Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Diagnostic and interventional radiological procedures have an important role in liver transplantation. They are used before operation in the selection and presurgical management of candidates and posttransplantation in the follow-up, diagnosis, and treatment of complications.
Radiological evaluation of the liver transplant patient is usually performed on an outpatient basis. The goal is to determine abnormalities that preclude transplantation along with abnormalities that will affect the operative procedure. Real-time ultrasonography is used routinely to evaluate the liver, the biliary system, and the portal system. Ultrasonography has been found to have a sensitivity rate of 80% to 100% in detecting bile duct obstruction. It is also used to evaluate hepatic echo texture. Focal or diffuse heterogeneity may be seen in cases of fatty infiltration, cirrhosis, or tumor. In addition, ultrasonography is used to exclude occult hepatic carcinoma and to detect adenopathy in the porta hepatis, ascites, or vascular invasion by tumor. Doppler ultrasonography is used to assess the portal vasculature. The patency and size of the extrahepatic portal vein must be ascertained and the patency of the inferior vena cava (IVC) determined, because narrowing or occlusion of either of these vessels alters surgical technique. The hepatic artery and hepatic veins are also evaluated. Patients with thrombosis of the hepatic veins in the Budd-Chiari syndrome may have thrombosis of the IVC and patency of the suprahepatic IVC, which is necessary for liver transplantation to be performed. The extrahepatic portal vein may be absent in patients with biliary atresia, and the IVC may be absent in polysplenia syndrome. If the portal vessels are clearly identified, ultrasonography alone is sufficient. However, nonvisualization or equivocal visualization of the portal vein owing to thrombosis of the portal vein with cavernous transformation and large collateral vessels requires arteriography or magnetic resonance angiography (MRA) for accurate assessment.
A computed tomographic (CT) scan of the chest, abdomen, and pelvis is indicated for all patients being evaluated for liver transplantation because of a hepatic tumor. The size, number, and location of intrahepatic masses can be seen on a CT scan. In addition, a CT scan provides information regarding splenomegaly, varices, ascites, vascular anomalies, and morphological pancreatic anomalies. It also allows evaluation of the entire abdomen for primary tumors, metastases, and abscesses. The preoperative CT scans provide information regarding liver size and shape from which liver volume can be calculated, facilitating the selection of a donor liver of appropriate size.
CT scans are used initially to determine whether a patient with a hepatic tumor is a candidate for partial hepatic resection or requires transplantation.
Most cases of liver cancer occur in the presence of end-stage cirrhosis, which distorts the hepatic parenchyma and may produce focal abnormalities and nodules.
The differentiation of focal liver lesions such as hepatocellular carcinoma (HCC) on CT is based on the attenuation differences in density between normal liver and the lesion. HCCs receive most of their blood supply from the hepatic artery, whereas normal liver parenchyma is supplied mainly through the portal vein. On CT, lesions with arterial-dominant vascularity show brisk enhancement during the arterial phase (20 to 40 seconds after contrast injection) and are better detected in the background of normal liver parenchyma, which remains relatively hypovascular during this phase. During the portal phase (60 to 90 seconds after the actual injection), the liver still receives opacified blood from the arterial system and also receives four times more blood from the portal system. During this phase, hypervascular lesions such as HCC can be isodense relative to normal liver because both enhance similarly.
With older nonhelical CT units, contrast images were acquired during the portal dominant phase. In this phase, hypovascular lesions are well seen, but hypervascular lesions were usually missed because they can be isodense relative to the liver parenchyma. The development of faster helical scanners permitted biphasic imaging, with completion of the liver examination, during the arterial-dominant and portal-dominant phases of contrast enhancement. Multirow helical scanners now allow a triple-pass CT scan during early arterial, late arterial, and portal venous phases. Studies show that a significant number of additional HCC lesions can be found during the arterial phase compared with the portal or delayed phases.
Currently the recommended CT protocol is a triple-phase CT with an arterial phase, a portal phase, and an equilibrium phase (10 to 15 minutes) following injection, when most HCC becomes hypovascular relative to the liver parenchyma. Generally HCCs show brisk hyperenhancement during the arterial phase and rapidly become isoattenuating or hypoattenuating during the portal phase. In a small number of cases, however, HCC lesions may be hypoenhancing and nearly isodense in the arterial phase and persist as hypoattenuating lesions during the portal phase.
In patients with hepatic cirrhosis an enhancement pattern consisting of hyperattenuation in the arterial phase and hypoisodensity in the portal phase is virtually diagnostic of HCC ( Fig. 35-1 ).
