Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cutaneous conditions of the head and neck are both common and diverse.
Identification of these conditions is often required of an otolaryngologist; although many cutaneous lesions can be identified based upon clinical appearance, biopsy is necessary for definitive diagnosis.
Benign lesions are often a cause for cosmetic concern; a variety of treatment options exists, including surgical methods and laser destruction.
Nevi should be evaluated for A symmetry, B order irregularity, C olor change, D iameter, and E volution over time.
Basal cell carcinoma is the most common form of cancer in humans, but melanoma causes the most deaths from skin cancer.
The otolaryngologist is frequently called upon to deliver the diagnosis of a skin lesion. In consultation or in passing, you could be the only one who notices that insidious melanoma. Perhaps the condition is a manifestation of a systemic illness that can be unmasked by the practical knowledge delivered in this chapter. If you diagnose one of the numerous benign skin lesions, you may confidently provide treatment options previously unknown to the patient for a cosmetically concerning lesion. This chapter will review the critical benign and malignant cutaneous lesions that may be encountered on the head and neck as well as their treatment. Management of advanced cutaneous malignancies, melanoma, and vascular anomalies will not be covered and can be found in Chapters 94 and 204 .
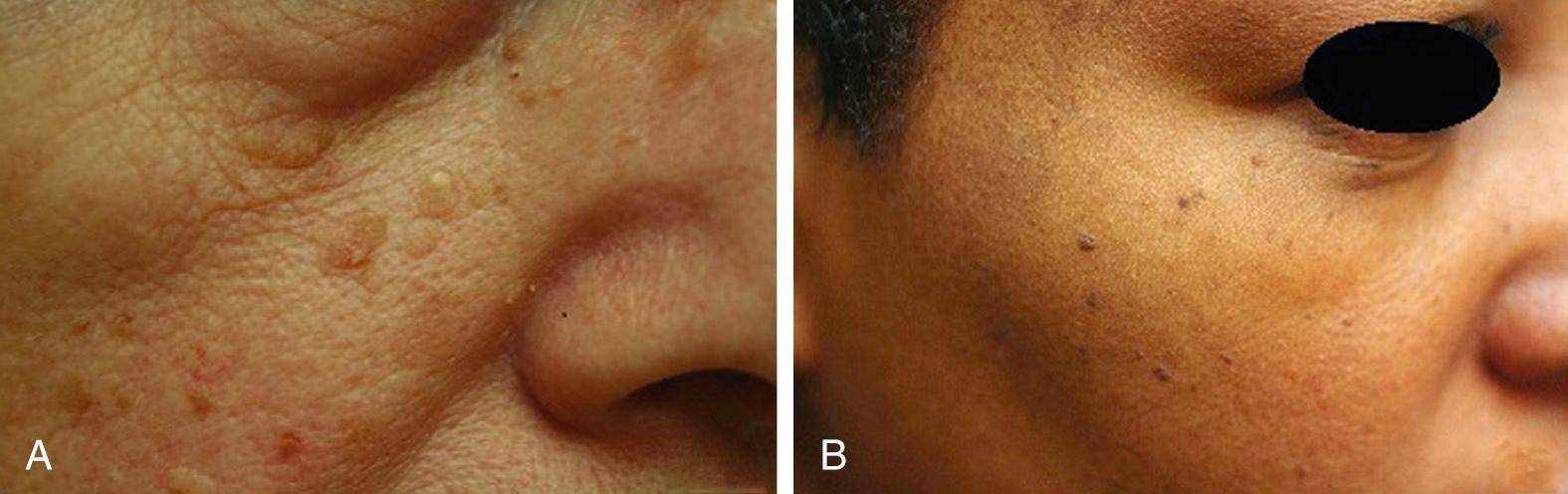
Seborrheic keratoses are common epidermal lesions ( Fig. 17.1 ). Although frequently found on the head and neck, seborrheic keratosis is most commonly located on the trunk. These lesions seldom appear before the third decade. Clinically, seborrheic keratoses appear as tan to darkly pigmented waxy, verrucous papules.
