Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The erythemas in this chapter are generally viewed as reactions to infections , drugs , malignancies , or other miscellaneous things. They are generally more dermal , having less scale or epidermal changes than the diseases in Chapter 2 . The erythema blanches , and there is no purpura or vasculitis as in Chapter 4 . When erythemas make rings, they are annular (1.5), and are sometimes called gyrate erythemas . When they have an acute onset, are bright red and edematous, and often accompanied by palm and sole involvement or fever, then sometimes clinicians invoke the poorly defined term toxic erythema . Toxic erythema can include conditions outside of this chapter, such as scarlet fever (12.2), toxic shock syndrome (12.2), Kawasaki’s syndrome (14.10), and acute graft-versus-host disease (17.3).
(see Fig. 3.1 )
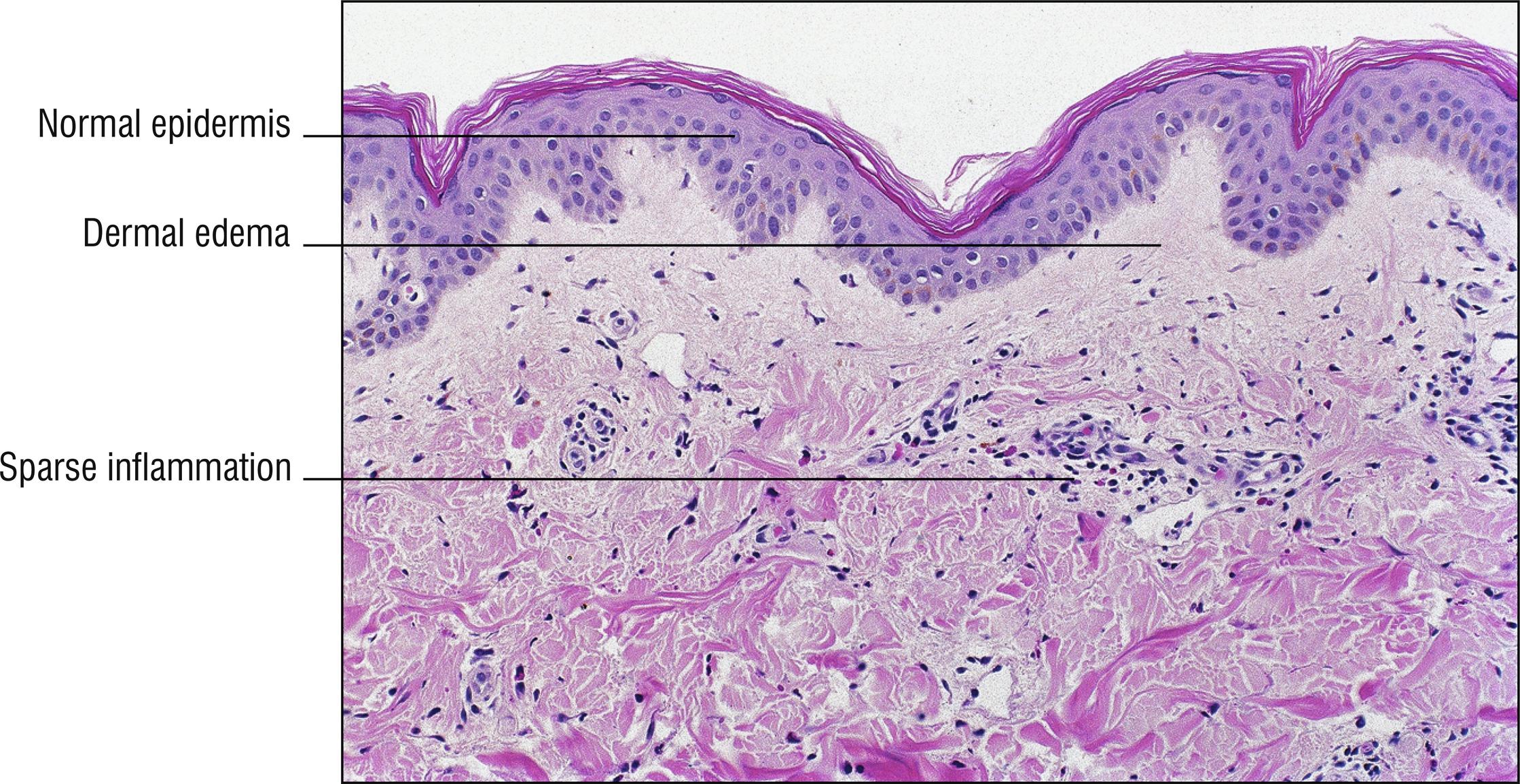
Common, occurs in 20% of the population sometime in their lifetime, evanescent wheals (hives) that move around hour by hour or at least within 24 hours, very pruritic (1.114), IgE mediated type I hypersensitivity to foods, drugs, infection, or idiopathic factors. May have dermatographism. Airway obstruction due to laryngeal edema may occur in severe cases.
