Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Psychodermatologic disorders include psychophysiologic skin conditions that compromise quality of life and primary psychiatric disorders associated with somatic expression of stress that results in skin findings. A number of primary psychodermatoses are reviewed, including trichotillomania, delusions of parasitosis, skin picking, and other self-induced skin lesions.
After a discussion of disorders with psychiatric implications, the cutaneous findings of other “outside disorders” including child abuse, graft-vs-host disease, and acquired immunodeficiency syndrome are reviewed. An algorithmic approach to psychodermatoses is summarized at the end of the chapter (see Fig. 11.24 ).
Localized skin conditions, which involve cosmetically important areas such as the head and neck, and chronic, widespread rashes such as atopic dermatitis, psoriasis, acne, and vitiligo, may be distressing enough to trigger psychophysiologic disorders. In this group of diseases, disfigurement can result in low self-esteem, social phobia, paranoia, and major depression.
Disfiguring lesions in infants and young children are a source of parental stress. However, if the lesions are treated before a critical period in psychologic development, long-term sequelae may be avoided. Although these critical periods are not well defined, many pediatricians agree that, if possible, treatment should be completed before patients begin school. For instance, large facial congenital pigmented nevi may be excised before kindergarten, and pulsed-dye laser treatment of port-wine stains may begin shortly after birth (see Fig 2.64, Fig 2.65, Fig 2.66 ).
Quality of life studies show that patients with eczema and psoriasis have significantly higher rates of anxiety, depression, and sleep disorders, as well as more absenteeism. Treatment is designed to eradicate the lesions that are most visible or symptomatic and minimize school absence. In adolescents, even mild acne may trigger a great deal of anxiety, and cystic acne is treated early and aggressively to avoid permanent scarring.
Periodic reassurance from the practitioner provides adequate support for many patients. Others may find participation in support-oriented groups, such as the National Vitiligo Foundation, National Alopecia Areata Foundation, and the Vascular Birthmarks Foundation, particularly helpful. However, when normal relationships with family and friends are disrupted, psychiatric consultation and counseling may be necessary.
In this category of psychodermatoses, the skin becomes the focus of a primary psychosis. In most cases, either no true dermatologic disorder is present or minor findings are misinterpreted by the patient in accordance with his or her underlying psychopathology. Although subtle symptoms may develop in childhood, most cases become manifest in adolescence or young adulthood.
Trichotillomania is a compulsive urge to pull out one’s own hair. It clinically looks like patchy hair loss that does not follow anatomic or physiologic landmarks. The scalp is most commonly affected, but other areas can be involved. On dermoscopy the most common findings are decreased hair density, broken hairs at different lengths, trichoptilosis (split ends), irregular coiled hairs, upright regrown hairs, and black dots showing perifollicular hemorrhages. Malakar and Mukherjee described a dermoscopy finding of a dark bulbar proximal tip with a linear stem of variable lengths looking like a burnt matchstick. Trauma and traction cause this finding.
Unlike innocent hair pulling, which occurs commonly in toddlers and preschoolers, children with trichotillomania demonstrate obsessive-compulsive symptoms.
The Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) describes trichotillomania as an impulse control disorder affecting 1.5–2% of the general population. In adults there is a female-to-male ratio of 4:1; however, in children, girls and boys are equally affected and severity is variable. Observational data show that one-third of affected children have comorbid psychiatric conditions including generalized anxiety, social phobia, major depression, substance-use disorders, attention-deficit/hyperactive disorder, and oppositional defiant disorder.
Trichotillomania differs from other obsessive-compulsive disorders (OCDs) as age of onset is usually early adolescence rather than late adolescence, and individuals with trichotillomania do not have intrusive thoughts like in other OCDs. There are often other repetitive motor symptoms such as skin picking and nail biting. Psychotherapy evidence supports cognitive behavioral therapy, focusing on habit-reversal training, where the emphasis is on replacing hair pulling with more desirable behaviors.
A glutamatergic agent, N-acetyl cysteine, has been found to reduce urges. Olanzapine has also been shown to be effective. There is no evidence that selective serotonin reuptake inhibitors (SSRIs) are beneficial. Trichotillomania is not self-limited and requires long-term psychiatric and medical therapy (see Fig. 8.24 ).
