Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radiologic evaluation of esophageal diseases can be performed by fluoroscopic barium examination (esophagram), computed tomography (CT) scan, positron emission tomography (PET) scan, fused CT and PET images (PET/CT), and magnetic resonance imaging (MRI). These five imaging modalities constitute the radiologic options currently available for esophageal evaluation. Which test is best for the diagnosis of esophageal disease? It depends. The choice of esophageal imaging modality depends on the goal of esophageal imaging. Indeed, the choice of esophageal testing, in general, depends on the goal of the testing. When the diagnostic questions are esophageal obstruction, characterization of hiatal hernia, esophageal perforation, or achalasia, the esophagram is the best test to perform. When the diagnostic questions are gastroesophageal reflux disease (GERD), other esophagitis, mass, or motility disorder other than achalasia, the esophagram can be useful, although it is not the best test available for these entities. When the diagnostic question is the staging of esophageal tumors, esophagram is not indicated because it demonstrates the luminal margin of the esophagus only. Tumor staging questions are best answered by cross-sectional imaging modalities.
The barium esophagram remains a test of definite utility in the 21st century, along with cross-sectional imaging (CT, MRI, and PET), endoscopy, endoscopic ultrasound (EUS), high-resolution manometry, pH monitoring, and multichannel intraluminal impedance. In fact, all of these tests are complementary for the diagnosis of esophageal diseases.
In our practice over the last decade, the volume of radiographic contrast studies of the stomach, small bowel, and colon has continued to decline; however, the volume of esophagrams has increased each year. This increasing utilization of a nearly 100-year-old test by gastroenterologists and other referring physicians and surgeons indicates its continuing relevance for the evaluation of dysphagia. The utility of the esophagram is increased further when, in the appropriate clinical context of dysphagia, it is paired with a fluoroscopic video swallow. Between them, these two examinations can demonstrate the structure and function of the oropharynx, hypopharynx, cervical esophagus, and thoracic esophagus. Their relatively low cost and almost universal availability make them a logical starting point for the evaluation of dysphagia.
This chapter begins by describing the essential technical elements, normal findings, and common artifacts of the esophagram. Then, the utility of the esophagram is discussed in the settings of GERD, esophageal motility disorders, esophageal neoplasms, and the postoperative esophagus. The discussion of esophageal neoplasms includes a discussion of the role of cross-sectional imaging, especially PET/CT, for tumor staging. Subsequently, miscellaneous conditions such as hiatal hernias, esophageal rings and webs, less common types of esophageal strictures, caustic injury, and esophageal perforation, diverticula, and varices are discussed and illustrated.
An understanding of the imaging techniques of the esophagram helps the referring physician evaluate the quality of images, the completeness of the study, and the validity of the conclusions reached by the radiologist. The essential techniques of the esophagram are not complex. The performance of the radiologist performing esophagrams improves when referring physicians and surgeons provide follow-up regarding the accuracy of his or her diagnoses. Indeed, a team approach to the care of esophageal diseases not only benefits the patient; it also benefits the physicians caring for the patient. They learn from each other.
A complete esophagram is a multiphasic examination performed in upright and recumbent positions with variable consistencies of barium resulting in air-contrast, single-contrast, and mucosal relief images. Unfortunately, radiologists typically refer to this complete esophagram as an air-contrast esophagram ; nevertheless, they know that single-contrast, recumbent images are necessary, in addition to air-contrast images, to consider an esophagram complete. The images obtained during air-contrast, single-contrast, and mucosal relief phases of the examination are complementary.
The air-contrast technique is performed in the upright position, typically with the patient in the left posterior oblique position with respect to the vertical fluoroscopy table. This technique allows for detailed evaluation of the esophageal mucosa. Maximum gaseous distention of the esophagus is achieved when the patient ingests an effervescent agent that releases carbon dioxide when mixed with water. Immediately after the esophagus is distended by gas, the patient drinks high-density barium as quickly as possible in the upright position. Uniform distribution of this thick barium on the luminal surfaces of the gas-distended esophagus allows demonstration of the entire mucosa of the esophagus. Normally, the esophageal mucosa is featureless on these air-contrast images. Occasionally, tiny filling defects, representing undissolved effervescent crystals, are present on the mucosal surface ( Fig. 6.1 ). These artifactual filling defects usually change position on sequential upright images.
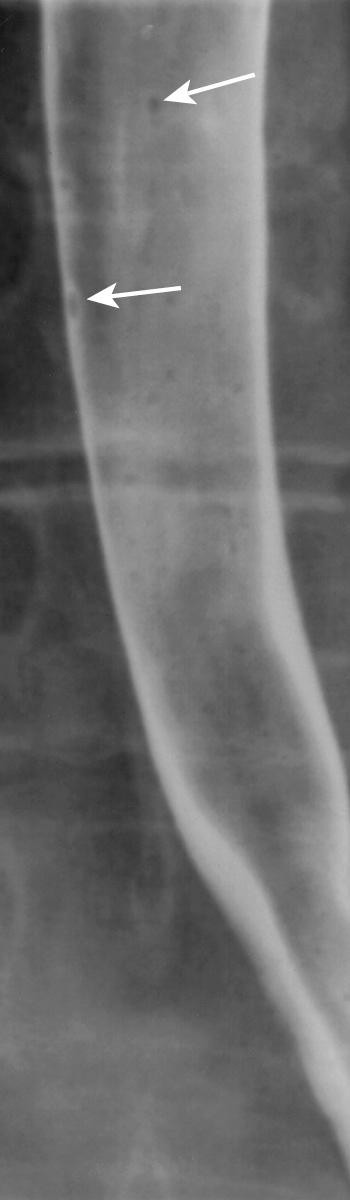
Because the esophagus remains distended by gas for only a short time in the upright position, the radiologist needs to obtain air-contrast images quickly. As the esophageal lumen collapses, residual barium is trapped between redundant longitudinal mucosal folds of the esophagus, resulting in a mucosal relief image of the esophagus. These longitudinal folds should appear as smooth and linear structures less than 3 mm thick on mucosal relief images ( Fig. 6.2 ). Mild thickening and irregularity of the distal longitudinal folds may be a subtle sign of reflux esophagitis.
Before tilting the table into the horizontal position, the radiologist should determine the need for upright evaluation of swallowing and the cervical esophagus. Anatomically, the two main sites of abnormalities resulting in dysphagia are the oropharynx and the esophagus. When patients report food sticking, and point to the neck or thoracic inlet as the level of obstruction, their symptoms may result from oropharyngeal dysphagia or esophageal dysphagia. However, when patients report food sticking, and point to the substernal region as the level of obstruction, their symptoms typically result from an esophageal dysphagia. Therefore, referring physicians and surgeons, as well as radiologists, should ask the patient two questions: (1) Does food stick? (2) Where does it stick?