Epidermis normal
Dermal edema
Sparse perivascular and interstitial eosinophils , lymphocytes , neutrophils (1.89), and/or mast cells (1.78)
Acute urticaria: usually lasts less than a month, higher chance of specific etiology being found.
Chronic urticaria: lasts more than a month, and may last for years, idiopathic in 90% of cases, less likely related to IgE.
Cold urticaria: more in children and young adults, related to cold exposure (lesions reproduced with ice cube test).
Solar urticaria: appears within hours of sun exposure (photodermatitis, 1.110).
Cholinergic urticaria: small papules appear after exercise.
Pressure urticaria: pressure on skin of hands, feet, or buttocks induces lesions.
Hereditary angioedema: autosomal dominant, prominent facial or lip edema, usually without urticaria, decreased levels or dysfunction of Cl esterase inhibitor.
Angioedema with acute urticaria: may have fever, leukocytosis, no family history, less inflammatory cells in skin and more edema, with tendency to extend deeper into subcutaneous fat.
Erythema marginatum: variant of urticaria that is faint, very evanescent, occurring with rheumatic fever (12.2).
Papular urticaria (15.7): related to arthropod bites.
Urticaria multiforme: Targetoid lesions resemble erythema multiforme (3.2), but lesions are still evanescent. Often acral edema. Common in children, often related to viruses or drugs.
Schnitzler syndrome: Urticaria with monoclonal gammopathy (1.80). Also may include fever, bone and joint pain, weight loss, malaise, fatigue, adenopathy, and hepatosplenomegaly.
Other diseases with dermal eosinophils (1.36).
Other diseases with dermal edema (1.30).
Other diseases with normal-appearing histology (1.94), perivascular (1.109), or interstitial dermatitis (1.65).
Urticarial vasculitis (4.1): mainly considered clinically when lesions are not evanescent.
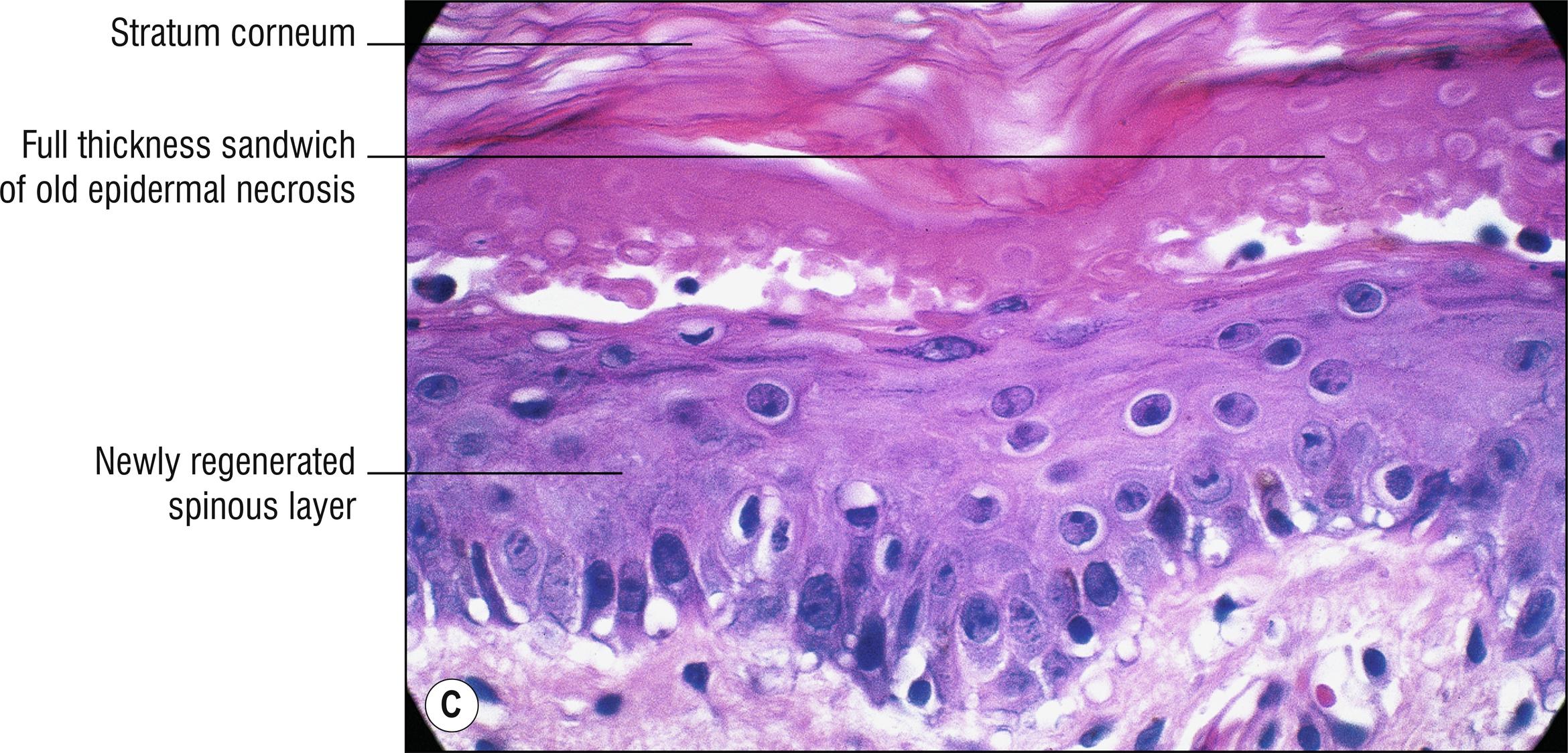
