Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Protozoa are responsible for many tropical diseases that not only affect large regions of the world but also can have different clinical presentations in the Old World versus the New World (e.g. leishmaniasis)
Protozoal infections can lead to significant morbidity in both immunocompromised hosts (e.g. toxoplasmosis) and immunocompetent individuals (e.g. Balamuthia spp.)
Worms (helminths) are common parasites with a worldwide distribution; cutaneous manifestations vary considerably, from pruritus ani to elephantiasis
Even helminthic diseases with a restricted geographic distribution, such as onchocerciasis and echinococcosis, may be observed in individuals from non-endemic areas due to immigration, tourism, disaster relief efforts or military service
▪ Old World cutaneous leishmaniasis: oriental sore, Delhi boil, Baghdad boil ▪ New World cutaneous and mucocutaneous leishmaniasis: American tegumentary leishmaniasis, chiclero ulcer (Mexico), uta and espundia (Peru), ulcera de Bauru (Brazil), bush or forest yaws, pian boi (Guyanas) ▪ Diffuse cutaneous leishmaniasis: anergic, lepromatous, or pseudolepromatous leishmaniasis ▪ Visceral leishmaniasis: kala-azar, Dumdum fever
Chronic parasitic (protozoan) disease in which organisms are found within phagolysosomes of mononuclear phagocytes
The clinical manifestations of leishmaniasis depend on the host's cell-mediated immune response and the species of Leishmania involved; clinical subtypes include cutaneous, disseminated cutaneous, diffuse cutaneous, mucocutaneous/mucosal, and visceral leishmaniasis
The most common cutaneous finding is a papule at the site of inoculation that classically evolves into an ulcer
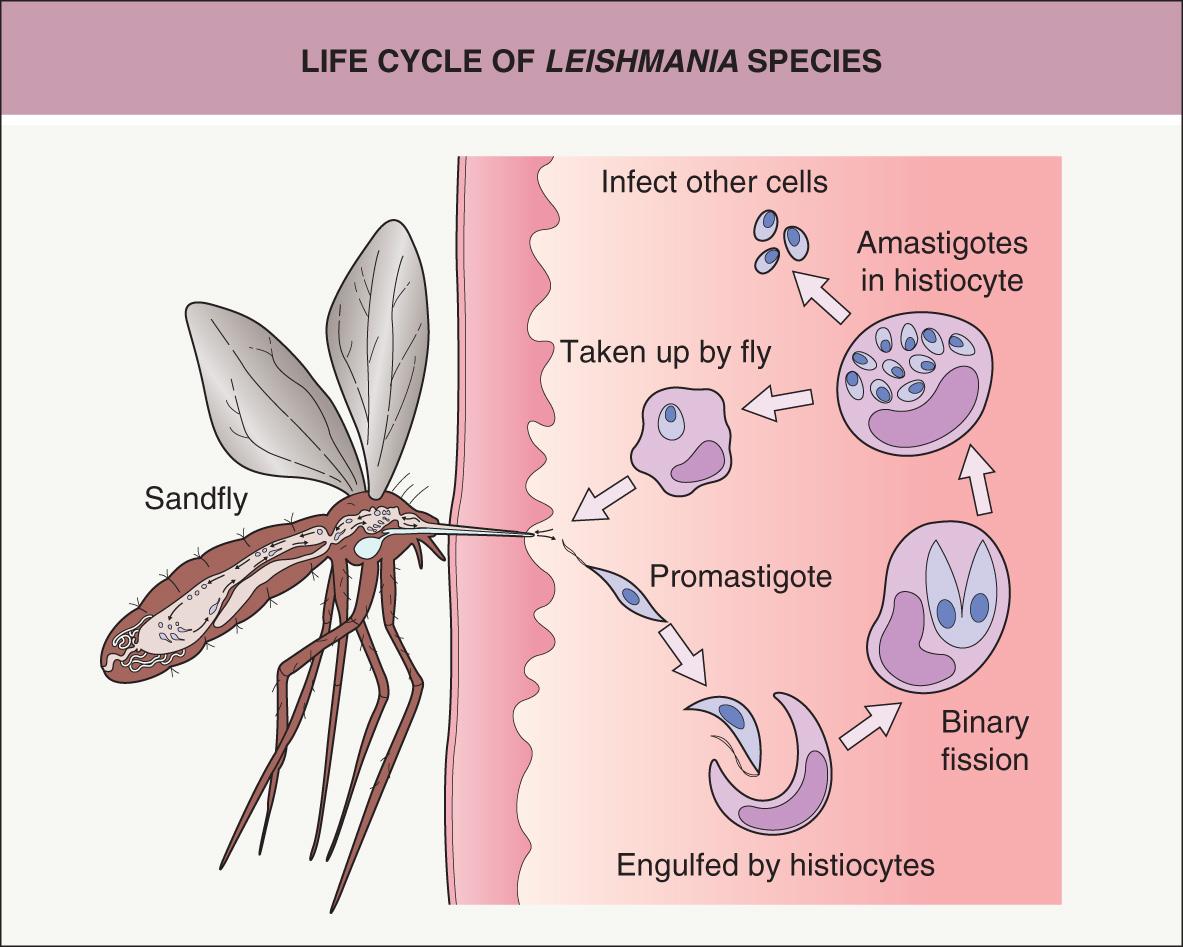
The vector is a sandfly infected with promastigotes
The disease has a worldwide distribution but is endemic in Latin America, the Mediterranean basin, and parts of Asia and Africa
Leishmaniasis encompasses a spectrum of chronic infections in humans and several animal species. It is caused by over 20 species of Leishmania ( Table 83.1 ), flagellated protozoans belonging to the order Kinetoplastidae. Transmission is via the bite of infected female sandflies from the genera Phlebotomus and Lutzomyia .
| EPIDEMIOLOGIC AND CLINICAL PATTERNS OF INFECTIONS WITH LEISHMANIA SPECIES | |||||
|---|---|---|---|---|---|
| Complex | Major species | Major reservoirs | Major geographic distribution | Clinical patterns (in addition to cutaneous) | Clinical forms of the cutaneous pattern |
