Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Respiratory infections are the most common illnesses occurring in humans and pneumonia is the leading cause of death due to infectious disease and the sixth most common cause of death in the United States. Pneumonia is an acute infection of the pulmonary parenchyma that is associated with at least some symptoms of acute infection, accompanied by the presence of an acute infiltrate on a chest radiograph.
Currently accepted classifications of pneumonia include community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), ventilator-associated pneumonia (VAP) and health care–associated pneumonia (HCAP).
The diagnosis of CAP is based on the presence of select clinical features (e.g. cough, fever, sputum production and pleuritic chest pain) and is supported by imaging of the lung, usually by chest radiography ( Box 5.1 ).
| Radiographic Findings | Most Common Organisms |
|---|---|
| Lobar consolidation | Streptococcus pneumoniae , Klebsiella pneumoniae |
| Round pneumonia | S. pneumoniae |
| Bronchopneumonia | Staphylococcus aureus , gram-negative bacilli, anaerobes, S. pneumoniae |
| Interstitial pneumonia | Virus, Mycoplasma pneumoniae |
| Cavity formation | Mycobacterium tuberculosis , S. aureus , gram-negative bacilli |
The spectrum of causative organisms of CAP includes gram-positive bacteria such as Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae and Staphylococcus aureus , as well as atypical organisms such as Mycoplasma pneumoniae , Chlamydia pneumoniae , or Legionella pneumophila, and viral agents such as influenza A virus and respiratory syncytial viruses. Pulmonary opacities are usually evident on the radiograph within 12 hours of the onset of symptoms. Although the radiographic findings do not allow a specific aetiological diagnosis, they may be helpful in narrowing down the differential diagnosis.
Hospital-acquired pneumonia (HAP) may be defined as one occurring after admission to hospital and was neither present nor in a period of incubation at the time of admission. Hospital-acquired pneumonia (nosocomial) is the leading cause of death from hospital-acquired infections and a serious public health problem. It occurs most commonly among intensive care unit (ICU) patients, predominantly in individuals requiring mechanical ventilation.
Microorganisms responsible for VAP may differ according to the population of patients in the ICU, the duration of hospital and ICU stays, and the specific diagnostic method(s) used. The spectrum of causative pathogens of VAP in humans is S. aureus , Pseudomonas aeruginosa and Enterobacteriaceae.
When pneumonia is associated with health care risk factors such as prior hospitalisation, dialysis, residing in a nursing home, and immunocompromised state, it is now classified as health care–associated pneumonia (HCAP). The number of individuals receiving health care outside the hospital setting, including home wound care or infusion therapy, dialysis, nursing homes and similar settings is constantly increasing.
Infectious pneumonia needs to be differentiated from aspiration pneumonia, which also presents with patchy consolidations typically in the dependent portions of the lung (superior segments of the lower lobes and posterior segments of the upper lobes). The pattern is very variable, dependent on the quantity and quality of aspirated material, and ranges from tree-in-bud to patchy consolidations, usually multilobar and bilateral in distribution, though more frequently and more extensively to the right side due to the vertical position of the right-sided central airways.
A clinical diagnosis of pneumonia can usually be readily established on the basis of signs, symptoms and chest radiographs. However, distinguishing pneumonia from conditions such as left heart failure, pulmonary embolism and aspiration pneumonia may sometimes be difficult, especially as patients with pre-existing lung disease (severe emphysema, interstitial lung disease etc.) may develop very atypical patterns of pneumonia.
Although different patterns of pneumonia are associated with certain underlying microorganisms, it has to be clearly stated that there is no specific radiological pattern of pneumonia caused by one particular microbe. Overlap of imaging findings also with respect to course over time makes the differentiation of aetiologies based solely on the radiograph unreliable.
The spectrum of causative pathogens of pneumonia in humans includes gram-positive bacteria ( S. pneumoniae and S. aureus ), gram-negative bacteria ( H. influenzae, Escherichia coli and Klebsiella pneumoniae ), atypical bacteria ( Mycoplasma pneumoniae , C. pneumoniae and L. pneumophila ), oral anaerobes and viral agents, fungi, protozoa and parasites.
Differentiation of aetiologies based solely on the radiograph is not reliable, yet the pattern of abnormalities can be very useful in formulating a differential diagnosis of the nature of the disease. New emerging pathogens have been recognised such as community-acquired methicillin-resistant S. aureus , human metapneumovirus (hMPV), avian influenza A viruses (H5N1), coronavirus associated with severe acute respiratory syndrome (SARS), swine flu (H1N1) and Middle East respiratory syndrome coronavirus (MERS-CoV).