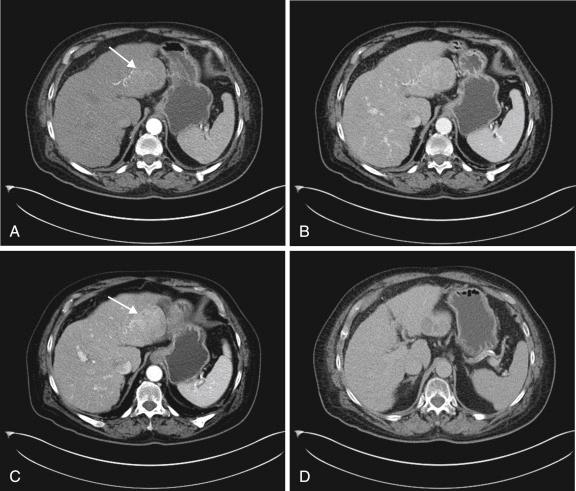
Other features characteristic for HCC are the presence of a prominent fibrous capsule on contrast-enhanced images, focal macroscopic adipose tissue within the tumor, and coexistence of a liver mass and portal vein thrombosis. Although the majority of nodules in the setting of chronic liver disease are HCC, other lesions may be detected in cirrhotic patients undergoing screening with helical CT. Hyperenhancing lesions in the arterial phase include small hemangiomas, transient hepatic attenuation differences, atypical dysplastic nodules, focal nodular hyperplasia, liver cell adenoma, and hypervascular metastases. In chronic liver disease the differential diagnosis of HCC consists largely of hemangioma, transient hepatic attenuation differences, and the rare hypervascular dysplastic nodule. In patients with chronic liver disease the differential diagnosis of hypodense lesions in the portal or equilibrium phase is hypovascular HCC, peripheral cholangiocarcinoma, dysplastic nodules, and regenerative nodules. Other lesions, such as liver metastases from other primary tumors, are rare.
Multiple benign masses occurring in the cirrhotic liver can mimic a malignant tumor. By definition, regenerative nodules are present in all cirrhotic livers. Regenerative nodules are formed by regenerative hepatocytes surrounded by fibrotic septa. They can vary from 1 to 3 mm in micronodular cirrhosis to 3 to 15 mm in macronodular cirrhosis. Histologically they are composed of normal hepatocytes, and their blood supply is predominantly portal. Because the blood supply and architecture of regenerative nodules are similar to adjacent normal liver parenchyma, visualization of regenerative nodules is difficult. On unenhanced scans they blend in with other regenerative nodules and fibrosis, and those seen are typically revealed as low-attenuation nodules because they contain iron or glycogen or are surrounded by low-attenuation fibrous tissue. Occasionally they appear as slightly hyperdense lesions on noncontrast studies. More often they appear in the equilibrium phase as tiny hypodense lesions. Although infrequent, large regenerative nodules may present as low-density lesions in the arterial, portal, and equilibrium phases, mimicking hypovascular HCCs.
Dysplastic nodules are regenerative nodules containing cellular atypia without frank malignant characteristics and are seen in 15% to 25% of cirrhotic livers. They are supplied primarily by the portal vein, although high-grade dysplastic nodules may develop arterial hypervascularity. In a series of patients undergoing hepatic transplantation, the sensitivity of helical CT was 39% (9 of 23) with all of the lesions being hypoattenuating.
Large studies are needed to determine the exact sensitivity and specificity of helical CT in the detection of HCC. Lim et al reported a sensitivity of 71% (15 of 21) for helical CT in the detection of HCC. The detection rate for lesions less than 2 cm was 60%, and the detection rate for lesions larger than 2 cm was 82%. In the series of Valls et al helical CT had a sensitivity of 79.6% (39 of 49) and a positive predictive value of 86.6% in the detection of HCC. There were six false-positive results, largely related to macronodular regenerative nodules and hyperplastic dysplastic nodules.
The detection and staging of HCC is essential in the pretransplant evaluation. Studies support liver transplantation in patients with a solitary HCC that is less than 5 cm or with no more than three tumor nodules (each 3 cm or less in diameter) as long as there is no evidence of vascular invasion and extrahepatic spread. Following these criteria, the reported actuarial survival rate is 75% at 4 or 5 years.
Magnetic resonance imaging (MRI) is now frequently used in transplant imaging. It is used as an alternative in patients who are allergic to iodinated contrast media. It can provide information on focal liver lesions and can clarify CT findings in cases of focal fatty change. It can provide information regarding the biliary tree, and three-dimensional time-of-flight gadolinium-enhanced MRA techniques permit visualization of the arterial and portal venous system. MRI is used to help distinguish dysplastic nodules from HCC. Dysplastic nodules are typically hyperintense on nonenhanced T1-weighted images and of low signal intensity on T2-weighted images. They are almost never hyperintense on T2-weighted images.
