralateral postauricular skin is an excellent donor site for a full-thickness skin graft used to resurface the lateral ear. Preauricular skin may also be used with minimal donor site morbidity. In cases where the perichondrium is absent, resulting in an avascular surface, cartilage may be removed if it is not critical to auricular shape (see examples in Chapter 15 ). Windows created through the cartilage provide surface contact between the graft and the vascularized subcutaneous tissue of the medial aspect of the auricle. The cartilage of the concha, fossa triangularis, and scapha are amenable to partial removal without loss of structural integrity of the ear. The cartilaginous windows provide access to the perichondrium of the medial aspect of the ear, which in turn provides sufficient vascularity for successful skin grafting.
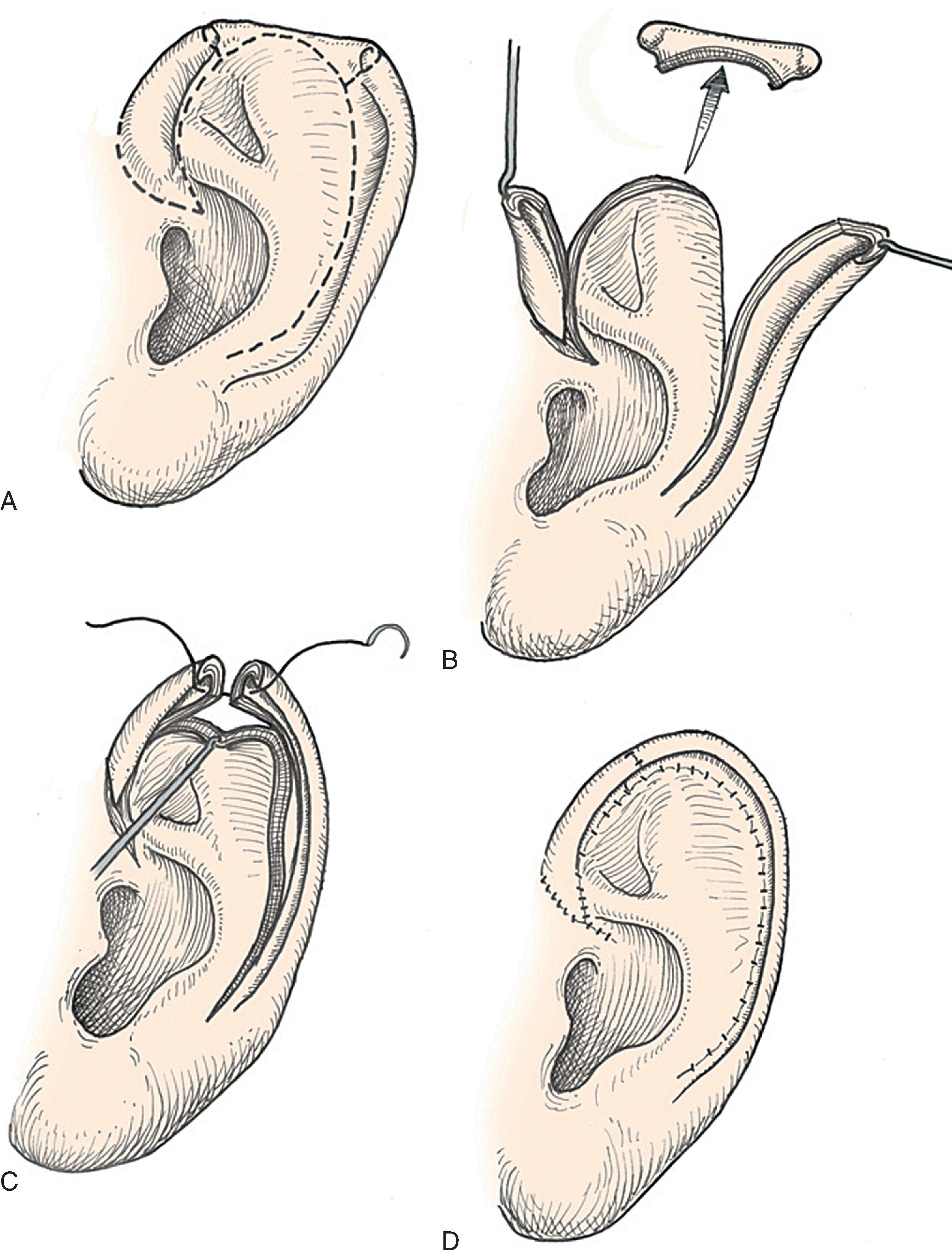
Surgical approaches for reconstruction of defects of skin and underlying cartilage include converting the defect into a full-thickness, wedge-shaped excision, followed by primary wound closure, or employing a composite graft or flap that incorporates structural support. The size and location of the defect dictate which alternative is most appropriate. Defects less than 1.5 cm of the helix or antihelix are best repaired by conversion to a wedge-shaped excision. The wound is then repaired primarily, and results in a minimally visible scar. Although this approach does reduce vertical height of the ear, the difference with the contralateral ear is usually not conspicuous. When performing a wedge-shaped excision of the auricle, excessive wound closure tension is avoided by removing a portion of the concha to accommodate advancement of the two borders of the ear defect. If this is not performed, cupping and distortion of the ear will occur. Medium-sized helical