Delusions of parasitosis, the most common monosymptomatic hypochondriacal psychosis treated by dermatologists, occurs when an individual is convinced that the skin is infested with imaginary mites, worms, or insects. Cutaneous findings range from none to excoriations, lichenification, prurigo nodularis, and ulcerations, which are created by the patient attempting to dig out the parasites. Patients may also present with collections of scale, hair, and/or other debris presumably containing parasites ( Fig. 11.1 ). Other delusional disorders include bromosis (foul odor) and dysmorphosis (abnormal or ugly appearance).

These patients have little insight into their disease and usually refuse consultation with psychiatrists. Unfortunately, the prognosis is guarded, and symptoms may persist indefinitely. Small case studies of delusions of parasitosis showed symptom improvement with pimozide at a dose from 1 to 5 mg daily for 6 weeks before starting to taper and olanzapine at 5 mg daily for 10 weeks, sometimes increasing to 10 mg daily.
Concurrent medications may be beneficial, including anxiolytics, antidepressants, and corticosteroid creams. Aripiprazole, a third-generation antipsychotic, is another potentially safe and effective option.
Skin picking disorders and other body-focused repetitive behavior disorders (BFRBD) have been introduced in the DSM-5. These disorders can be expressed in multigenerational families and may have comorbid associations.
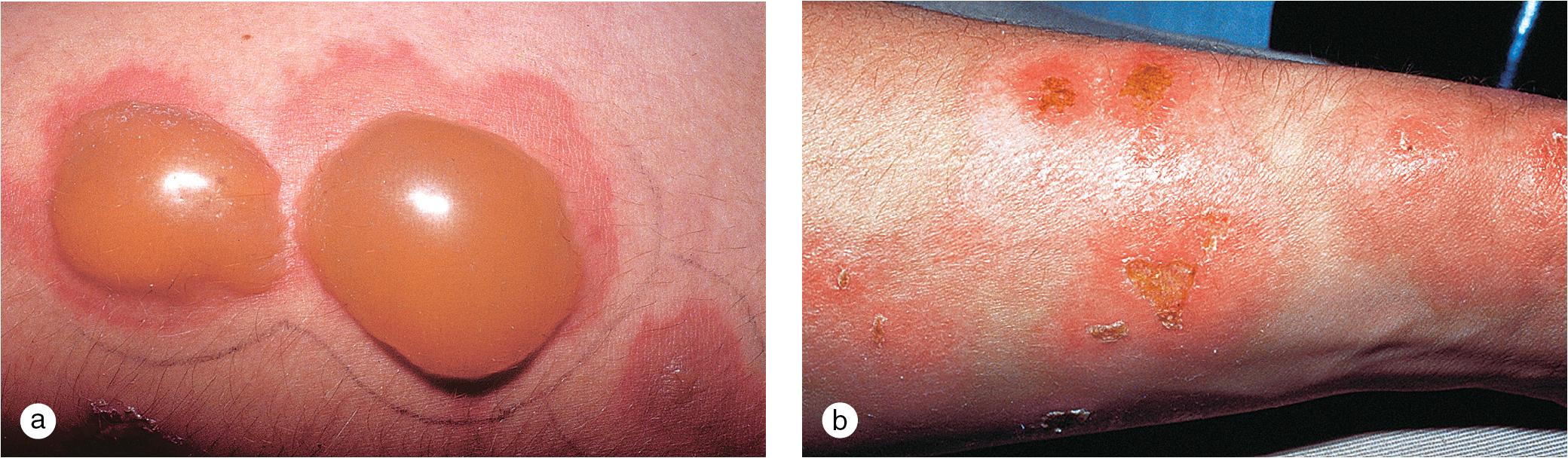
In acne excoriée and skin picking, variants of OCDs, patients pick and gouge trivial acne or other skin lesions on the face, arms, or hands, but often at multiple sites, resulting in erosions and ulcerations that may heal with scarring ( Fig. 11.2 ). Acne excoriée occurs most commonly in adolescents. This disorder is triggered by emotional states such as anxiety or boredom. There are two subgroups: those with primary acne and those with no primary lesions. Patients may attempt to stop picking, and acne treatment, when appropriate, is the first line of treatment. Cognitive behavioral therapy, habit reversal training, and N-acetyl cysteine have been shown to have good results. SSRIs and/or low-dose antipsychotics have also been used with variable responses.