Regenerative nodules typically are isointense on T1-weighted images and low signal intensity nodules on T2-weighted and gradient-recalled images. HCCs are isointense or hyperintense on nonenhanced T1-weighted images and hyperintense, isointense, or hypointense on T2-weighted images ( Fig. 35-2 ). Hyperintensity on T2-weighted images is characteristic of HCC and is related to a lower degree of histological differentiation. On contrast-enhanced images, most HCCs exhibit diffuse enhancement during the arterial phase, with rapid washout during the portal (venous) phase.
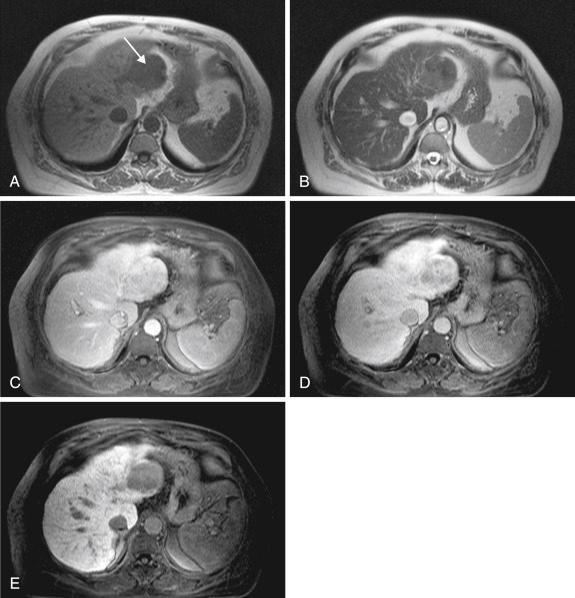
Other typical findings of HCC on MRI include a visible tumor capsule, a mosaic pattern, intratumoral fat deposition, portal or hepatic vein invasion, and arterioportal venous shunting. These major findings may be absent in very small tumors, with only the hypervascularity detected.
The HCC capsule, a major morphological finding in HCC, is a fibrous area surrounding the tumor formed by condensation and collagenation of reticulum fibers after the disappearance of hepatocytes from compression of the tumor. It usually is hypointense on unenhanced T1- and T2-weighted spin-echo images, hypointense on unenhanced gradient echo images, and hyperintense on delayed postgadolinium images. The presence of fatty change within the tumor is another primary and characteristic finding in HCC.
Fibrous septa and a mosaic pattern are characteristic of HCC and are well seen, especially after contrast injection.
Currently breath-hold T1- and T2-weighted images of the liver are recommended because they avoid the motion artifact commonly seen with conventional longer spin-echo MRI sequences. For T2-weighted images, breath-hold turbo spin echo (TSE) with long echo train or half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequences are recommended. For T1-weighted images, breath-hold gradient-echo sequences permit scanning of the entire liver in a single breath-hold and allow dynamic contrast–enhanced images, which allow the entire liver to be imaged in the arterial phase.
Breath-hold chemical shift (in phase and opposed phase) can show fatty infiltration of the liver as well as fat within hepatic nodules. Chemical-shift MRI techniques, which are based on the difference in resonance frequency of water and fat protons, is the most reliable MRI technique in detecting intratumoral fat. Lesions containing a mixture of fat and water protons exhibit low signal intensity on opposed-phase images because the signal from water cancels the signal from fat. High signal intensity is seen on in-phase images because the signals are summed.
After the T1 and T2 unenhanced MRI study, extracellular-type gadolinium chelate contrast agent is injected, and contrast-enhanced images are obtained in the arterial, portal, and equilibrium phases. Images in the arterial phase (15 to 20 seconds after injection) are needed in cirrhotic livers to show hypervascular lesions or small HCCs.
Imaging in the portal venous phase (60 seconds after injection) and the equilibrium phase (90 seconds to 5 minutes after injection) after contrast is important for showing washout of HCC and delayed enhancement of the capsule.
Although MRI has helped solve diagnostic questions in cirrhotic patients, because the development of HCC in chronic liver disease is a progressive process ranging from regenerative nodules to low- or high-grade dysplastic nodules and HCC, the detection and characterization of nodular lesions in cirrhotic livers remains a challenge. With MRI, regenerative nodules may be hypointense on all pulse sequences if they contain iron and may be hyperintense on T1-weighted images. They do not enhance on the arterial phase postgadolinium and do not show a capsule in delayed-phase images. Iron-containing siderotic regenerative nodules are well shown as low-signal-intensity nodules on MRI and are seen much better than with CT.