defects, from 1.5 to 2 cm, can be managed by composite grafting from the contralateral ear. Typically a composite graft one-half the size of the defect is transplanted from the opposite ear, thereby creating two ears of equal size ( Fig. 22.5 ). The cartilage edges of the graft and the recipient site are securely approximated with a row of interrupted sutures. Graft immobilization is essential for proper healing and can be accomplished by using bolster sutures to secure a splint over the ear. De-epithelializing the medial aspect of the composite graft and implanting it into a subcutaneous recipient site have been described. The graft is released from its soft tissue attachment in a second surgical stage. This approach is designed to increase graft survival. Transfer of composite grafts from the contralateral ear exposes both ears to some risk for infection and deformity, so its use must be carefully considered in view of this risk.

Many local flaps have been described for repair of full-thickness auricular defects. Chondrocutaneous composite advancement flaps are best suited to repair full-thickness helical rim defects. Helical chondrocutaneous composite flaps take advantage of the available tissue of the remaining helical rim and the redundant lax skin of the lobule. Anteriorly, a V-to-Y advancement of the helical root designed as an island flap is usually combined with a posterior chondrocutaneous composite advancement flap to achieve closure of helical rim defects ( Fig. 22.6 ). Chondrocutaneous composite flaps may be advanced with the medial skin intact or incised. Although Antia originally described keeping the medial skin intact, there is greater ease of flap advancement with at least a limited incision of the medial skin. The arterial network of the helix-scapha region allows for the creation of long chondrocutaneous