(see Fig. 3.2A–D )
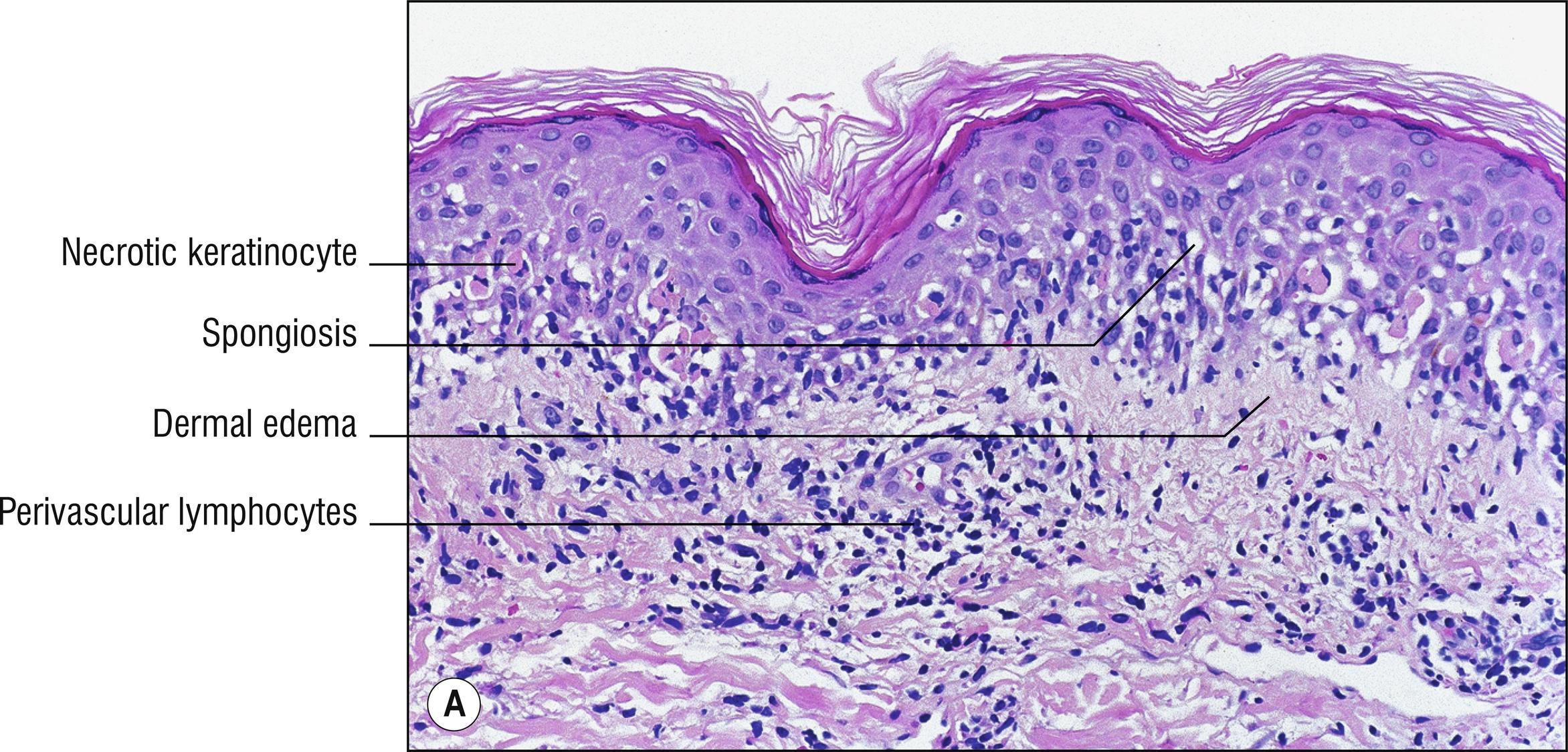
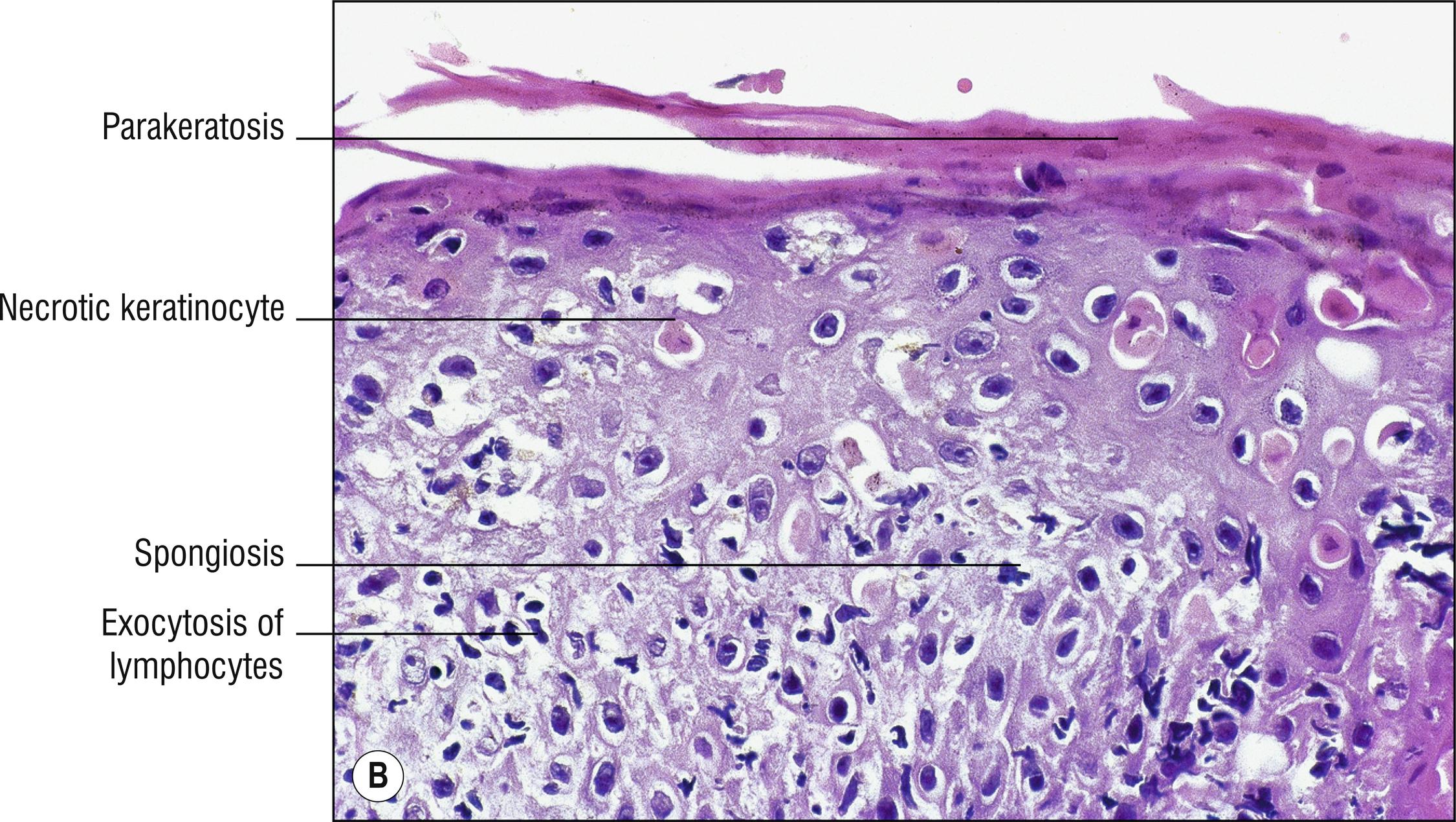
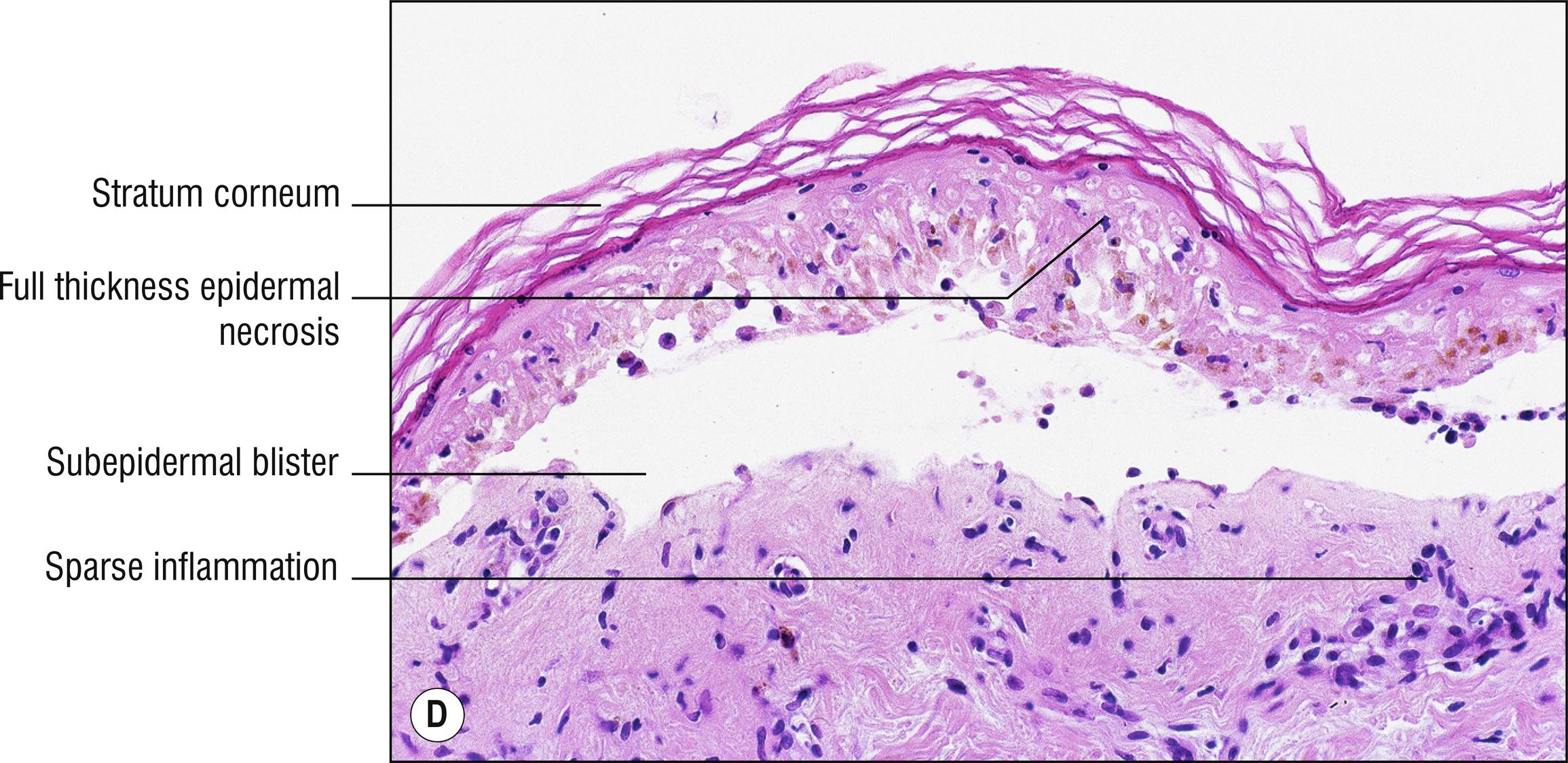
Common, acute onset , multiform lesions (papules, urticarial plaques, targets [1.5], blisters), often recurrent , especially on acral skin more than the trunk, common on the palms (1.100). Mostly in children and young adults . If classic targets are present, it is almost always a reaction to herpes simplex infection (14.2). A wide variety of drugs (3.5) and infections are the cause in other cases. Although some authors refer to “epidermal” and “dermal” types of erythema multiforme, this is just a function of what type of lesion is biopsied.
Necrotic keratinocytes
Sometimes spongiosis (1.132), rarely intraepidermal vesicles
Basal layer liquefaction (1.64), sometimes subepidermal blister (1.147)
Edema of the papillary dermis (1.30)
Perivascular or interface lymphocytes (1.64), rarely with eosinophils (1.36)