Although there is considerable overlap in signal intensity on unenhanced T1- and T2-weighted images between dysplastic nodules and HCC, it has been reported that low-grade dysplastic nodules have a tendency to show hypointensity on T2-weighted images and hyperintensity on T1-weighted images. HCC has an isointense or hyperintense pattern on T1-weighted images and is isointense with partial hyperintensity on T2-weighted images.
Because of their predominantly portal supply, low-grade dysplastic nodules do not typically capture extracellular contrast in arterial-phase images. Even though it has been shown that 96% of dysplastic nodules have a portal blood supply and 94% of HCCs have an arterial blood supply, the blood supply of dysplastic nodules is controversial and variable.
Currently, although some imaging features on MRI are reported to be characteristic for dysplastic nodules, it remains difficult to diagnose them definitively by any imaging technique.
Difficulties with lesion characterization have been affected by the development of newer gadolinium-based contrast agents. The detection and characterization of liver lesions using gadolinium-based contrast agents is based mainly on the assessment of vascularity and perfusion. However, because cirrhosis is characterized by variable disturbances in hepatic blood flow because of disruption of normal anatomy, assessment of blood flow to hepatocellular nodules may be difficult with conventional extracellular gadolinium-containing agents. Well-differentiated HCC may have portal supply and show hypoenhancement, which may evade detection and be confused with benign nodules. With cirrhosis the presence or absence of contrast may be difficult to assess in small (<2-cm lesions). The newer combined extracellular-hepatobiliary agents have imaging properties of conventional extracellular agents but also possess hepatocellular function. In contrast to extracellular agents these agents are actively taken up by hepatocytes and subsequently secreted into the biliary system. Two agents currently approved by the Food and Drug Administration are gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid (gadoxetate disodium [Gd-EOB-DTPA], gadoxetic acid [Eovist or Primovist]) and gadobenate dimeglumine (MultiHance). In cirrhotic livers the peak parenchymal enhancement may be delayed and may not be achieved for 40 minutes or more because of impaired transport mechanisms. There may also be delayed biliary excretion with delayed and reduced enhancement of the bile ducts. Blood pool enhancements may be prolonged, but peak enhancements of hepatic and portal veins is of shorter duration and lower intensity. On Gd-EOB-DTPA administration the contrast behavior of HCCs in the dynamic phases (arterial, portovenous, and equilibrium phases) is comparable to that with extracellular fluid Gd-based contrast agents with rapid arterial enhancement followed by rapid washout. In the hepatocyte phase, however, typical HCCs are seen as areas of low intensity relative to surrounding liver parenchyma because they do not have the ability to take up Gd-EOB-DTPA (see Fig. 35-2 ). Regenerative nodules typically show Gd-EOB-DTPA uptake and excretion because of preserved hepatic function and intact ion transporters and have signal similar to that of background liver. In the hepatocyte phase, dysplastic nodules that have retained the ability to take up the agent but not to excrete it appear hyperintense because of intracellular cholestasis, whereas nodules that have lost the ability to take up the agent are hypointense.
Although some benign hyperenhancing nodules such as small hemangiomas and focal nodular hyperplasia rarely are encountered in cirrhotic patients, the diagnosis of HCC is highly likely when a hypervascular nodule is identified in a cirrhotic liver. In the absence of other major characteristic findings of HCC, the hypervascularity of the nodule in the arterial phase may be the only feature that helps to diagnose small HCC. These small HCCs should be differentiated from the hyperattenuating transitory parenchymal areas detected on the arterial phase of dynamic CT or MRI, which are attributed to nonspecific arterioportal shunts caused by cirrhotic changes or produced by iatrogenic vascular injury. A rounded nodular shape and delayed washout favor the diagnosis of HCC. Geographical morphological characteristics and isointensity on delayed venous-phase images favor the diagnosis of vascular nontumoral change. With Gd-EOB-DTPA, areas of transient arterial enhancement are usually isointense to parenchyma because they contain functional hepatocytes.
Portal or hepatic venous invasion is characteristic of HCC. On MRI, portal vein tumor thrombus shows as an intravascular mass of intermediate signal on T1-weighted images. Similar to liver tumor, the intravascular mass enhances in the arterial phase after contrast injection. Gadolinium-enhanced MRA techniques are particularly useful in visualization of the hepatic artery and the portal venous system.
With triphasic contrast-enhanced helical CT or dynamic gadolinium-enhanced MRI, small, 2-cm, hypervascular HCCs may be detected in the arterial phase.
