Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
As a dermatologist walks into the examination room of the patient in Fig. 123.1 , several diagnostic possibilities likely come to mind. The patient's history, additional physical findings, and other clues help narrow the differential diagnosis. In this case, knowing the patient's history of atopic dermatitis lends context to the appearance of punched-out erosions and allows one to arrive at the diagnosis of eczema herpeticum. Therefore, awareness of the epidemiology of a disease, how it is distributed within populations, and the factors that influence its distribution can assist in establishing a diagnosis .

Considering the high or increasing prevalence of many skin conditions, dermatologists have the potential to play an important role in public health research and policy. This chapter highlights the relevance of dermatologic conditions to public health, the impact epidemiology can have on a dermatology practice, and major types of public health studies, as well as research design concepts and terminology used in epidemiology.
Skin conditions are a major cause of morbidity worldwide. Based on analysis of global burden of disease data , skin diseases accounted for over 36 million disability-adjusted life years (DALYs) lost in 2010 and ranked as the fourth most common cause of nonfatal disease burden ( Table 123.1 ). In the US, dermatology accounts for 4% of all outpatient visits, representing the third most common subspecialty ambulatory visit (after ophthalmology and orthopedics). In addition, ~5–8% of primary care and 4% of emergency department visits are primarily for dermatologic conditions, with the most common outpatient diagnoses including eczema, skin infections, benign neoplasms, acne, psoriasis, and skin cancer . Notably, in 2010, the symptom of itch accounted for 1% of all outpatient visits in the US .
| DISABILITY-ADJUSTED LIFE YEAR (DALY) RATES FOR ALL SKIN CONDITIONS COMBINED, 2010 | |
|---|---|
| DALY rate/100 000 individuals | Example countries |
| <508 | Germany |
| 509–562 | Canada, Spain, United Kingdom |
| 563–609 | Brazil, France, Japan, United States |
| 610–677 | Australia, Finland, Taiwan |
| 678–740 | Ethiopia, Haiti |
| >740 | Papua New Guinea, Sudan |
Not only are dermatologic conditions common, but some are rising in incidence. For example, the incidence of melanoma increased by ~2.9% per year in the US from 1981 to 2006, and then at a lower rate of ~0.9% per year from 2007 to 2013 ; these increases have included all tumor thickness groups, although mortality has overall been stable with improvement in recent years . In addition, many countries have experienced an increase in the frequency of non-melanoma skin cancers, i.e. basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs) . Indoor tanning is associated with an increased risk of skin cancer and has reached alarming rates among youth, with indoor tanning exposure in nearly 20% of adolescents in the US, Canada, and Northern and Western Europe .
Ensuring the health of Lesbian, Gay, Bisexual and Trangender people (LGBT) is of importance for all physicians, including dermatologists. Recognition and treatment of sexually transmitted infections such as HIV and syphilis is essential, with the associated cutaneous manifestations often alerting one to the diagnosis (see Chs 78 and 82 ). In addition, high rates of skin cancer are a concern for gay men, based upon reports of 6-fold higher rates of tanning bed use and over double the rates of skin cancer as compared to heterosexual men. These cutaneous carcinomas are also more common and more aggressive in HIV-infected individuals. Dermatologists must continue to address deficits in cultural competence related to transgender patients; an example would be FDA-mandated risk mitigation programs such as iPledge. As emerging data suggests continued health disparities amongst the LGBT community, there is a greater need for healthcare providers who are culturally competent in LGBT health as well as more research on how to evaluate and address the existing disparities.
Epidemiologic studies have yielded information on the etiology, risk factors, natural history, prognosis, incidence, prevalence, and effective treatments of dermatologic diseases. The impact that epidemiologic data can have on patient care and systems-based practice in dermatology is outlined in Table 123.2 .
| USES FOR EPIDEMIOLOGY IN DERMATOLOGY |
| Epidemiology applied at the patient care level |
|
| Epidemiology applied at the systems level |
|
Participants in observational studies are observed and certain outcomes are measured, without external manipulation or an attempt to affect the outcome.
Many of the studies currently being done in dermatology are descriptive. These include case reports and case series. A case report is a detailed description of an individual patient's characteristics (e.g. demographic information), clinical presentation, diagnosis, treatment, and disease course. A case series reports on some aspect(s) of a disease, diagnostic procedure, or treatment in a group of patients with common characteristics . Case reports and series are useful for determining the manifestations of rare conditions, reporting the preliminary outcomes of experimental therapies, and generating hypotheses for larger studies. A major limitation of case series is the lack of a control group ( Table 123.3 ) , although previous data (e.g. on the prevalence of risk factors in the general population) can sometimes be utilized for comparison.
| STUDY TYPES AND THEIR CHARACTERISTICS | ||||||
|---|---|---|---|---|---|---|
| Type of study | Study group | Control group | Association measure frequently used | Advantages | Limitations | Level of evidence for whether a therapy is efficacious * |
| Case series | Persons with disease | None | Varies (e.g. percentile) |
|
|
4 |
| Case–control | Persons with disease | Persons without disease | OR (approximates the RR in rare diseases) |
|
|
3 |
| Cohort | Persons exposed | Persons not exposed | RR or absolute risk † |
|
|
2 ** |
| Cross-sectional | Persons with disease or exposed | Either of the above | OR or relative prevalence |
|
|
2 ** |
| Randomized controlled trials (RCTs) | Persons randomized to treatment | Persons randomized to control | Varies (e.g. RR or percentiles) |
|
|
1 |
* The level of evidence for a therapeutic efficacy has a scale of 1–5, 1 being the best. Expert opinions represent level 5. The level of evidence for therapeutic efficacy for a systematic review depends on the types of studies it reviews. A systematic review of RCTs with good homogeneity ranks above an individual RCT.