Extravasated erythrocytes sometimes (1.40)
Stevens–Johnson syndrome: more mucous membrane involvement and more epidermal necrosis. Some authorities attempt to define it differently based upon the amount of body surface area involved, making the inane statement that Stevens–Johnson syndrome involves less than 10% body surface area, whereas toxic epidermal necrolysis involves more than 30%, with 10–30% involvement constituting an overlap zone. This is ridiculous because it makes no sense to change the diagnosis if the disease worsens.
Toxic epidermal necrolysis (TEN): extensive sloughing of full-thickness necrotic skin, higher body surface area involved than Stevens–Johnson syndrome, may be life-threatening (prognosis calculated by SCORTEN scoring system), usually due to sulfonamides, phenytoin, and other drugs.
Necrolytic migratory erythema (glucagonoma syndrome): crusted plaques, especially mouth, perioral, and acral skin, elevated serum glucagon level, psoriasiform (1.119), tendency for only the superficial epidermis to be necrotic and pale (1.99), underlying glucagonoma may not be found in all cases.
Fixed drug reaction (3.5): similar to erythema multiforme, but localized to a fixed site, associated with drugs.
Erythrodysesthesia syndrome (3.5).
Urticaria multiforme: A clinical term used when lesions have overlapping appearances between urticaria (3.1) and erythema multiforme.
MIRM: Mycoplasma pneumoniae –induced rash and mucositis.
Paraneoplastic pemphigus (5.4): necrotic keratinocytes more prominent than acantholysis, so it is easily mistaken for erythema multiforme clinically and histologically.
Rowell syndrome and other lupus erythematosus variants (17.6): lupus erythematosus with necrotic keratinocytes resembling erythema multiforme. ASAP syndrome resembles TEN.
Other diseases with necrotic keratinocytes (1.86) or perivascular lymphocytes (1.109).