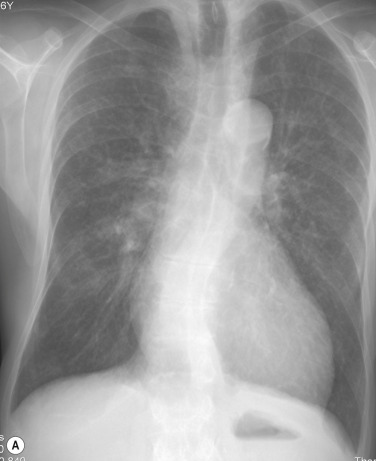
Chest radiography remains an important component of evaluating a patient with a suspicion of pneumonia, and is usually the first examination to be obtained. Although chest radiographs are of limited value in predicting the causative pathogen, they are of good use to determine the extent of pneumonia and to detect complications (e.g. cavitation, abscess formation, pneumothorax and pleural effusion).
High-resolution computed tomography (HRCT) with thin < 2 mm thick slices, has been shown to be more sensitive than the radiograph in the detection of subtle abnormalities and may show findings suggestive of pneumonia up to 5 days earlier than chest radiographs
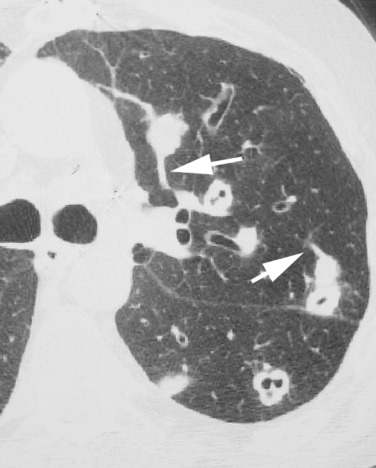
High-resolution CT is recommended in patients with clinical suspicion of infection and normal or non-specific radiographic findings and in patients with increased risk of pulmonary infections (e.g. neutropenia) ( Fig. 5.1 ). CT is also indicated in patients with pneumonia and persistent or recurrent pulmonary opacities to diagnose or rule out underlying or alternative disease processes.
According to the American Thoracic Society (ATS), the presence of radiographically visible opacification is part of the definition of pneumonia, although there may be a time delay of several hours between onset of clinical symptoms and radiographic changes. Specific conditions may further the delay or cause a negative chest radiograph.
Regression of pneumonia over time varies with the underlying organism, patient comorbidity and patient age and can take between 1 to 2 weeks or up to 2 months.
Pneumonia is usually divided according to the chest imaging appearance into lobar pneumonia, bronchopneumonia, and interstitial pneumonia. Common associated findings include hilar and mediastinal lymphadenopathy, pleural effusion, cavitation, and chest wall invasion. These findings are not specific and may be seen in other conditions. In up to 10% of patients with proven Pneumocystis pneumonia (PCP), the chest radiograph is normal.
In lobar pneumonia , the inflammatory exudate begins in the distal air spaces adjacent to the visceral pleura, and then spreads via collateral air drift routes (pores of Kohn) to produce uniform homogeneous opacification of partial or complete segments of lung and, occasionally, an entire lobe. Occasionally, infection is manifested as a spherical focus of consolidation ( Fig. 5.2 ). An air bronchogram is frequently seen. S. pneumoniae is by far the most common cause of complete lobar consolidation. Other causative agents that produce complete lobar consolidation include K. pneumoniae and other gram-negative bacilli, L. pneumophila , H. influenzae , and, occasionally, M. pneumoniae .

Characteristic manifestations on CT are lobar or sublobar consolidations, sharply demarcated by the interlobar fissure.
Bronchopneumonia (lobular pneumonia) is characterised histologically by predominantly peribronchiolar inflammation. Although initially patchy, progression of disease results in lobular and segmental consolidation ( Fig. 5.3 ). The initial peribronchiolar inflammation manifests radiologically as patchy airspace nodules with poorly defined margins. An air bronchogram is usually absent. The most common causative organisms of bronchopneumonia are S. aureus, H. influenzae, P. aeruginosa and anaerobic bacteria.
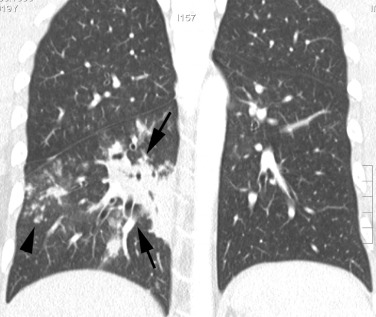
Characteristic manifestations of bronchopneumonia on HRCT include centrilobular ill-defined nodules and branching linear opacities, airspace nodules, and multifocal lobular areas of consolidation.