Patients may desire removal of seborrheic keratoses that become irritated or pruritic or for cosmesis. Lesions can be removed with cryotherapy alone, cryotherapy and curettage, or electrodessication and curettage. Removal with ablative lasers, and, more recently, fractional ablative lasers, has been described in select patients. A study comparing erbium:yttrium aluminum garnet (Erb:YAG) laser with cryotherapy for the treatment of seborrheic keratosis found an improved healing rate and a lower rate of pigment alteration with the use of laser.
One variant of the seborrheic keratosis is dermatosis papulosa nigra (see Fig. 17.1 ). Found in individuals of Asian or African descent, these black seborrheic keratoses cluster in the periocular region. Individuals with dermatosis papulosa nigra have numerous small, sometimes, pedunculated lesions. The condition tends to be familial.
Dermatosis papulosa nigra can be treated similarly to seborrheic keratoses. However, because the condition typically occurs in more darkly pigmented individuals, care must be taken to avoid postinflammatory pigment alteration. Cryotherapy frequently results in hypopigmentation, and electrodessication can cause postinflammatory hyperpigmentation. The potassium-titanyl-phosphate (KTP) laser and the carbon dioxide laser have been described as treatment modalities with minimal risk of pigment alteration. With any treatment, test areas should be performed prior to treating an entire area to avoid unwanted consequences.
An epidermal nevus is a rare congenital verrucous lesion. On close examination, one can observe the individual minute papules that coalesce into a larger plaque along the lines of Blaschko. Epidermal nevi are hamartomatous lesions that result from a postzygotic mutation in an embryonic cell that populates a region of epidermis. Variants of epidermal nevi include classic epidermal nevus, nevus comedonicus, and nevus sebaceous. Epidermal nevi may be isolated or found as part of a syndrome with skeletal and central nervous system anomalies.
If cosmetically or functionally undesirable, epidermal nevi can be flattened with an ablative laser, such as the carbon dioxide or Erb:YAG; however, recurrence is common. If size permits, the lesion may be excised in its entirety, although scarring may be marked with this approach.
Verruca vulgaris or common warts are caused by the human papilloma virus (HPV). On the head and neck, verrucae may have a filiform appearance. Lesions may be solitary or multiple and may spread with shaving. Verrucae are most commonly caused by HPV types 1, 2, 27, and 57.