When the patient indicates that food sticks at the level of the neck or thoracic inlet, the oropharynx and cervical esophagus should be evaluated in the upright position. For example, the radiologist puts the patient in the upright lateral position and observes a swallow fluoroscopically. Structural causes of oropharyngeal dysphagia such as cricopharyngeal bar, cervical esophageal stricture, or cervical esophageal web are readily identified in the lateral position. When a neuromuscular cause of dysphagia is suggested by this single upright view, it is best evaluated by a speech pathologist trained in the evaluation of dysphagia. The speech pathologist interviews and examines the patient before performing a video swallow study with multiple consistencies of barium. In fact, we often perform the video swallow, in consultation with speech pathologist, and the esophagram during a single patient visit to the fluoroscopy suite. This patient convenience is facilitated by our referring physicians and surgeons, who are aware of the variable etiology of so-called high dysphagia (when the patient indicates that food sticks at the level of neck or thoracic inlet). Consequently, they can order both the video swallow study and the esophagram initially, or they can give us permission to evaluate the esophagus as necessary based on the result of the video swallow. A motion-recording device that captures 30 frames per second is very helpful for the evaluation of swallowing. This type of continuous recording captures the dynamic events of swallowing far better than rapid sequential radiographic images captured at 4 to 8 frames per second.
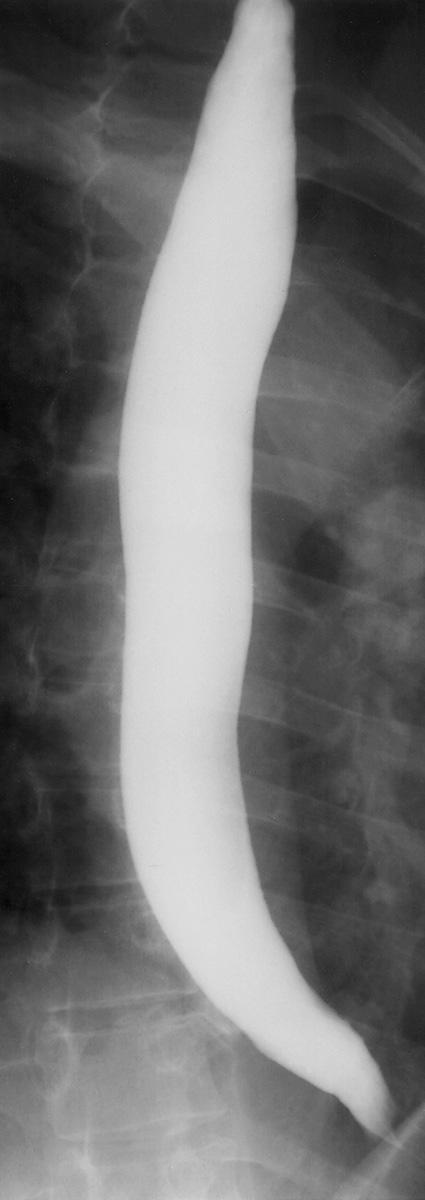
The single-contrast phase of esophagram is performed in the prone, right anterior, oblique position with respect to the horizontal fluoroscopy table. Patients drink as rapidly as possible in this position to produce maximal esophageal distention. Fixed segments of subtle esophageal narrowing become apparent only during maximal esophageal distention. If the patient cannot drink barium rapidly enough to sufficiently distend the lumen, areas of segmental narrowing are likely to go undetected.
When fully distended, the margins of the esophagus should be smooth on these single-contrast images ( Fig. 6.3 ). Normal extrinsic impressions occur at the level of the transverse aorta and the left main stem bronchus ( Fig. 6.4 ). Extrinsic impressions occurring elsewhere should be viewed with suspicion.
Esophageal motility should be tested by single swallows of barium with patient in the prone, right anterior, oblique position. In this position, gravity does not contribute to esophageal emptying. To prevent esophageal peristaltic inhibition, patients are asked not to swallow between swallows. In addition, the time between swallows should be at least 20 seconds. The primary peristaltic wave initiated by swallowing should propagate through the entire esophagus and result in bolus passage into the stomach. The trailing edge of the peristaltic wave resembles an inverted V , as sequential muscular contractions obliterate the esophageal lumen from proximal to distal. Frequently, a small amount of barium remains in the middle third of the esophagus after passage of the primary peristaltic wave. This small residual volume of barium should not be interpreted as abnormal motility since this esophageal segment is normally the zone of lowest normal contractile amplitude. Completion of the peristaltic contraction is accompanied by relaxation of the lower esophageal sphincter (LES) as the bolus passes into the stomach.
In normal patients, 95% of swallows are accompanied by normal esophageal peristalsis. The incidence of failed and low-amplitude peristaltic contractions probably increases with age. This increased incidence with age may represent normal aging or subclinical disease. Therefore, abnormal peristaltic function, especially nonpropulsive (tertiary) contractions, should be interpreted with caution in older individuals.
As the esophagram comes to an end, we return the fluoroscopy table and the patient to the upright position. When patients complain of difficulty swallowing pills, or we are suspicious of an esophageal stricture based on prone, single-contrast images, we ask them if they are willing to swallow a 12.5-mm barium tablet with 60 mL of water in the upright position. In normal subjects, the tablet should pass into the stomach within 60 seconds. One-half or one-third of a marshmallow, swallowed with thin barium in upright position, may hang up at areas of narrowing not otherwise visible during routine examination. Single bites of other foods, such as bread, may also be used to assess the functional severity of a stricture. None of these items should be administered by the radiologist to a patient at risk of aspiration. In addition, patients have the right to refuse to swallow a tablet or other food bolus. Many patients, especially those with oropharyngeal causes of dysphagia, are frightened of choking on the pill or food bolus.