The term atypical pneumonia (interstitial pneumonia) was initially applied to the clinical and radiographic appearance of lung infection not behaving or looking like that caused by S. pneumoniae . In the literature, the term ‘atypical pneumonia’ (as opposed to ‘bacterial pneumonia’) is still in wide usage, although technically incorrect. Many causative organisms are identified as bacteria, albeit unusual types ( Mycoplasma is a type of bacteria without a cell wall and Chlamydia are intracellular parasites). It is therefore important to realise that the term ‘atypical pneumonia’—if more correctly based on the underlying type of causative pathogen—does not only refer to an interstitial pattern ( Pneumocystis jiroveci pneumonia, certain viral infections but also infections presenting with dense consolidation such as Legionella , Mycoplasma , Chlamydia, etc.).
The usual causes of interstitial pneumonia are viral and mycoplasmal infections that radiographically present with focal or diffuse small heterogeneous opacities.
See Box 5.2 .
Staphylococcus aureus , including methicillin-resistant S. aureus
Anaerobic aspiration syndrome
Klebsiella spp.
Streptococcus milleri
Right-sided endocarditis
Tuberculosis
Nontuberculous mycobacteria
Lung abscess is defined as a localised necrotic cavity containing pus and the most common cause is aspiration. A lung abscess occurs most commonly in the posterior segment of an upper lobe or the superior segment of a lower lobe ( Fig. 5.4 ). Common causes of lung abscess include anaerobic bacteria (most commonly Fusobacterium nucleatum and Bacteroides sp.), S. aureus , P. aeruginosa and K. pneumoniae and radiologically manifest with single or multiple masses that are often cavitated.
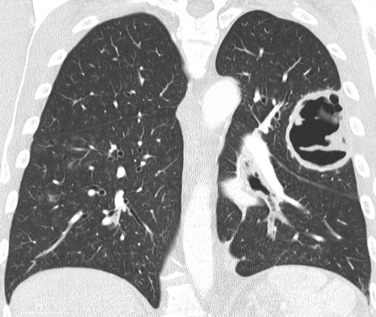
Pulmonary gangrene is a rare complication of pneumonia characterised by the development of fragments of necrotic lung within an abscess cavity (pulmonary sequestrum). Radiological manifestations consist initially of small lucencies within an area of consolidated lung, usually developing within lobar consolidation associated with enlargement of the lobe and outward bulging of the fissure (bulging fissure sign).
Pneumatocele is a thin-walled, gas-filled space that usually develops in association with infection. It presumably results from drainage of a focus of necrotic lung parenchyma followed by check-valve obstruction of the airway subtending it, enabling air to enter the parenchymal space during inspiration but preventing its egress during expiration. The complication is caused most often by S. aureus in infants and children and P. jiroveci in patients who have acquired immune deficiency syndrome (AIDS) ( Fig. 5.5 ).
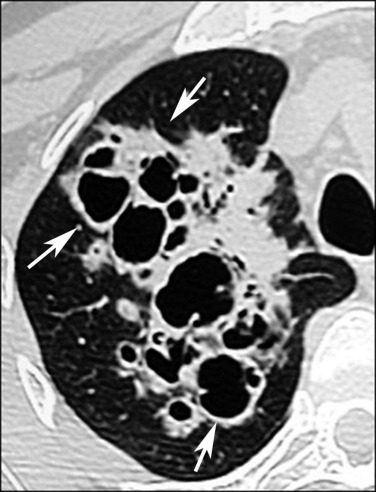
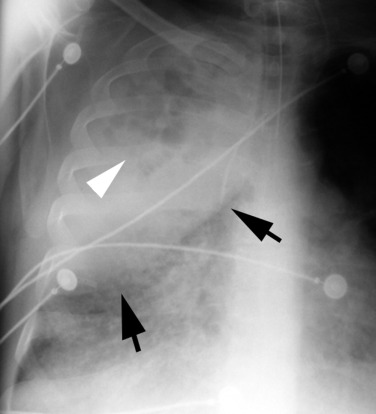
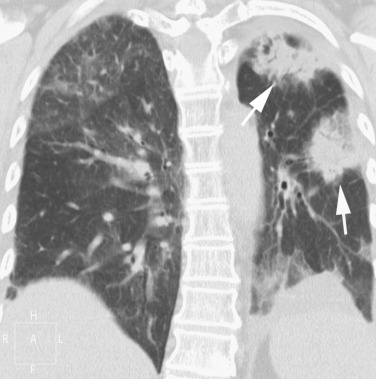
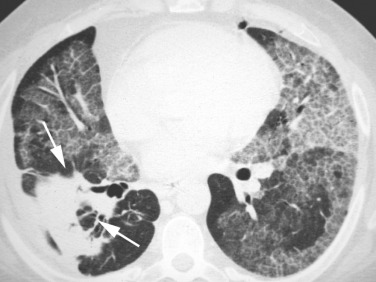
Septic emboli to the lungs originate in a variety of sites, including cardiac valves (endocarditis), peripheral veins (thrombophlebitis), and venous catheters or pacemaker wires. On cross-sectional CT images the nodules often appear to have a vessel leading into them (‘feeding vessel’ sign) ( Fig. 5.6 ). Dependent on the underlying organism, nodules cavitate typically at different time points, resulting in the simultaneous appearance of solid nodules and nodules with varying sizes of cavitations.