composite flaps on a narrow pedicle. Depending on the size of the helical defect, Burow triangles are excised to facilitate advancement of the flaps ( Figs. 22.7 and 22.8 ). Chondrocutaneous flaps in the form of transposition flaps may also be used for reconstruction of nonhelical defects.


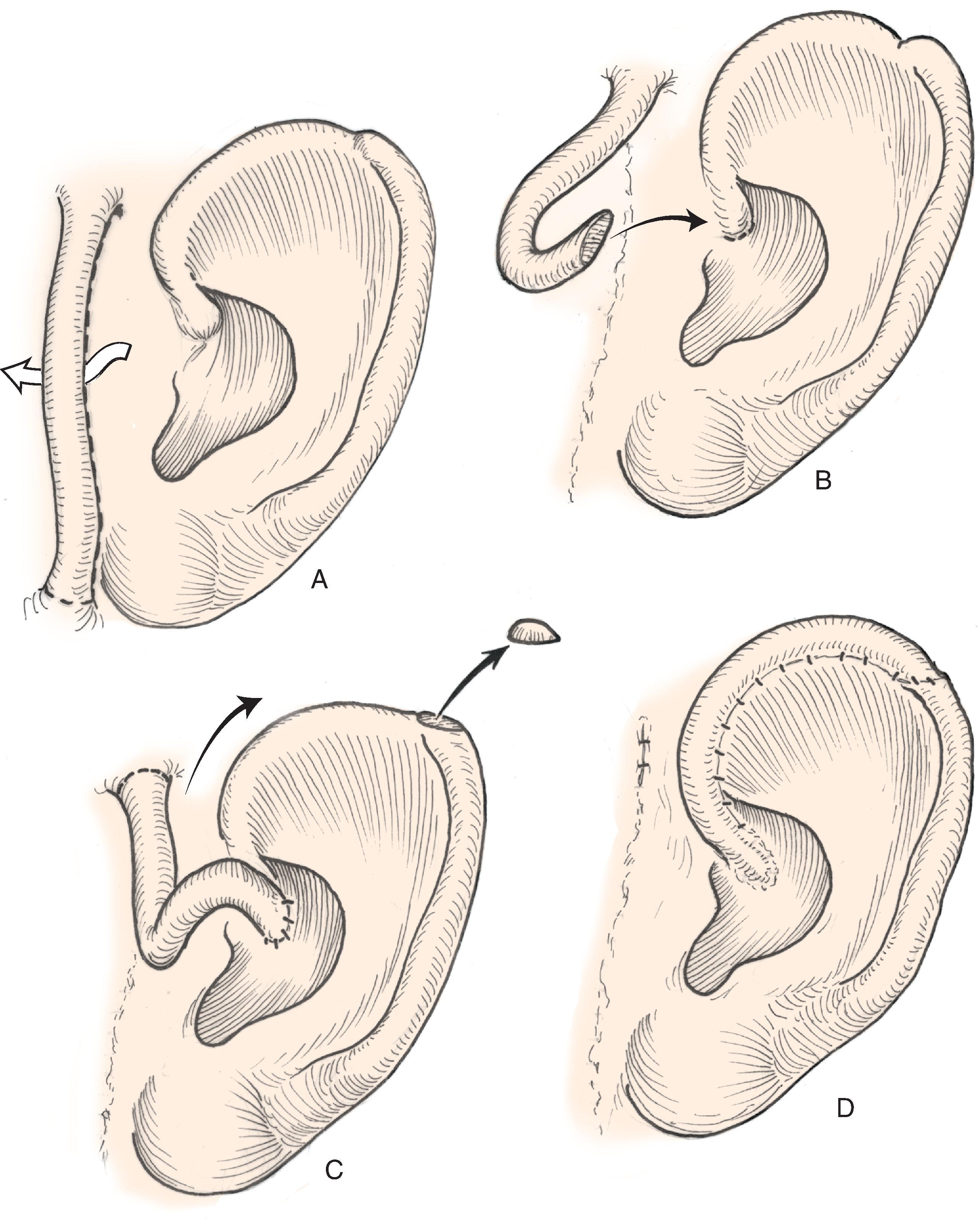
Both postauricular and preauricular skin serve as ideal donor sites for the creation of interpolated tube flaps. These flaps are used to reconstruct longer segments of the helical rim that are too large for reconstruction using a chondrocutaneous advancement flap. Initially, the flap is dissected as a bipedicled flap that is tubed upon itself ( Fig. 22.9 , A ). After 3 weeks, one end of the cutaneous tube is detached from its origin and secured to one border of the helical rim defect. Three weeks later, the other end of the tube is incised and inset in the other border of the helical defect. Interpolated tube flaps are most useful for reconstructing defects confined to the helical rim that are greater than 2.5 cm in length ( Fig. 22.10 , E , F ).

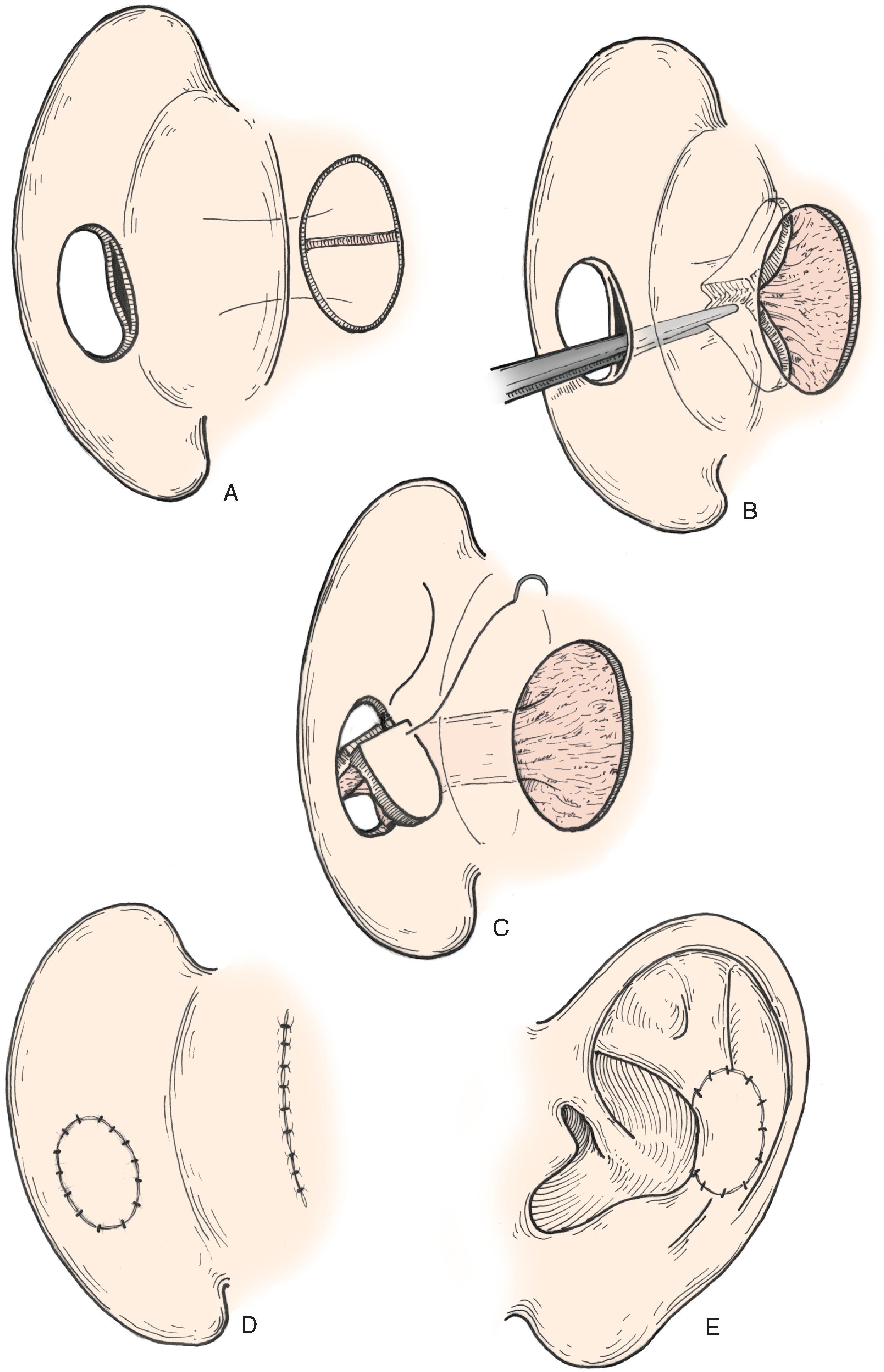
Postauricular island advancement flaps work well for conchal reconstruction and repair of full-thickness defects of the nonhelical portions of the ear. , The postauricular flap is based on the auricular branch of the postauricular artery. The flap is designed as an island based on a subcutaneous tissue pedicle. A significant advantage is that it provides a single stage repair with easy closure of the postauricular donor site. When designed as an island, the flap is outlined and incised deeply through the postauricular muscle. Posteriorly, the mastoid periosteum is incised, and the dissection proceeds in a superior and anterior direction. Care is taken to preserve the vascular supply to the flap as it enters the flap