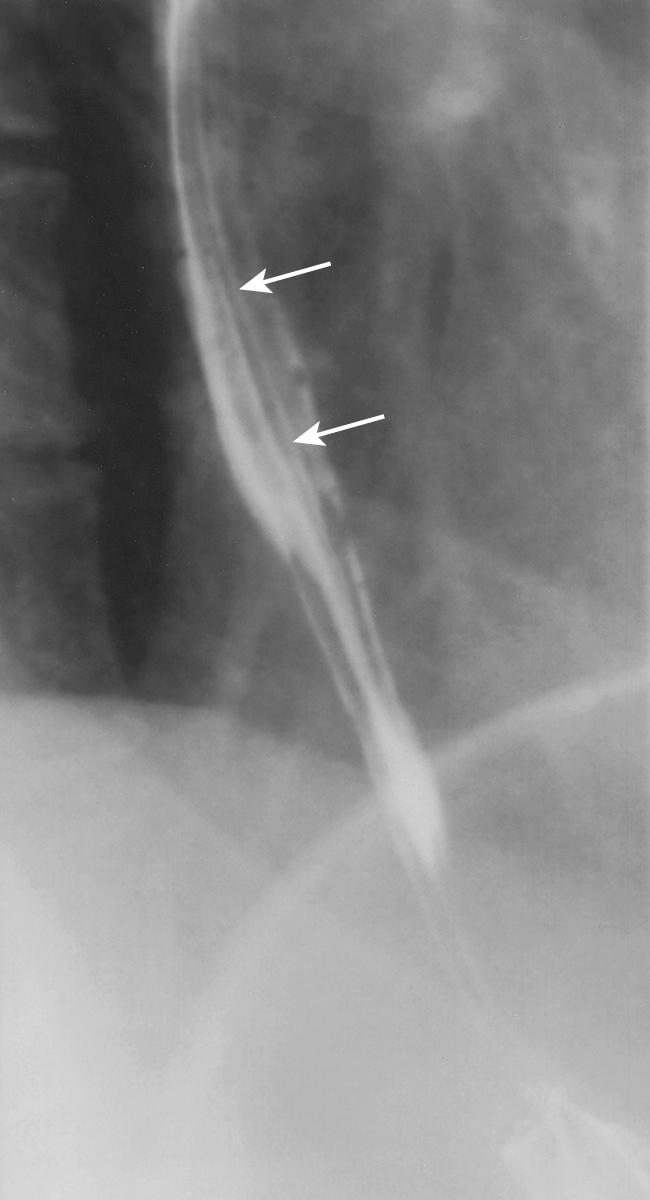
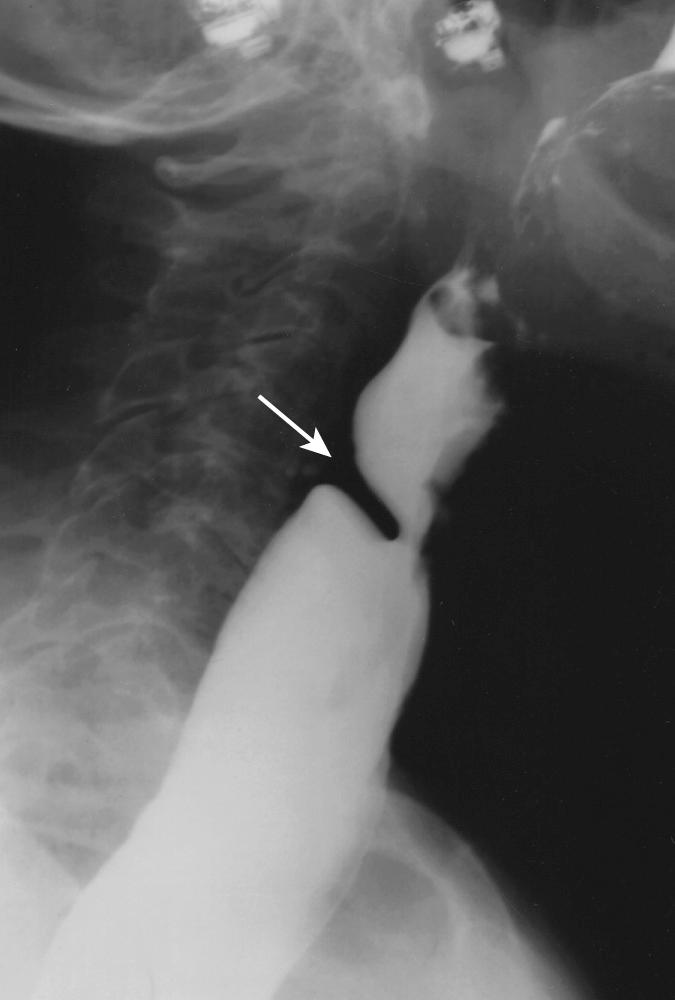
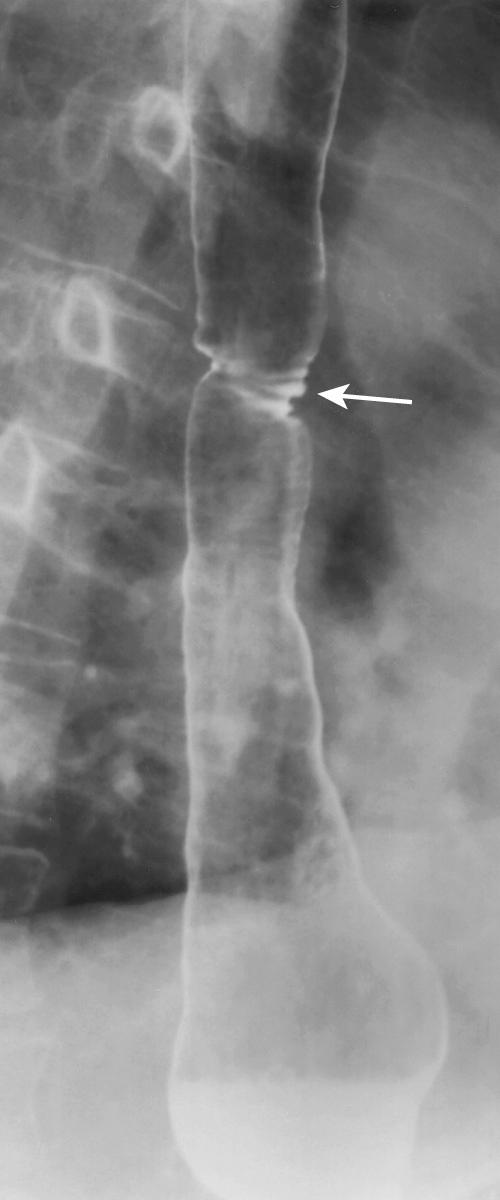
With the patient in the upright position again, the radiologist has one more chance to evaluate swallowing in the cervical esophagus in the lateral position. This evaluation is especially relevant in patients who report food sticking in region of neck or thoracic inlet. The likelihood of an oropharyngeal cause of dysphagia in these patients is more likely than it is in those patients who report food sticking in the substernal region. This upright lateral view may suggest neuromuscular causes of dysphagia, best evaluated by speech pathologists. The abnormality revealed most commonly by these lateral images is a cricopharyngeal bar at the pharyngoesophageal junction. This failure of the cricopharyngeus muscle to relax occasionally accompanies more distal disease and may contribute to the dysphagia symptoms ( Fig. 6.5 ). Cervical esophageal webs, rings, and strictures can also be demonstrated by this lateral view.
A brief examination of the stomach contributes to the evaluation of patients complaining of dysphagia. Neoplasms of the gastric cardia can present with dysphagia, and may be overlooked if the stomach is not evaluated. In patients with GERD, gastric dysfunction may be an important contributory factor, so evidence of delayed gastric emptying should be noted.
The normal esophageal ampulla (vestibule) is sometimes confused with a hiatal hernia. It appears as a smoothly marginated, mildly dilated segment of the esophagus just superior to the esophageal hiatus ( Fig. 6.6 ). Unlike a hiatal hernia, the ampulla does not contain gastric folds and will demonstrate typical esophageal peristalsis. The transient appearance of fine, evenly spaced, transverse folds is called “feline esophagus” ( Fig. 6.7 ). This condition has been reported to be more frequent in patients with GERD, but is also demonstrated in asymptomatic patients. It is thought to result from contraction of the longitudinal muscle layer of the esophagus, usually in response to gastroesophageal reflux (GER).

One of the earliest reports of abnormal reflux of gastric contents into the esophagus was based on observations made during GI contrast studies. Today the esophagram remains useful in evaluating GERD patients, especially those considering surgical intervention.