Empyema occurs in less than 5% of pulmonary infections. The pathogens traditionally associated with empyema are S. pneumoniae , Streptococcus pyogenes and S. aureus . Radiographically, early signs include obliteration of the costophrenic angle. Complete opacification of a hemithorax and contralateral mediastinal displacement may occur in large effusions. Typically, an infected pleural effusion is encapsulated. Other CT features include (1) pleural enhancement and thickening of the parietal pleura (split pleura sign), (2) increased density of extrathoracic fat and (3) thickening and increased density of the extrapleural subcostal fat.
Bronchopleural fistula is a sinus tract between the bronchus and the pleural space that may result from necrotising pneumonias, lung surgery, lung neoplasms and trauma. Imaging features consist of (1) increase in intrapleural air space, (2) appearance of a new air-fluid level, (3) changes in an already present air-fluid level, (4) development of tension pneumothorax and (5) demonstration of actual fistulous communication by CT.
The clinician evaluating the patient with a known or suspected diagnosis of pulmonary infection faces a diagnostic challenge. This is because most processes present with similar signs and symptoms, and the radiographic findings of an individual pneumonia do not provide a specific aetiological diagnosis. Furthermore, radiographic manifestations of a given infectious process may be variable, depending on the immunological status of the patient as well as the pre- or coexisting lung disease.
The most useful imaging techniques available for the evaluation of the patient with known or suspected pulmonary infection are chest radiography and CT.
S. pneumoniae is responsible for approximately one-third of all cases of CAP.
Pneumoccocal infections occur predominantly in the winter and early spring and are often associated with prior viral infection. Risk factors for the development of pneumococcal pneumonia include the extremes of age, chronic heart or lung disease, immunosuppression, alcoholism, institutionalisation and prior splenectomy. The characteristic clinical presentation is abrupt in onset, with fever, chills, cough and pleuritic chest pain. In the elderly, these classic features of disease may be absent and pneumonia may be confused with or confounded by other common medical problems, such as congestive heart failure, pulmonary thromboembolism or malignancy.
The typical radiographic appearance of acute pneumococcal pneumonia consist of an homogeneous consolidation that crosses segmental boundaries (nonsegmental) but involves only one lobe (lobar pneumonia) ( Fig. 5.7 ). Occasionally, infection is manifested as a spherical focus of consolidation that simulates a mass (round pneumonia). Complications such as cavitation and pneumatocele formation are rare. Pleural effusion is common and is seen in up to half of patients.

The CT ‘angiogram sign’, initially described in the lobar form of lepidic adenocarcinomas as the enhancement of branching pulmonary vessels in a homogeneous low-attenuation consolidation of lung parenchyma, may also occur in lobar pneumonia.
K. pneumoniae is among the most common gram-negative bacteria, accounting for 0.5%–5.0% of all cases of pneumonia. The radiographic features include bulging fissures due to volume increase of the infected lobe, sharp margins of the advancing border of the pneumonic infiltrate and early abscess formation ( Fig. 5.8 ). CT findings consist of ground-glass attenuation, consolidation and abscess formation.
Legionella is one of the most common causes of severe CAP in immunocompetent hosts. Human infection may occur when Legionella contaminates water systems, such as air conditioners and condensers. Risk factors for the development of L. pneumophila pneumonia include immunosuppression, post-transplantation, cigarette smoking, renal disease and exposure to contaminated drinking water. Patients with Legionella pneumonia usually present with fever, cough (initially dry and later productive), malaise, myalgia, confusion, headaches and diarrhoea.