inferiorly. With the subcutaneous pedicle intact, the flap is advanced into its respective conchal or nonmarginal auricular defect ( Fig. 22.11 ). Postauricular flaps may also be developed as interpolated flaps, requiring a subsequent stage to inset the flap. Interpolated postauricular flaps have been described as a single stage procedure, which is accomplished by de-epithelializing the skin of the flap’s pedicle. , A modification has also been described that consists of harvesting the flap from the medial surface of the auricle to repair a skin defect of the lateral surface. The technique requires de-epithelialization of a portion of the pedicle.
The principles set forth by Tanzer and colleagues for microtia reconstruction are germane to reconstruction of large acquired auricular defects. , Use of a three-dimensional autologous rib cartilage framework with soft tissue coverage is the mainstay of microtia repair. Similar structural frameworks may be used for reconstruction of large full-thickness auricular defects. Success depends on the use of supple, thin, and highly vascular skin flaps to cover cartilage grafts and to ensure a refined contour of the reconstructed ear. When local skin is scarred or absent, as is often the case with acquired defects, a temporoparietal fascia flap may provide the necessary thin, highly vascular covering for cartilage grafts and concomitantly serve as the recipient site for overlying split- or full-thickness skin grafting. When the vertical height of the ear is likely to diminish by more than 20 mm by using a local flap, repair with a regional flap is more appropriate. The temporoparietal fascia flap, combined with autologous cartilage grafting to replace auricular framework deficiencies, has proven to be the most versatile regional flap for reconstruction of larger full-thickness ear defects.