(see Fig. 3.3A,B )
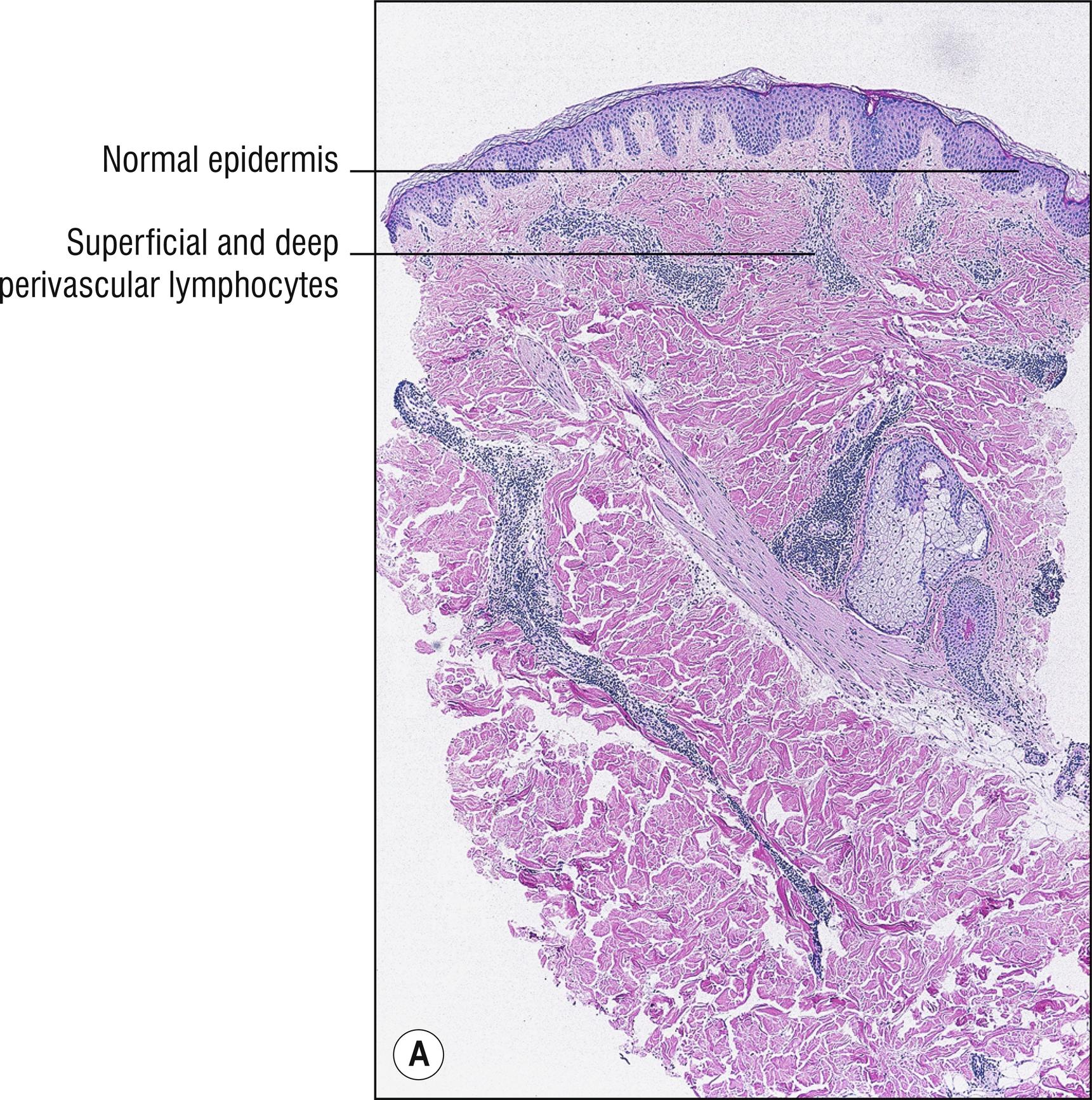
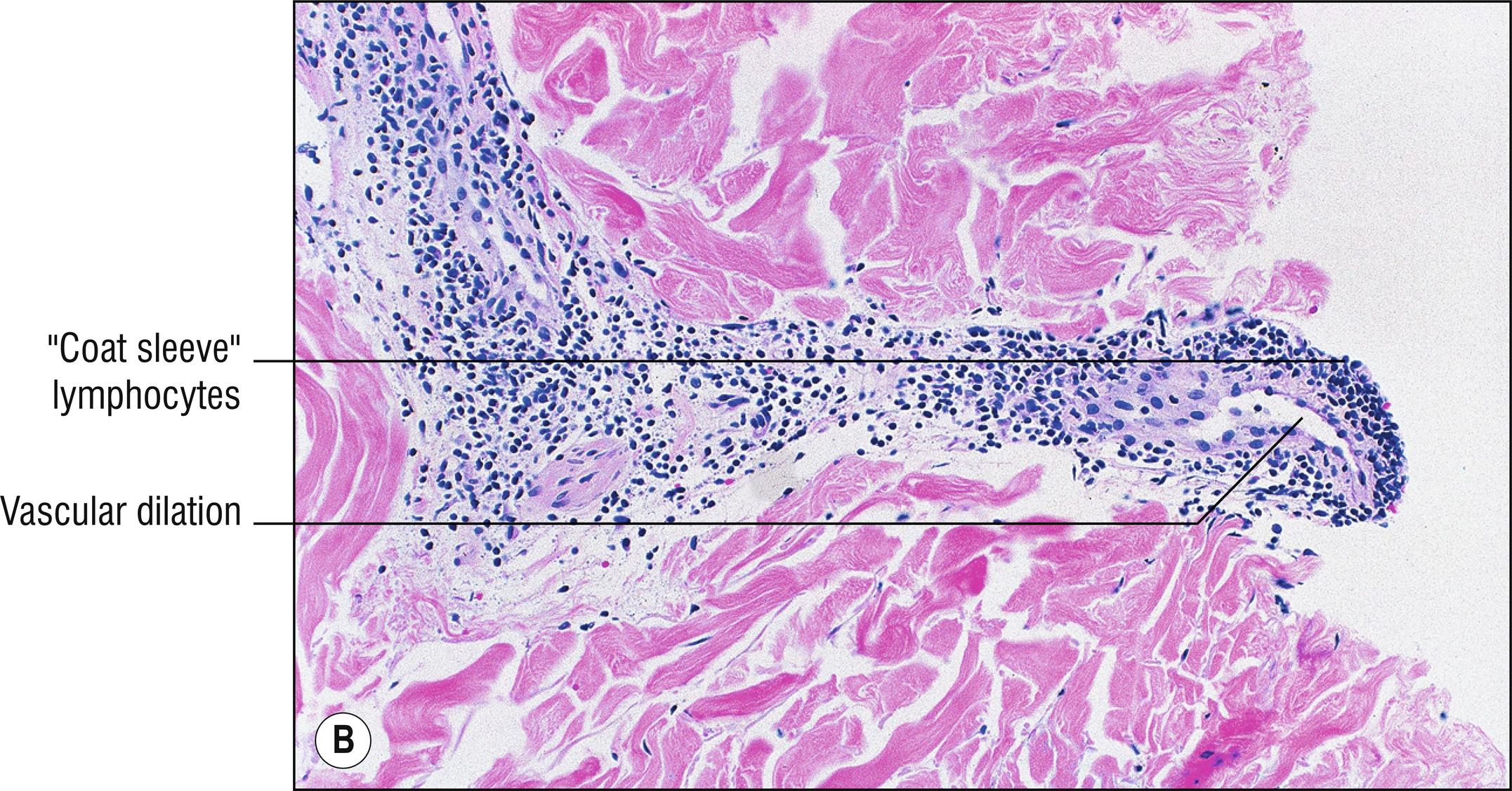
Uncommon, annular plaques (if rings are not present, then it is not EAC!), often with half-rings with a collarette of trailing scale , usually of the trunk (1.141) of adults. Usually idiopathic, sometimes a cause such as tinea pedis is found.
Occasional focal spongiosis (1.132) or parakeratosis (1.104)
Sharply demarcated “ coat-sleeve ” lymphocytes densely arranged around dilated superficial and deep blood vessels
Other annular diseases (1.5), especially gyrate erythemas.
Erythema multiforme (3.2): more necrotic keratinocytes.
Secondary syphilis (12.13): plasma cells, positive serology.
Other diseases with superficial and deep perivascular dermatitis (1.109).
Very rare, impressive wood-grain appearance of pruritic, red, scaly rash most common on trunk (1.141), changing daily, usually associated with underlying systemic malignancy (1.105), especially carcinomas, most commonly of the lung.
Mild focal spongiosis (1.132) and parakeratosis (1.104)
Perivascular lymphocytes (1.109), sometimes with eosinophils (1.36)
Diagnosis is made from characteristic clinical “wood-grain” appearance. Other annular rashes (1.5) rarely have such a striking clinical appearance. Histology is non-specific, resembling other diseases with perivascular dermatitis (1.109).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here