The cause of GERD is multifactorial. The most common etiologic factor is abnormality of the LES leading to loss of the normal antireflux barrier. Contributory factors include the volume and composition of the gastric refluxate, altered esophageal mucosal resistance, and the effectiveness of esophageal clearance. Although other tests are more accurate in quantifying these etiologic factors, the esophagram may provide clues that point to the need for further evaluation. For example, the demonstration of a hiatal hernia by esophagram suggests alteration of the normal antireflux barrier that can be confirmed with LES manometry. Radiographic signs of abnormal esophageal motility suggest poor esophageal clearance of any refluxed material that can be evaluated with esophageal manometry.
The classic symptoms of GERD—namely, heartburn and regurgitation—are nonspecific and may accompany a variety of esophageal diseases, including motility disorders. About 10% of patients with motility disorders present with symptoms suggestive of GERD—namely, heartburn and regurgitation. Furthermore, dysphagia and chest pain, more typical symptoms of motility disorders, may be absent in these patients. Symptoms of heartburn are even more common in achalasia, occurring in 40% of patients. In patients with classic achalasia, the esophagram is usually characteristic, confirming the diagnosis. In patients complaining of heartburn, the correct diagnosis of achalasia prevents a potential catastrophe resulting from inappropriate antireflux surgery.
Ambulatory pH monitoring is the gold standard for the diagnosis of GER. A pH of 4 or less during greater than 5% of the 24-hour monitoring period constitutes a positive test. A few studies have correlated pH results with radiographic detection of GER. One study demonstrated relatively good correlation, showing a radiographic sensitivity of 70% and specificity of 74%, with both spontaneous reflux and the water siphon test. A subsequent study failed to confirm this correlation and concluded that barium radiography lacks sufficient sensitivity and specificity to be used as a screening procedure for GERD. In general, the response to trials of proton pump inhibitors in patients with typical symptoms of heartburn and regurgitation are more predictive of pH test results than the presence of radiologically detectable GER.
Small volumes of barium transiently refluxing into the distal esophagus are probably not significant. However, repeated episodes of reflux into the upper esophagus, particularly in the presence of a large hiatal hernia, are often predictive of a high pH score.
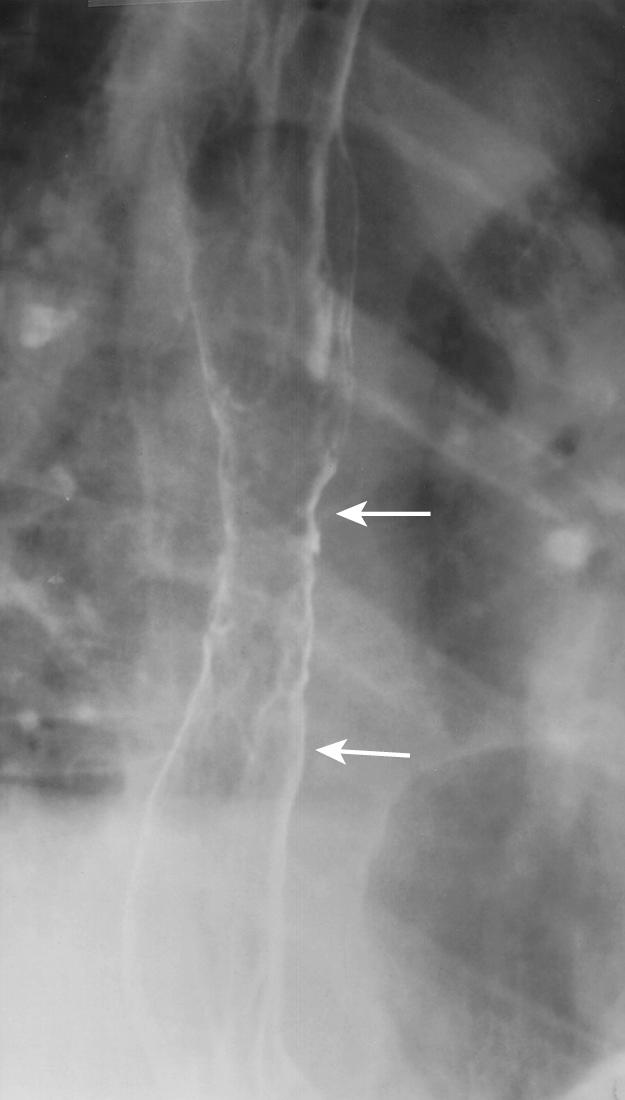
Esophageal injury is manifested by acute inflammation, scarring, stricture, Barrett metaplasia, and alterations in esophageal motility. Radiographic detection of acute esophagitis depends on the severity of the disease. Mild to moderate degrees of inflammation are frequently not demonstrated radiographically. Signs of acute esophagitis include thickening and irregularity of the distal esophageal folds, best demonstrated by mucosal relief images ( Fig. 6.8 ). Less frequently, mucosal nodularity and erosions are visible on air-contrast images.
Esophageal scars and strictures secondary to GERD are generally visible radiographically. The appearance of these scars and strictures can be typical enough to exclude malignancy. Reflux strictures usually occur at the gastroesophageal junction (GEJ); they may be smoothly tapered or irregular ( Fig. 6.9 ). When compared with a mucosal ring (Schatzki ring), strictures are generally more eccentric and thicker. When an otherwise typical-appearing reflux stricture occurs well above the GEJ, it suggests the possibility of Barrett metaplasia between the GEJ and the stricture ( Fig. 6.10 ).
Single-contrast evaluation of the esophagus in the prone position is superior to endoscopy for detecting areas of segmental esophageal narrowing, especially larger-diameter strictures and those that taper gradually. These strictures may only be demonstrated when the esophagus is maximally dilated by rapidly ingested barium. They may not be appreciated endoscopically, particularly with smaller-diameter endoscopes. Many esophageal strictures and rings may be missed if the esophagus is examined only in the upright position.
Initial reports suggested high sensitivity of air-contrast esophagrams for the detection of columnar epithelium in Barrett esophagus. The findings were described as a reticular mucosal pattern ( Fig. 6.11 ). However, other investigators found this radiographic feature to be present in only 23% of cases. The findings of hiatal hernia, GER, and esophageal stricture are better clues to the presence of Barrett metaplasia than the reticular mucosal pattern described initially. In addition, a midesophageal stricture suggests Barrett metaplasia between the stricture and the GEJ (see Fig. 6.10 ).
Abnormal motility causing poor clearance of refluxed material promotes esophageal damage by prolonging exposure of the mucosa to the noxious effects of the refluxate. Studies have shown relatively good correlation between the results of synchronous manometry and fluoroscopic observation of the barium bolus progressing through the esophagus, suggesting that barium examination may provide accurate estimates of esophageal motility. Therefore evidence of poor esophageal motility radiographically may help identify patients who will be resistant to conventional-dose proton pump inhibitor therapy. This information is also helpful in selection of the appropriate surgical approach and type of antireflux repair.