** In general, a cohort study (2b) is ranked as better than a cross-sectional study (2c).
† Absolute risk reduction is the incidence rate of disease in the exposed group subtracted by that of the unexposed group. This is affected by the rate of disease in the population; the greater the prevalence of disease, the higher the absolute risk reduction. The reciprocal of absolute risk reduction is the number needed to treat to avoid one person getting the disease.
An example of a valuable case series is the description of scalp involvement in patients with dermatomyositis by Kasteler and Callen . Fourteen of the 17 patients with dermatomyositis who were seen in the authors' practice over a 5-year period had scalp involvement, manifesting as atrophic, erythematous, scaly plaques. Five of the 14 affected individuals had previously been diagnosed with scalp psoriasis or seborrheic dermatitis. This study helped raise awareness of scalp involvement as a manifestation of dermatomyositis.
Case–control, cohort, and cross-sectional studies are often performed to help elucidate the etiology and risk factors of a disease (see Table 123.3 ). These methods involve studying a disease of interest (e.g. cutaneous SCC) and an exposure that is suspected of being a risk factor for the disease (e.g. ultraviolet [UV] radiation), so that the study participants can be categorized as having the disease or not and as being exposed to the potential risk factor or not ( Table 123.4 ).
| CATEGORIZATION OF STUDY PARTICIPANTS, BASED ON THEIR DISEASE AND EXPOSURE | ||
|---|---|---|
| Disease (e.g. cutaneous SCC) | No disease (e.g. no cutaneous SCC) | |
| Exposed (e.g. high-dose UV) |
a | b |
| Non-exposed (e.g. no high-dose UV) |
c | d |
A case–control study identifies a group of individuals with a disease, as well as a comparison group without the disease from the same population. The study design retrospectively evaluates the level of exposure in the disease group (cases), as compared to that in the group without disease (controls). To ensure that those with disease and without are comparable, both types of participants should be sampled from a single population and data collected in the same way for each group . In addition, cases and controls should be matched on possible confounding factors; for example, if there is a 60-year-old female case, then a 60-year-old female control from the same general population would be selected.
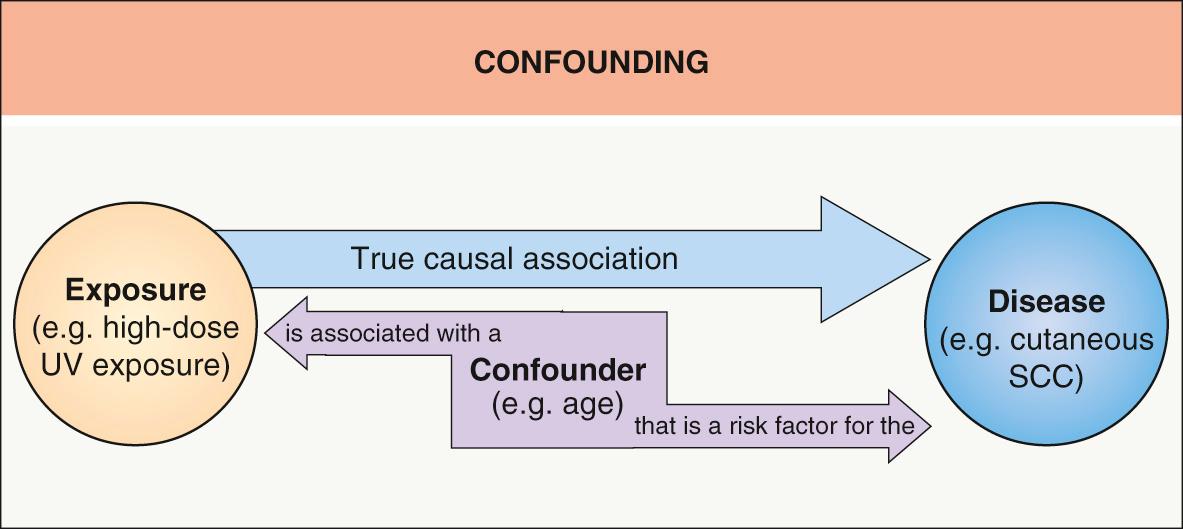
A confounder is an extraneous variable that is associated with both the exposure and the disease being studied; it could therefore account for a part or all of the relationship between the exposure and disease. Although the confounder may be a contributing factor to the disease, it is not caused by the exposure and thus is not along the “causal pathway” between the exposure and disease ( Fig. 123.2 ). Age and gender are examples of possible confounders. These and other characteristics that may be associated with both the exposure and the disease should also be recorded and placed in the statistical model. If an association remains after accounting for confounders, it is more likely to be a true one.