Imaging findings include peripheral airspace consolidation similar to that seen in acute S. pneumoniae pneumonia. In many cases, the area of consolidation rapidly progresses to occupy all or a large portion of a lobe (lobar pneumonia) to involve contiguous lobes or to become bilateral ( Fig. 5.9 ). Occasionally, Legionella pneumonia may result in a round area of consolidation simulating a mass (round pneumonia). Pleural effusion may occur in 35%–63% of cases.

C. pneumoniae (strain TWAR) is the most commonly occurring gram-negative intracellular bacterial pathogen. It is frequently involved in respiratory tract infections and has also been implicated in the pathogenesis of asthma in both adults and children. On CT, C. pneumoniae pneumonia demonstrates a wide spectrum of imaging findings that are similar to those of S. pneumoniae pneumonia and M. pneumoniae pneumonia, consisting of areas of consolidation, bronchovascular bundle thickening, nodules, small pleural effusion, lymphadenopathy, reticular or linear opacities and airway dilatation ( Fig. 5.10 ).
Moraxella catarrhalis (formerly known as Branhamella catarrhalis ) is an intracellular gram-negative coccus now recognised as one of the common respiratory pathogens. M. catarrhalis causes otitis media and sinusitis in children and relatively mild pneumonia and acute exacerbation in older patients with chronic obstructive pulmonary disease (COPD). It is currently considered the third most common cause of community-acquired bacterial pneumonia (after S. pneumoniae and H. influenzae ). M. catarrhalis seldom results in pneumonia in previously healthy individuals. Most patients with this type of pneumonia (80% to 90%) have underlying chronic pulmonary disease and their clinical illness may be difficult to distinguish from exacerbations of lung disease by other causes. Chest radiographs show bronchopneumonia or lobar pneumonia that usually involves a single lobe. Additional CT findings include ground-glass opacities, bronchial wall thickening and centrilobular nodules. Small effusions occur in one-third of patients.
Nocardia is a genus of filamentous gram-positive, weakly acid-fast, aerobic bacteria that affects both immunosuppressed and immunocompetent patients. Nocardiosis usually begins with a focus of pulmonary infection and may disseminate through haematogenous spread to other organs, most commonly to the central nervous system (CNS). Imaging findings are variable and consist of unifocal or multifocal consolidation and single or multiple pulmonary nodules. Cavitation is common and lymphadenopathy or chest wall involvement may occur. Nocardia asteroides infection may complicate alveolar proteinosis ( Fig. 5.11 ).
Thoracic actinomycosis is a chronic suppurative pulmonary or endobronchial infection caused by Actinomyces sp., most frequently Actinomyces israelii , which is considered to be a gram-positive branching filamentous bacterium. Actinomycosis has the ability to spread across fascial planes to contiguous tissues without regard for normal anatomic barriers. On CT, parenchymal actinomycosis is characterised by airspace consolidation with cavitation, or central areas of low attenuation and adjacent pleural thickening ( Fig. 5.12 ). Endobronchial actinomycosis can be associated with a foreign body (direct aspiration of a foreign body contaminated with Actinomyces organisms) or a broncholith (secondary colonisation of a pre-existing endobronchial broncholith by aspirated Actinomyces organisms).

The most common rickettsial lung infection is sporadic or epidemic Q-fever pneumonia caused by Coxiella burnetii , an intracellular, gram-negative bacterium.
Affected patients are invariably debilitated by a chronic medical or pulmonary disease. These bacteria are generally aspirated from a colonised upper respiratory tract or may be inhaled or spread haematogenously. The lower lobes predominantly tend to be affected and the radiographic pattern is similar to that seen with S. aureus infections in adults.
Infection is mainly acquired by inhalation from farm livestock or their products, and occasionally from domestic animals. Imaging findings consist of multilobar airspace consolidation, solitary or multiple nodules surrounded by a halo of ‘ground-glass’ opacity and vessel connection, and necrotising pneumonia.
Other rickettsial infections such as Rocky Mountain spotted fever are usually tick-borne and occasionally demonstrate diffuse heterogeneous or homogeneous opacities on chest radiographs, perhaps representing vasculitis or cardiogenic pulmonary oedema.
Tularaemia is an acute, febrile, bacterial zoonosis caused by the aerobic gram-negative bacillus Francisella tularensis. It is endemic in parts of Europe, Asia and North America. Primary pneumonic tularaemia occurs in rural settings. Humans become infected after introduction of the bacillus by inhalation, intradermal injection or oral ingestion. Chest radiographic findings are scattered multifocal consolidations, hilar adenopathy and pleural effusion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here