The presence of a large hiatal hernia (>5 cm) or evidence of a shortened esophagus can influence the type of surgical repair and operative approach during surgery for GERD. In fact, failure to recognize these conditions may lead to surgical failure as a result of an inappropriate surgical approach or type of repair. The size of a hiatal hernia is best estimated during a barium study. Hernia size is determined by measuring the distance from the GEJ to the esophageal hiatus during maximum filling of the hernia in the prone position. Hernia size can be underestimated by endoscopy, perhaps because of partial reduction of the hernia during passage of the endoscope.
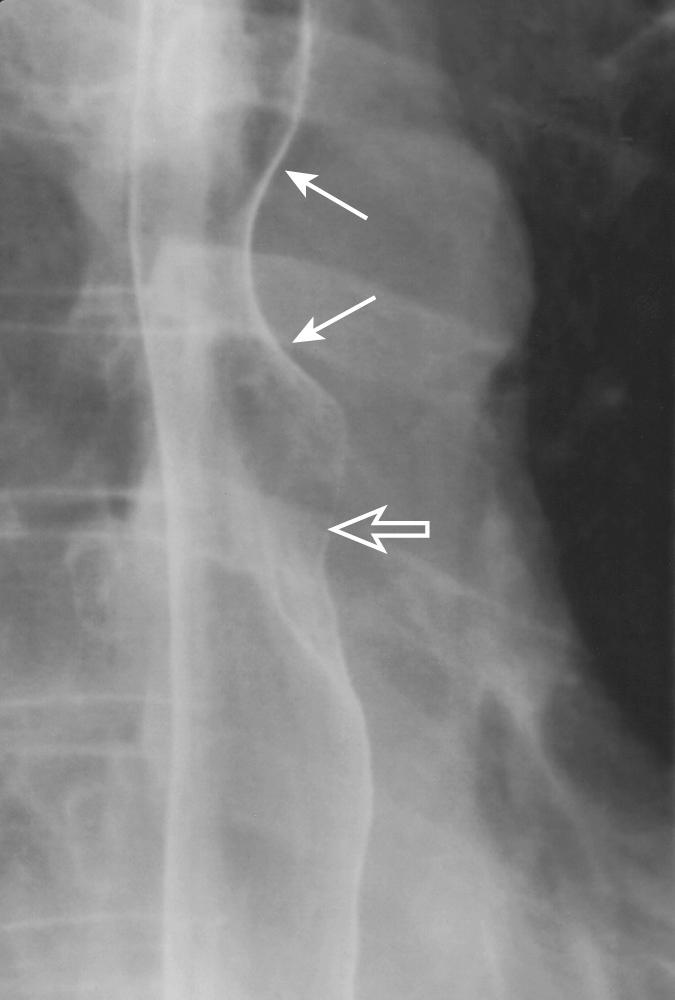
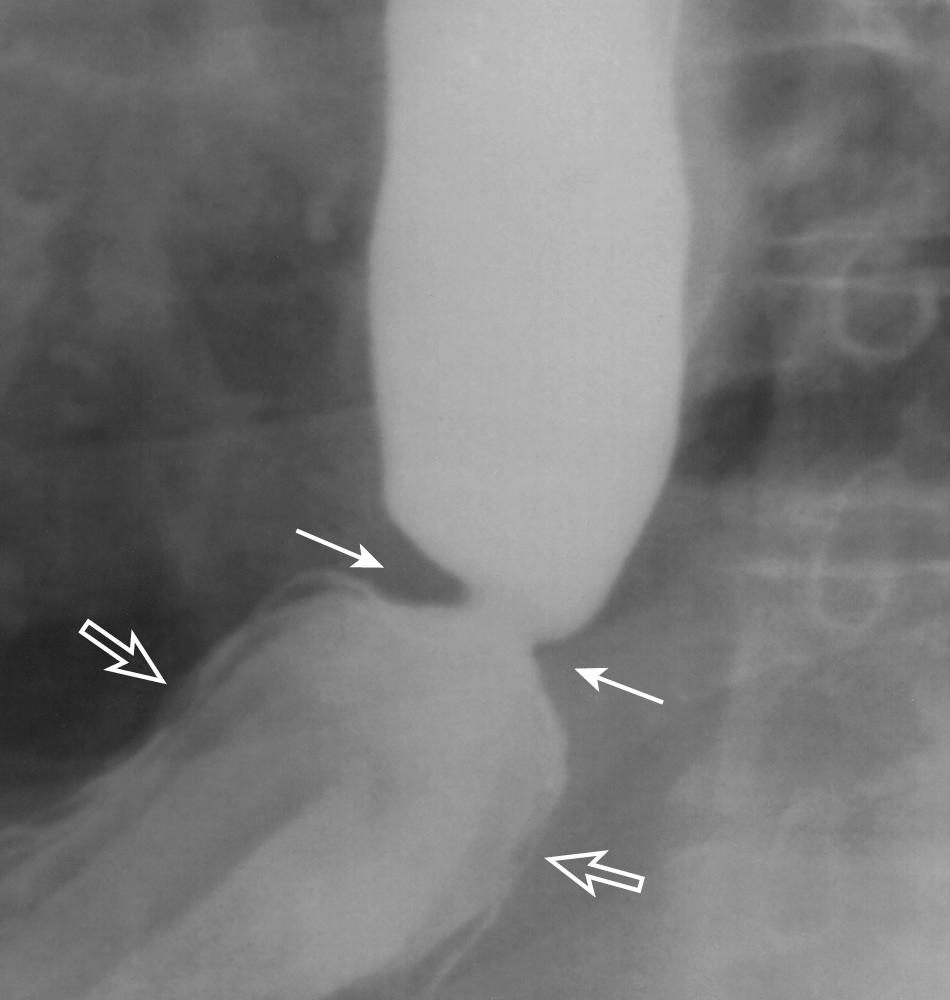
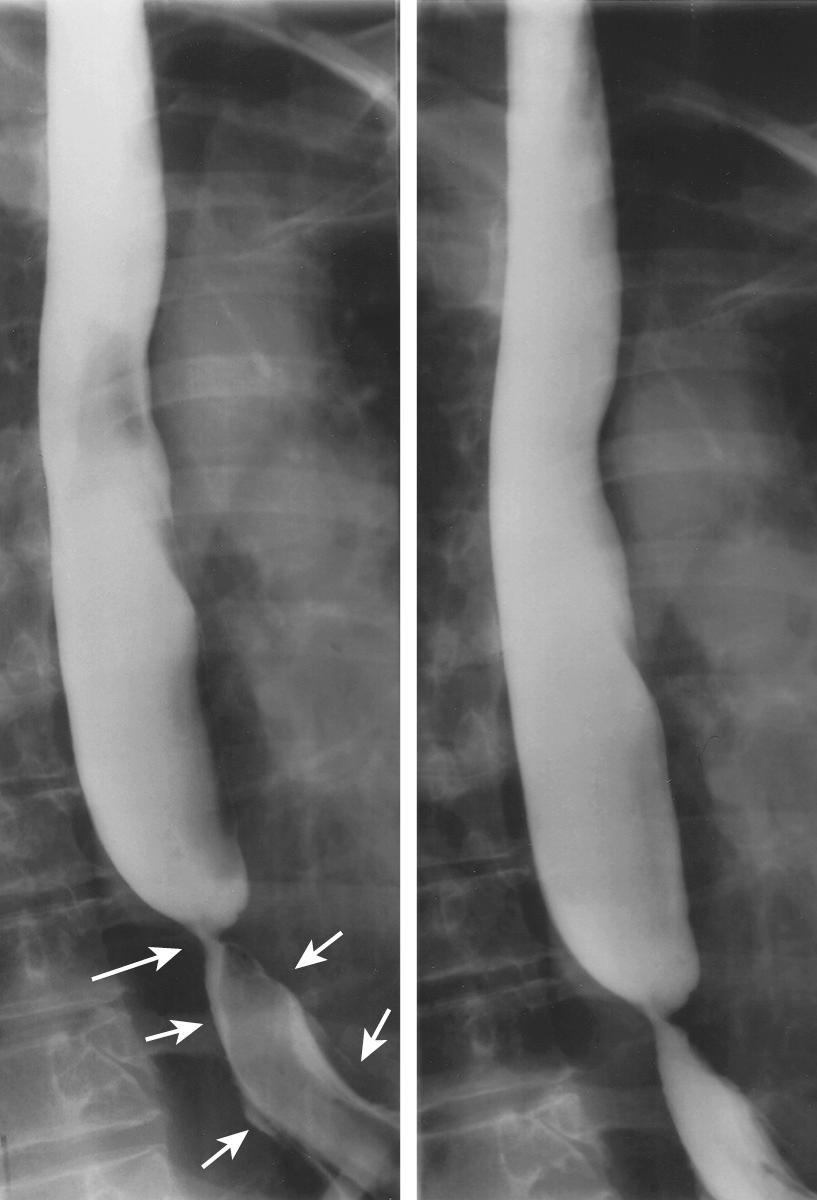
Esophageal shortening is the result of longitudinal scarring, often caused by severe GERD. In such cases, inadequate surgical dissection during laparoscopic fundoplication may leave the repair under tension and lead to early surgical failure. Clues to the diagnosis of esophageal shortening include esophageal scarring, stricture, and the size and shape of the hiatal hernia. A hiatal hernia with tapered, rather than bulging, shoulders suggests shortening ( Fig. 6.12 ).
Conditions associated with abnormal esophageal motor function are classified as motility disorders. Established manometric criteria exist for all of the motility disorders. The diagnosis of a motility disorder is based on a combination of manometric and clinical findings. Esophagram may suggest dysmotility and help referring physicians and surgeons select patients who would benefit from further evaluation by manometry.