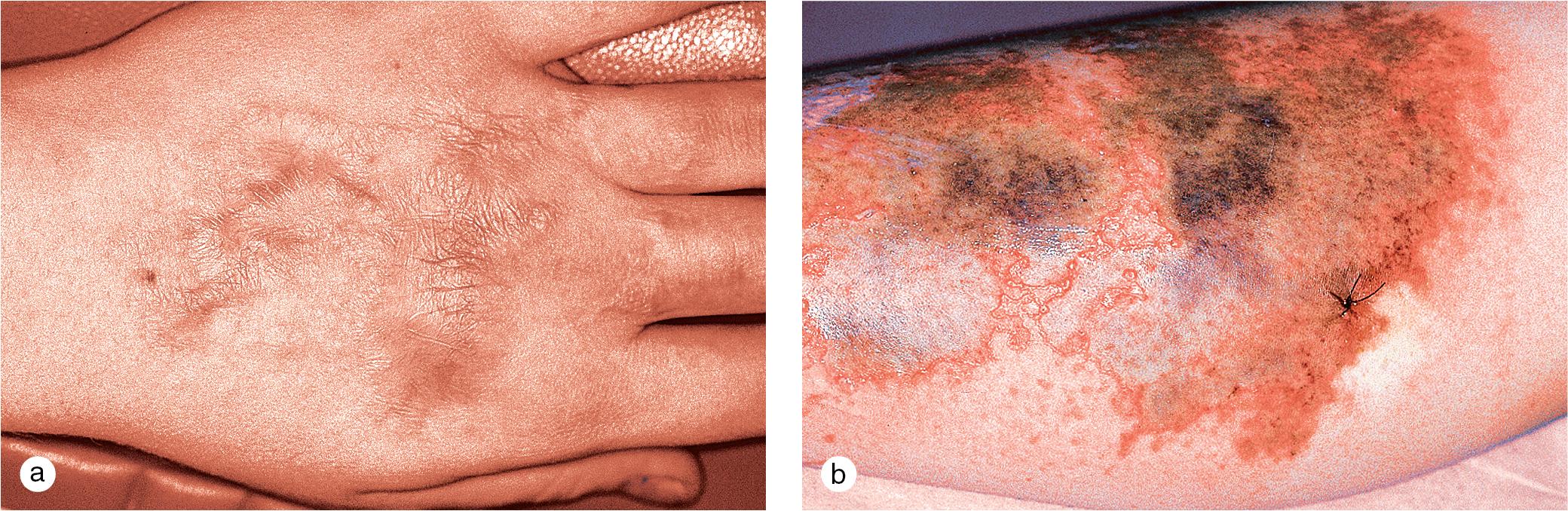
A subset of patients with self-induced skin lesions, often referred to as factitious disorders, usually adolescents, develop cutaneous findings such as coining, excoriations, and chemical burns in association with situational stress ( Figs. 11.3–11.5 ). Disordered family dynamics, sexual abuse, school phobia, lost love, and other acute or chronic psychosocial problems may result in this form of attention-seeking behavior. When this diagnosis is suspected, lesions may be covered with occlusive dressings for several weeks to see if healing occurs. When confronted, the patients usually admit to the self-injurious behavior. Counseling and improvement in the situation often result in an end to the lesions.

When patients develop bizarre symptoms with few or confusing clinical findings, a psychiatric source is often considered. However, careful attention to the course of symptoms and development of skin lesions may give a clue to the true dermatologic diagnosis.
Dermatitis herpetiformis (DH) is a good example of a pseudopsychodermatosis. In DH, persistent, intense pruritus and subsequent excoriations, which obliterate the primary vesiculobullous lesions, make diagnosis difficult. Unless DH is considered and confirmed by skin biopsy and/or immunofluorescence studies, the patient may be mistakenly referred to psychiatry for evaluation of “neurotic” excoriations. Scabies, folliculitis, urticaria, and other pruritic dermatoses may also be misdiagnosed as psychogenic pruritus.
Occasionally, children with temporal lobe seizures present with pseudo-delusions of parasitosis. Complaints of bizarre sensations in the skin also prompt a search for medication overdosage (e.g., diphenhydramine) or illicit drug exposure, or result in excoriations, ulcerations, or other skin findings ( Fig. 11.6 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here