Although ultrasound, CT, and MR imaging are all useful in the diagnosis of HCC in cirrhotic patients, a recent study has shown that significantly higher diagnostic accuracy, sensitivity, and negative predictive value is achieved with dynamic plus hepatobiliary phase MRI compared with ultrasonography, multidetector computed tomography, and dynamic phase MRI alone. The specificity and positive predictive value of ultrasonography was significantly lower than that of multidetector computed tomography, dynamic phase MRI, and dynamic plus hepatobiliary phase MRI. The MRI imaging was performed using the extracellular gadolinium-containing contrast agent (MultiHance).
Several organizations have convened study groups to develop a comprehensive reporting and data system for CT and MRI of the liver in patients with cirrhosis and other risk factors for HCC. These include the American Association for the Study of Liver Diseases, the United Network for Organ Sharing (UNOS), and the American College of Radiology. In 2011 UNOS released its Organ Procurement and Transplantation Network (OPTN) transplant imaging criteria policy for liver transplant candidates with HCC. The criteria were designed to improve specificity of the diagnosis of HCC in imaging and determining eligibility for HCC exception points. Under the criteria, lesions must be classified according to the OPTN classification. OPTN class 5 lesions correspond to an imaging diagnosis of HCC. The imaging diagnosis is based on lesion hyperenhancement on late hepatic arterial images and depending upon lesion size, other features, including washout on venous/delayed phase images, late capsule or pseudocapsule enhancement, and lesion growth. The imaging criteria currently do not take into account hepatobiliary contrast agents or imaging-based criteria for the diagnosis of vascular invasion.
Cholangiography, although not a routine part of the pretransplant evaluation, may be performed in cases of sclerosing cholangitis, which is the third most common indication for liver transplantation. Magnetic resonance cholangiography is useful. The technique is noninvasive and can provide useful images of the biliary tree. The technique does require patient cooperation. Limitations include image degradation by motion artifact and difficulty detecting and assessing severity of strictures. Its sensitivity and specificity are yet to be determined.
Because occult cholangiocarcinoma is found in 10% of the resected liver specimens of patients with primary sclerosing cholangitis, biopsy of suspicious narrowed areas should be considered before transplantation. Arteriography is performed when suspected vascular problems are detected on ultrasound studies or in difficult cases. In many cases MRA techniques can obviate the need for arteriography and venography, because the IVC and hepatic veins are well seen with MRA. The portal vein is also well seen (see Fig. 35-2 ). Another angiographic procedure useful in the management of patients awaiting liver transplantation is the transjugular intrahepatic portosystemic shunt (TIPS) procedure, which involves the creation of a tract between a hepatic vein and the portal vein with placement of a stent in the tract. The procedure is performed with jugular vein access for catheterization of a hepatic vein. With fluoroscopic guidance, a specially designed needle-catheter system is used to create a channel from the hepatic vein through the hepatic parenchyma to the portal vein. When the tract has been created, it is dilated with a balloon angioplasty catheter, and a metallic stent is placed in the tract to maintain patency. Various stents are used, including bare metal and polytetrafluoroethylene-covered stents, which have been shown to have higher patency rates. The procedure permits effective nonoperative decompression of the portal system. The TIPS procedure has been used successfully to stabilize patients during the period before transplantation. Liver transplantation was not impeded in any of these cases. When the stents are properly placed well within the liver, with minimal extension into the portal vein or IVC, liver transplantation can be performed in the standard manner. Experience indicates that TIPS is also useful for the treatment of intractable ascites.
Radionuclide imaging studies are rarely performed on donors. Occasionally, single-photon emission CT liver-spleen scans using technetium Tc 99m sulfur colloid are performed to determine the volume of the native liver.
A bone scan is indicated for patients being evaluated for liver transplantation because of a hepatic tumor.
Mammography is performed in women who are 45 years of age or older and have a family history of breast cancer.
Multiple imaging modalities are available for evaluation of the liver transplant patient. In the immediate postoperative period, chest radiographs are obtained daily to evaluate for atelectasis, pneumonia, diaphragmatic paralysis, and pleural effusions. Doppler ultrasonography is the preliminary imaging modality for gross evaluation of the liver parenchyma, biliary tree, and vasculature. When ultrasound findings are indeterminate or do not correlate with clinical findings, CT is usually performed. The major indications for CT are detection of bile leak, hemorrhage, or abscess. CT and MRI are useful for assessment of vasculature. For suspected biliary strictures, T-tube cholangiography and MR cholangiopancreatography are used. Conventional arteriography or cholangiography is indicated for confirmation of noninvasive imaging findings or at time of treatment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here