The efficacy of the esophagram for detection of esophageal dysmotility is dependent on the type of motility disorder. Although the examination is very sensitive for the detection of achalasia (95%), it is less sensitive for diffuse esophageal spasm (DES; 71%) and nonspecific esophageal motility disorder (NEMD; 46%). In a group of patients with dysphagia, the overall sensitivity of esophagram for the detection of a motility disorder was 56%. The sensitivity increased to 89% when patients with nutcracker esophagus and NEMD were excluded.
Symptoms of dysmotility are nonspecific and include dysphagia, regurgitation, chest pain, and heartburn. Dysphagia to both liquids and solids is more common in motility disorders. When present, regurgitation is usually described as bland rather than acidic, as a result of its origin from the esophagus rather than the stomach. Chest pain varies from intermittent and sharp to constant and pressure-like. It may mimic pain of cardiac origin. The presence of dysphagia increased the likelihood of an esophageal, rather than cardiac, cause of chest pain. Heartburn is a common complaint, especially in patients with achalasia. The nonspecificity of the symptoms of motility disorders, especially their overlap with symptoms of GERD, makes additional diagnostic studies necessary to clarify the nature of the disease.
Motility disorders are classified as either primary or secondary. This distinction is based on whether the esophagus is primarily involved or whether the esophageal involvement is part of a systemic process.
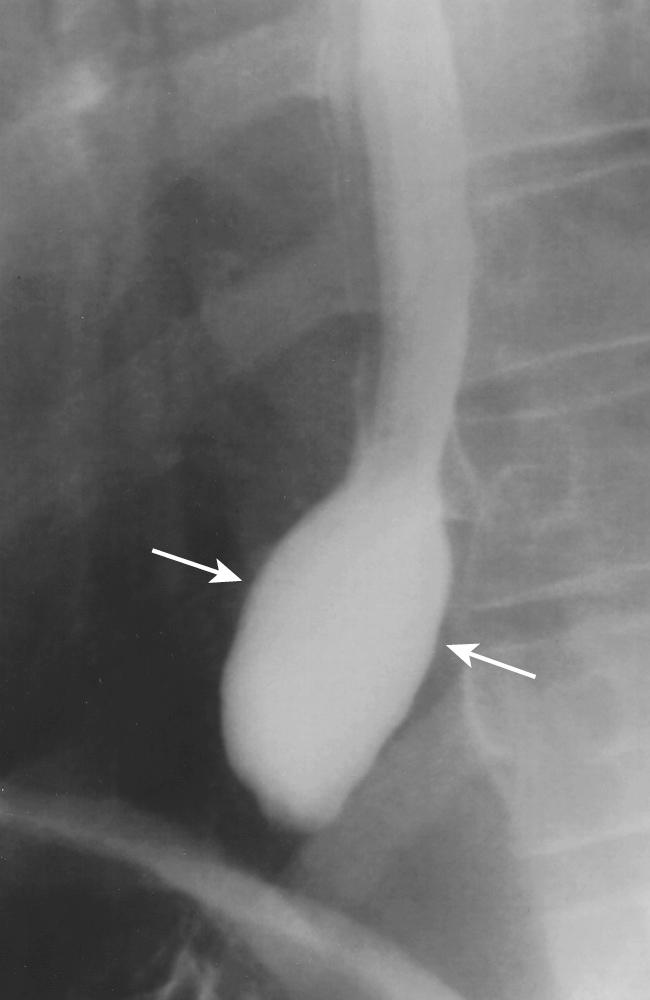
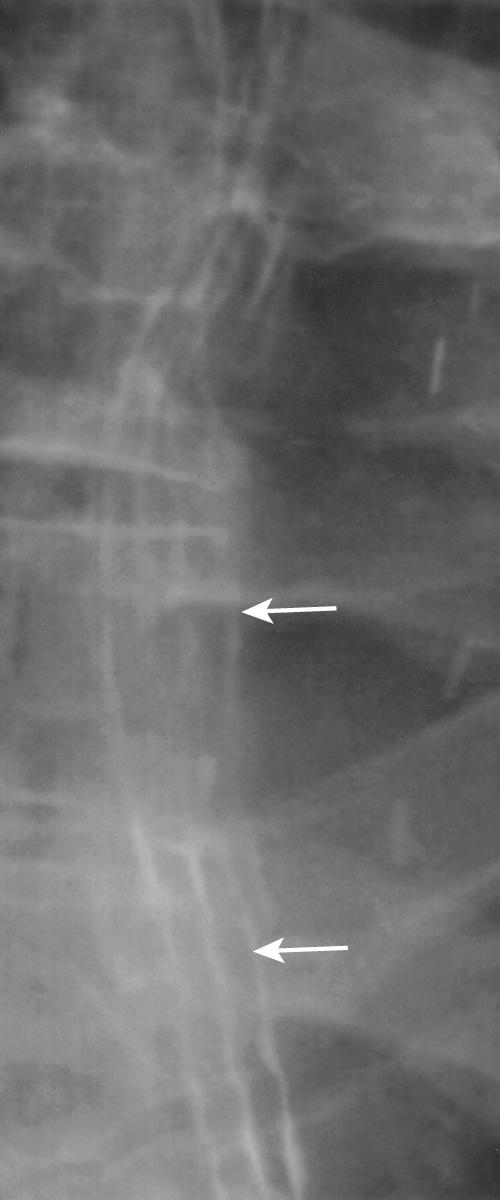
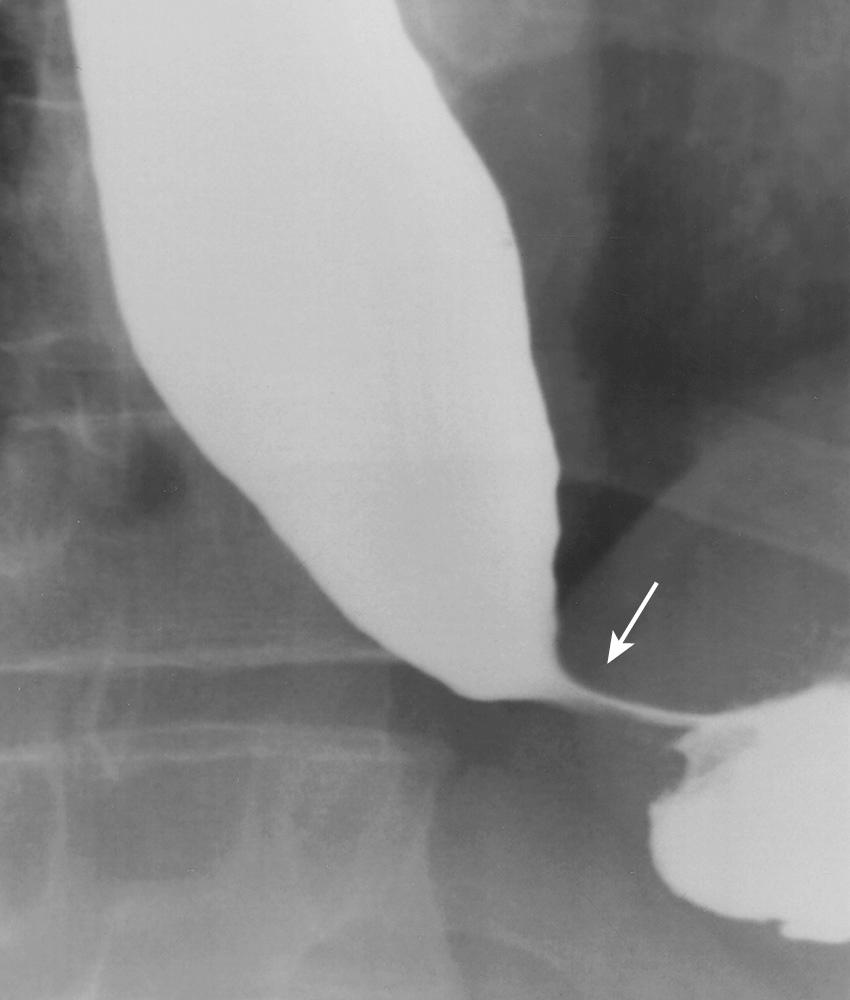
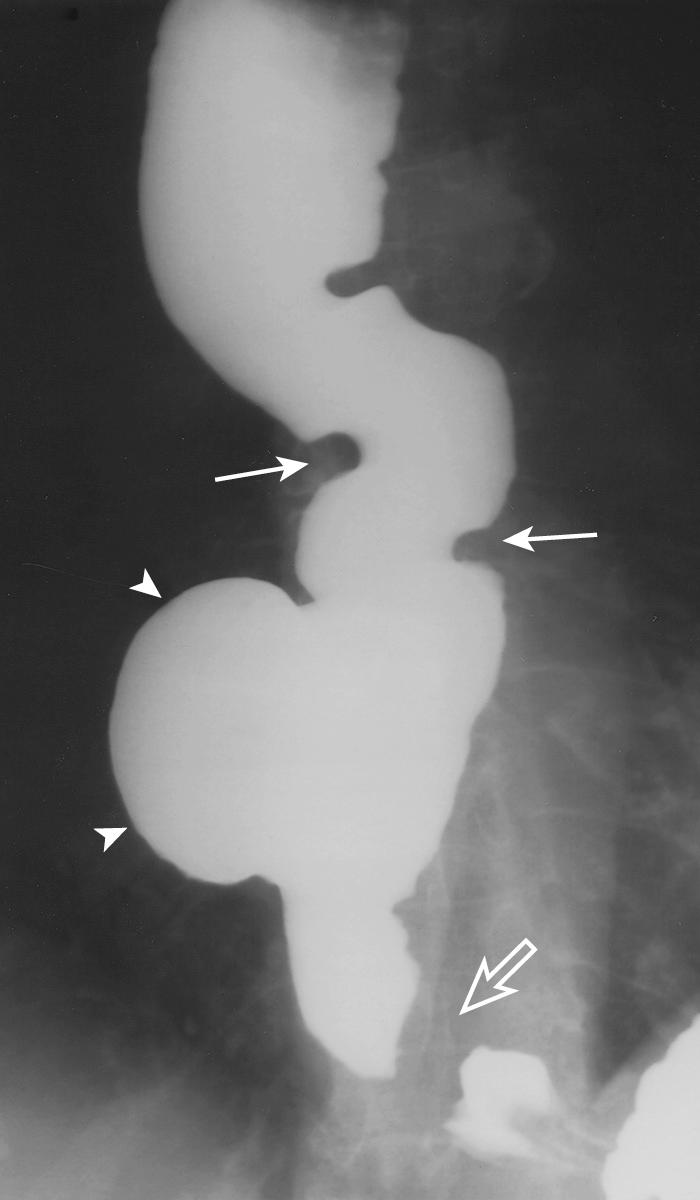
Achalasia is characterized manometrically by absent peristalsis in the distal two-thirds of the esophagus and abnormally high LES resting pressure. In classic achalasia, the esophagus is markedly dilated. As the patient drinks in the upright position, the barium column is usually distorted by retained food and fluid within the dilated lumen. Nevertheless, the lower end of the barium column is typically tapered to a point, resembling a bird's beak ( Fig. 6.13 ). A barium-fluid level results when barium, which is denser than water, accumulates inferior to the retained secretions in the esophagus. The height of this barium-fluid level is usually characteristic for each patient—the more severe the obstruction, the higher the level. With severe achalasia, the esophagus becomes redundant and the distal esophagus assumes a sigmoid configuration ( Fig. 6.14 ). The configuration contributes another cause of poor esophageal emptying to the absent peristalsis and LES relaxation failure of less severe achalasia.