Verrucae may be treated with cryotherapy, using liquid nitrogen. Often, multiple treatments are needed for complete resolution, usually 3 to 4 weeks apart. Electrosurgery and laser ablation may be performed but precautions must be taken to prevent the spread of the virus during therapy, as ablative treatments have been documented to aerosolize viral particles and may lead to further viral spread. Topical imiquimod has been approved by the US Food and Drug Administration for the treatment of genital warts. This therapy may be offered, off-label, for the treatment of multiple verrucae of the skin. Pulsed dye laser is another option for recalcitrant lesions.
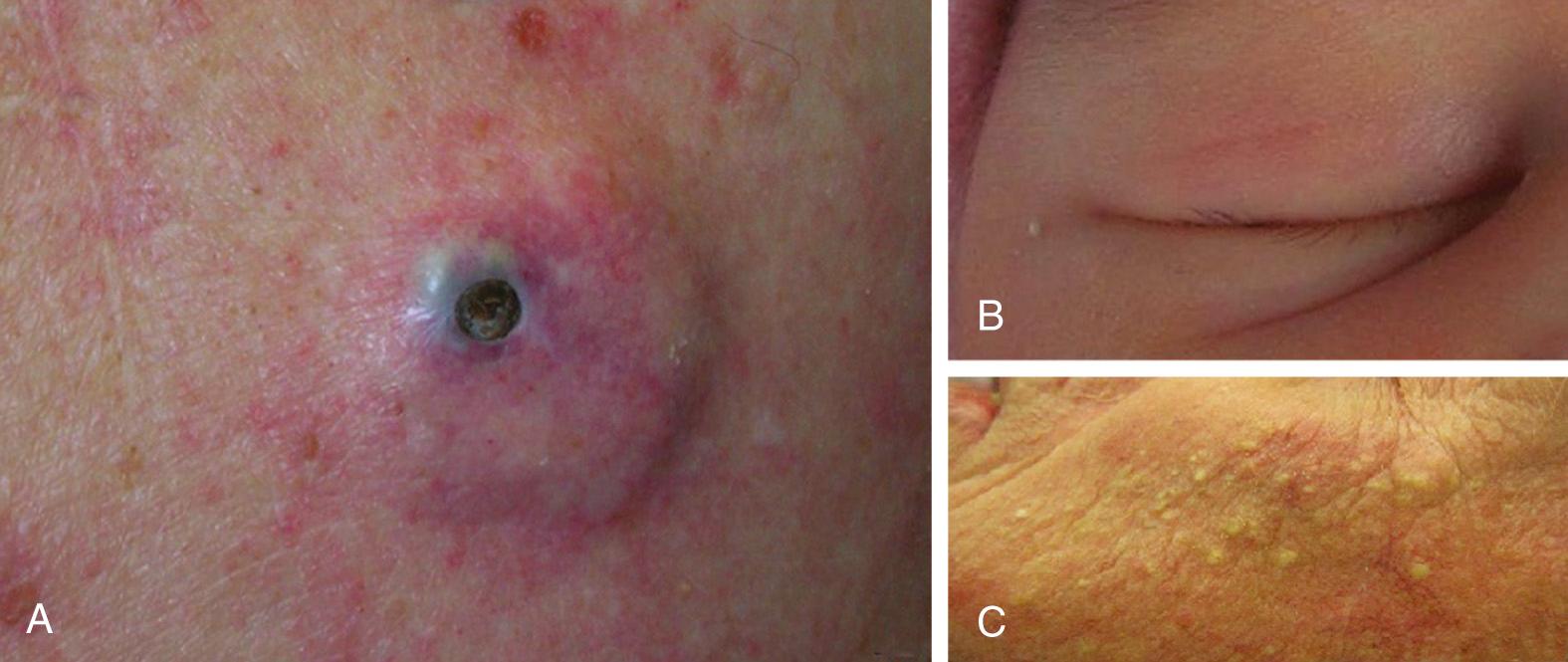
Epidermal inclusion cysts are common subcutaneous lesions ( Fig. 17.2 ). These lesions range in size from several millimeters to several centimeters, and often have a central punctum that may drain a foul-smelling, cheesy substance. Also known as keratin cysts or sebaceous cysts , the lesions may remain dormant for years. When inflamed, epidermal inclusion cysts can dramatically increase in size, be painful, and have overlying erythema. Histologically, epidermal inclusion cysts are characterized by columnar epithelial cells lining a keratin-filled sac.
Inflamed cysts can be treated with intralesional steroids. Severely inflamed cysts may become secondarily infected and require incision and drainage along with antibiotic therapy. Both aerobic and anaerobic microorganisms have been identified in inflamed epidermal cysts. Definitive therapy is surgical excision, but this should be performed once inflammation has ceased to avoid postoperative infection and greater scarring. Prophylactic excision of noninflamed lesions can be performed to prevent future problems and can usually be accomplished by removing a small overlying ellipse of skin.
A variant of the epidermal inclusion cyst localized to the hair-bearing scalp is the pilar or trichilemmal cyst. Unlike other cutaneous epidermal inclusion cysts, pilar cysts often lack a central punctum and are usually more solid to the touch. Pilar cysts are less likely to become inflamed when compared with epidermal inclusion cysts on other parts of the body, but may be irritated with combing and grooming.
Treatment is with surgical excision. Very rarely, histopathological evaluation of a presumed pilar cyst may make the diagnosis of a proliferating trichilemmal tumor. Hence, it is of paramount importance to submit the excised tissue for review, as proliferating trichilemmal tumors have potential for malignant transformation.
Milia are small (typically <3 mm), white, superficial epidermal inclusion cysts, frequently found on the face (see Fig. 17.2 ). Milia are usually primary lesions, but may result secondarily to injury of the skin. The lesions are benign and usually asymptomatic, but may be of cosmetic concern.
Milia may be removed by nicking with a 19-gauge needle or 11 blade before applying gentle pressure with a comedone extractor. Smaller lesions may respond to microdermabrasion or off-label topical therapy with a high potency retinoid.