In a case–control study, one can calculate the odds of having had the exposure among those with disease (a/c), as compared to the odds of having had the exposure among those without disease (b/d) (see Table 123.4 ). The association measure used for case–control studies is an odds ratio (OR), which equals (a/c)/(b/d) or ad/bc. An OR = 1 denotes a null association, whereas an OR statistically significantly greater or less than 1 indicates a positive or negative association, respectively. An OR is different from a relative risk (RR), the rate of disease among those exposed divided by that among those unexposed, (a/a+b)/(c/c+d) (see Cohort study section below). While the RR cannot be directly calculated from a case–control study, the OR approximates the RR when the disease is rare.
One of the major advantages of a case–control study is that it can yield information on a disease with many possible predictors, yet use only a limited number of participants. Therefore, it is well-suited for the investigation of rare conditions. Also, these studies are relatively inexpensive and time-efficient. One of the disadvantages of a case–control study is that it is not clear if the exposure preceded the disease, so causality cannot be established. In addition, this type of study has several potential biases. Sampling bias can occur when cases and controls are collected separately and may not be comparable. Because of the retrospective ascertainment of exposure, recall bias can occur; for example, those with disease may recall the exposure with greater detail because they have been contemplating the potential causes of their condition. Of note, a case–control study does not yield information on the incidence or prevalence of a disease.
An example of a recent case–control study is that by Picard et al. , which examined the association between psoriasis (here the “exposure”) and coronary artery disease. They compared the prevalence of psoriasis in case patients referred to a cardiologist for coronary artery disease (CAD; confirmed by angiography) to that in age- and gender-matched control patients without CAD (lack of history or symptoms; no Q wave on electrocardiogram) who were referred to a surgeon for a non-cardiovascular condition. The investigators found that psoriasis was present in 8.0% of cases and 3.4% of controls, with an OR of 2.64 (95% confidence interval [CI], 1.42–4.88). In other words, those with CAD had 2.64 times greater odds of having psoriasis, when compared to those without CAD. The 95% CI does not include 1, signifying that the OR is statistically significant ( Fig. 123.3 ). However, upon adjusting for potentially confounding cardiovascular risk factors in multivariate analysis, the OR decreased to 1.84 (95% CI, 0.99–3.40), which includes 1 and is therefore only of borderline significance.

A cohort study recruits its participants from the general population, and those recruited must be without the disease of interest. Using the example given in Table 123.4 , all participants would need to be SCC-free at the onset of the study. They are then categorized as having or not having high-dose UV exposure and are followed over time. At the end of the study, one can calculate the rate of cutaneous SCC among those with high-dose UV exposure (a/a+b) and compare it to the rate of SCC among those without high-dose UV exposure (c/c+d). Therefore, a cohort study compares the incidence of disease between those exposed and not exposed to particular risk factor(s). This is usually expressed in terms of a RR (see definition above). Similar to an OR, a RR of 1 represents a null association, whereas an RR statistically significantly greater or less than 1 indicates a positive or negative association, respectively. A cohort study can be done prospectively, allowing for more control over measuring outcomes (preferred particularly for fatal diseases), or retrospectively, which is less expensive and requires less time.
One of the advantages of a cohort study is that it can determine the incidence of a disease, which is the number of new cases divided by the total number of people at risk in a particular population (e.g. participants in the study) over a specified time period (e.g. length of study) . It also gives information on the natural history of a disease, since it captures data from the time of disease onset. Another advantage is that a cohort study establishes temporality, as the exposure precedes the outcome, and therefore allows for causal inference between the exposure and disease. The disadvantages are that a cohort study often requires a large sample size and is less feasible for rare outcomes.
A recent cohort study by Zhang et al. looked at the association between tanning bed use and development of skin cancers. Their study population included >70 000 female nurses who were followed between 1989 and 2009. After adjusting for possible confounders (e.g. age, skin type, sun exposure, UV index at place of residence), they found that for an incremental increase of 4 sessions/year in mean use of tanning beds prior to age 35 years, the RR of developing BCC was 1.15 (95% CI, 1.11 to 1.19). Thus the use of tanning beds a mean of 4 or 8 times per year resulted in a ~15% or ~30% higher risk of BCC, respectively, compared to not using tanning beds. This demonstrates a “dose response” effect, i.e. women who used tanning beds more often had a higher skin cancer risk. Furthermore, the authors noted that women exposed to tanning beds in their teenage or college years were at higher risk than those exposed later in life.
Effect modification or interaction occurs when the association between the exposure and disease varies across levels of a variable (e.g. age; Fig. 123.4 ). Therefore, the exposure and effect modifier have an interdependent role in their effect on the disease. When this happens, the association between exposure and disease should be displayed at various levels or strata of the effect modifier .

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here