Vigorous achalasia is a variant of classic achalasia in which prominent tertiary contractions of the distal two-thirds of the esophagus accompany the esophageal dilatation and tapered narrowing of the GEJ ( Fig. 6.15 ) of classic achalasia.
Pseudoachalasia results from mural infiltration by malignancies at the GEJ. The esophageal findings mimic classic achalasia. In many cases, no intraluminal mass is demonstrated by esophagram or by endoscopy. In these cases, the diagnosis is often suspected because of the older age of the patient and the rapid onset of dysphagia. One paper suggests that the length of the “bird's beak” is greater in patients with pseudoachalasia than in those with classic achalasia. When pseudoachalasia is suspected, CT of the chest and abdomen with intravenous contrast material sometimes demonstrates the infiltrative intramural mass.
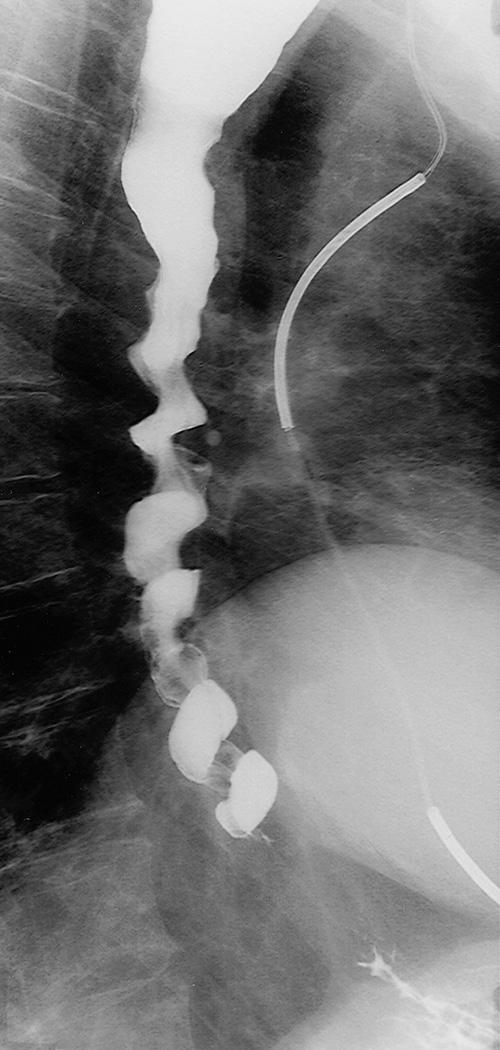
DES is a disorder of unknown cause characterized by intermittently abnormal motility associated with symptoms of chest pain and dysphagia. The dysphagia is variably present and does not necessarily accompany the chest pain. Manometrically, simultaneous contractions occur in greater than 10% of wet swallows. Radiographic features reflect the manometric findings; peristalsis is intermittently replaced by tertiary contractions, producing a “corkscrew” appearance of the esophagus ( Fig. 6.16 ). Normal peristalsis is usually present in the proximal esophagus. One report has suggested that delayed esophageal emptying, secondary to abnormalities of the LES, may be a more common esophagraphic finding in DES than a corkscrew appearance of the esophagus.
Radiographic sensitivity in the diagnosis of DES is low in comparison to its sensitivity in the diagnosis of achalasia. Tertiary contractions are common in both normal patients and those with motility disorders, and should not be interpreted as indicative of DES unless confirmed by manometry. Thickening of the distal esophageal wall by thoracic CT scans has been reported in 21% of patients with DES. The thickness of the esophageal wall by CT in normal subjects should not exceed 5.5 mm. Therefore DES should be considered in the differential diagnosis of concentric distal esophageal wall thickening by CT, along with infectious, inflammatory, and neoplastic causes.
NEMD is a “waste basket” category used that includes motility disorders that do not meet established manometric criteria for other motility disorders. Manometric abnormalities include failed peristalsis, low-amplitude contractions, prolonged duration of peristalsis, simultaneous contractions, tertiary contractions, and incomplete relaxation of the LES. Symptoms are nonspecific and include chest pain and dysphagia. Radiographic findings are frequently normal. When present, radiographic findings are nonspecific, and include ineffective peristalsis and tertiary contractions causing stasis of esophageal barium.
Recently, a subgroup of patients with NEMD defined manometric criteria demonstrating hypocontraction of the distal esophagus. GERD is common in these patients. However, radiographic findings in these patients are nonspecific, and are similar to those of other patients with NEMD.
Secondary motility disorders are systemic disorders that secondarily affect the esophagus. With few exceptions, the radiographic appearance is nonspecific. Of the collagen vascular diseases, scleroderma most often involves the esophagus. The pathologic changes of scleroderma result in hypomotility of the distal esophagus and a hypotensive LES. The combination of these two motor abnormalities sets the stage for severe GERD, secondary to recumbent GER and poor acid clearance.
The radiographic changes of scleroderma include poor distal esophageal peristalsis, stasis, and esophageal injury secondary to GERD. Eventually, the severe GERD caused by esophageal scleroderma results in distal esophageal scarring, an esophageal shortening resulting in proximal dilatation, distal stricture, and hiatal hernia with tapered, rather than shouldered, margins (see Fig. 6.12 ). When esophageal scleroderma reaches this advanced stage, it can be difficult to distinguish from achalasia because of the similar radiographic findings of poor esophageal peristalsis, distal stenosis, and proximal dilatation.
Chagas disease is caused by the tropical protozoan Trypanosoma cruzi . It is endemic to South and Central America. Cardiac muscle and smooth muscle of the gastrointestinal tract are commonly involved. The radiographic appearance of esophageal Chagas disease is identical to classic achalasia.
Patients with malignant esophageal neoplasms usually present with dysphagia. Conversely, benign esophageal tumors tend to be incidental radiographic or endoscopic findings. However, when these tumors are symptomatic, excision is usually curative. CT can occasionally suggest the diagnosis of esophageal neoplasm, but it is more useful in staging esophageal malignancies, along with more specific modalities such as PET and EUS.
The symptoms causing patients with esophageal malignancy to seek medical care are typically dysphagia of recent onset (1 to 4 months) and weight loss. The prognosis for symptomatic patients is dismal. Historically, more than 95% of esophageal cancers have been squamous cell carcinomas. However, in recent decades, the incidence of esophageal adenocarcinoma has increased dramatically. Radiographically, these two types of carcinoma are indistinguishable. However, adenocarcinoma predominantly occurs in the distal esophagus within regions of the Barrett esophagus. Squamous cell carcinoma, by comparison, tends to occur in the upper two-thirds of the esophagus. Other primary malignancies of the esophagus, such as sarcomas, gastrointestinal stromal tumors (GISTs), melanoma, and lymphoma, are rare.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here