Favre-Racouchot disease is a condition characterized by open comedones and milia-like cysts in the periocular region (see Fig. 17.2 ). The condition tends to affect elderly white men and is related to chronic sun exposure.
For improved cosmesis, individual lesions may be treated by comedone and milium extraction. High potency retinoids may aid in the removal of lesions and/or prevent new lesions from forming. Laser treatment with the carbon dioxide laser has also been reported.
Dermoid cysts are benign subcutaneous nodules that appear at birth or during childhood as small (usually <2 cm) isolated lesions, typically on the head. These lesions are formed prenatally due to entrapment of the epidermis along the lines of embryonic fusion. Dermoid cysts are frequently asymptomatic, and the most common location for a dermoid cyst is along the lateral brow.
When located in the midline or overlying a cranial suture, imaging should be obtained to identify any intracranial extension. Lesions may be surgically excised. Postauricular temporal bone dermoid cysts seem to form a distinct subgroup with a lesser tendency toward deep extension and are amenable to more conservative management strategies.
Melanocytic nevi of the head and neck are a common concern among patients. Nevi come in a variety of subtypes, including compound, intradermal, junctional, dysplastic, and Spitz ( Fig. 17.3 ). Compound and intradermal nevi are well-circumscribed, dome-shaped papules frequently localized to the head and neck. The former are hyperpigmented, and the latter are skin-colored or slightly erythematous. Lesions are usually asymptomatic, but may be irritated with shaving or rubbed by clothing. Junctional nevi are flat, benign, macules of even pigmentation. Dysplastic nevi share features of pigment irregularity and uneven borders with malignant melanoma. As a result, surgical removal is recommended to ascertain diagnosis. A Spitz nevus is a less common melanocytic lesion that clinically appears as an erythematous papule on the head of a child or adolescent. Definitive diagnosis is made histologically, and if cytologic atypia is noted, further resection is recommended.

One of the most important qualities required of the head and neck surgeon is the ability to discern a benign from a malignant melanocytic lesion. Often the distinction cannot be made upon clinical evaluation alone, and a biopsy for histopathological evaluation is needed. If melanoma or dysplastic nevus is suspected, an excisional biopsy should be performed to aid in the diagnosis and guide appropriate therapy. If complete surgical excision is not practical given the extent of the lesion, an incisional biopsy may be performed, with the understanding that sampling bias may exist. Indications for biopsy include asymmetry of the lesion, border irregularity, color variegation, diameter >6 mm, and evolution or change of the lesion.
If cosmetic removal of a benign lesion is desired, lesions may be surgically treated. Benign dermal nevi may be flattened with shave removal, although recurrence may occur with this method. Treatment with the quality-switched neodymium-doped: yttrium aluminum garnet (Q-switched Nd:YAG) laser will result in lightening of the lesions, although most clinicians advocate surgical removal for submission of tissue for histopathological evaluation.
Lentigenes are macular hyperpigmented lesions commonly found on the head and neck in older individuals (see Fig. 17.3 ). Lentigenes are photo-induced and darken upon sun exposure. Histologically, these lesions are characterized by a proliferation of benign melanocytes at the dermoepidermal junction. Lentigenes clinically are usually more well-defined and of more even pigment than the malignant melanocytic lesions lentigo maligna or melanoma in situ. In cases of clinical ambiguity, a biopsy can distinguish between the two.
Once a benign diagnosis has been rendered, elective removal may be considered. Strict photoprotection is necessary to prevent darkening of existing lentigenes as well as the appearance of new lesions. Individual lentigenes may be removed with the Q-switched Nd:YAG laser. If diffuse lentigenes are present, intense pulsed light may be a more practical method of lightening. Multiple treatments are sometimes necessary, and recurrence upon exposure to sunlight is typical. Cryotherapy has demonstrated efficacy in solitary lesions as melanocytes are selectively destroyed at low temperature. Another alternative is topical therapy with 2% to 4% hydroquinone, alone or in combination with a retinoid and steroid. Finally, chemical peels can be used to lighten these hyperpigmented lesions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here