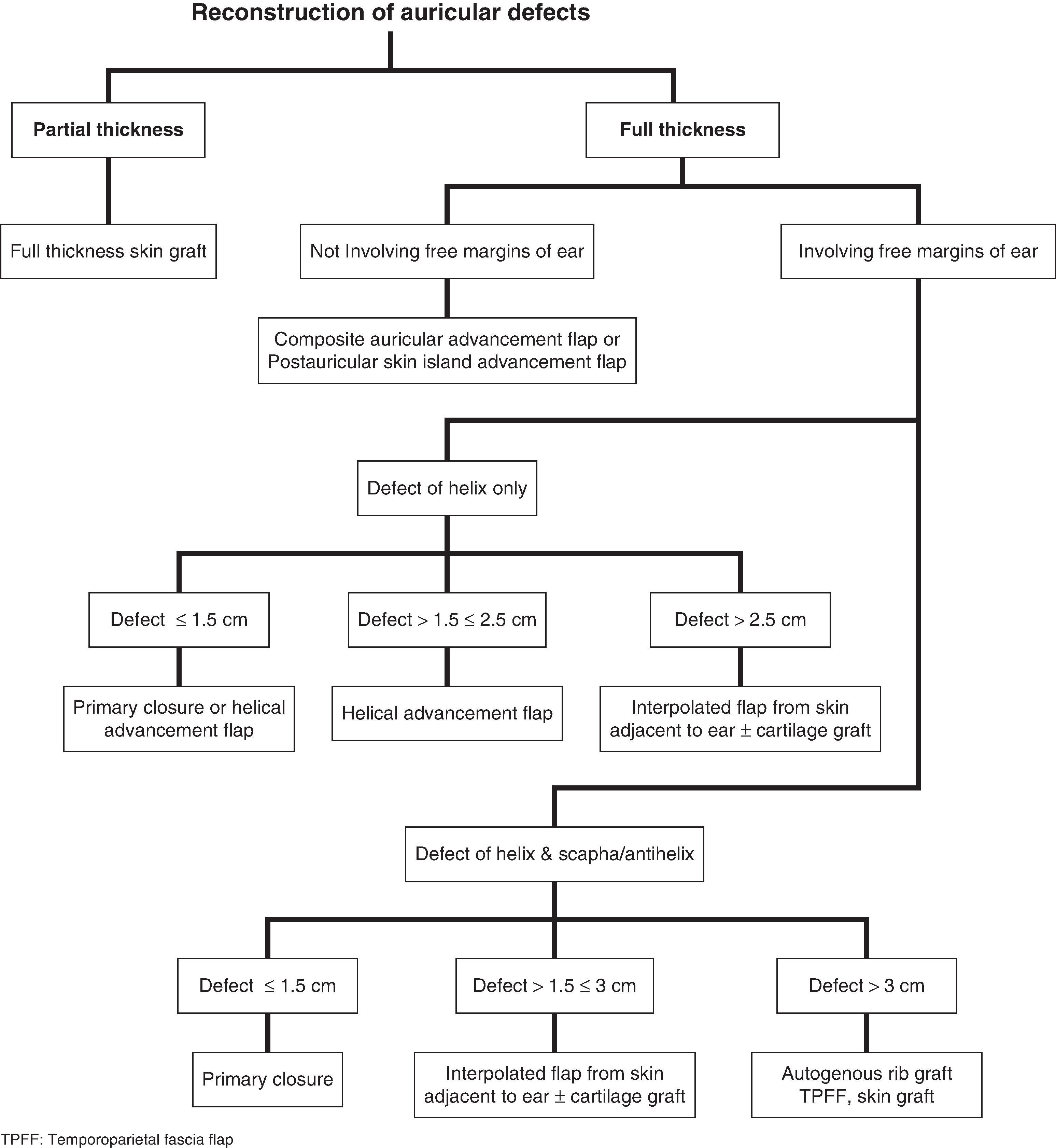
In planning auricular reconstruction, one must consider each missing component of the ear. A logical approach to a discussion of reconstructing acquired auricular defects is to divide them into those consisting of skin, skin and cartilage, and full-thickness ( Fig. 22.12 ). Such a discussion is also best presented according to anatomic location because of the variable availability of local and regional tissue in each of these locations.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here