| Leishmania donovani | L. donovani | Humans | Sudan, Kenya, Tanzania, India, Bangladesh | Visceral, PKD , mucosal (rare) | (Uncommon) |
| L. infantum | Dogs, foxes | Mediterranean region | Visceral (favors children) , PKD * , mucosal † (rare) | Favors children (uncommon) | |
| L. infantum chagasi ** | Dogs, foxes, opossums | Central and South America | |||
| Leishmania tropica | L. major | Rodents | Arid areas of Africa (north and south of the Sahara), Middle East and Central Asia | Mucosal (rare) | Old World zoonotic/rural (moist, early ulcerative with rapid course), recidivans (rare), lupoid (rare) |
| L. tropica | Humans, dogs | Eastern Mediterranean region, Middle East, Central Asia | Visceral (rare), mucosal (rare) | Old World anthroponotic/urban (dry, late ulcerative with chronic course), recidivans, lupoid | |
| L. aethiopica | Hyraxes | Ethiopia, Kenya, Yemen | Diffuse cutaneous, mucocutaneous | Dry/late ulcerative or moist/early ulcerative | |
| Leishmania mexicana | L. mexicana | Forest rodents | Mexico, Central America | Diffuse cutaneous (rare) | New World Variants include ulcerative, plaque-like, pustular, impetigo-like, erysipeloid, sarcoidosis-like, papulotuberous, verrucous, sporotrichoid, eczematous |
| L. amazonensis | Forest rodents | South America | Diffuse cutaneous , mucocutaneous, visceral (rare), PKD (rare) | ||
| L. venezuelensis, pifanoi, garnhami | Unknown | Venezuela | Diffuse cutaneous (rare) | ||
| Leishmania (Viannia) braziliensis | L. braziliensis | Forest rodents | Central and South America | Mucocutaneous , visceral † | |
| L. guyanensis | Sloths, anteaters | Guyana, Brazil | Mucocutaneous | ||
| L. panamensis | Sloths | Panama, Costa Rica, Colombia | Mucocutaneous | ||
| L. peruviana | Dogs | Peru, Argentina | |||
* Rare/controversial; reported in children and in HIV-infected adults following antiretroviral therapy.
** L. infantum subspecies in the New World; previously known as L. chagasi .
The disease has a worldwide distribution, affecting millions of people in South America, the Mediterranean basin, and parts of Asia and Africa ( Figs 83.1 & 83.2 ). There are four major clinical patterns: (1) cutaneous, which is restricted to the skin and is seen more often in the Old World; (2) mucocutaneous, which affects both the skin and mucosal surfaces and occurs almost exclusively in the New World; (3) diffuse cutaneous, which occurs mainly in the New World; and (4) visceral, which affects the organs of the mononuclear phagocyte system, e.g. liver, spleen .
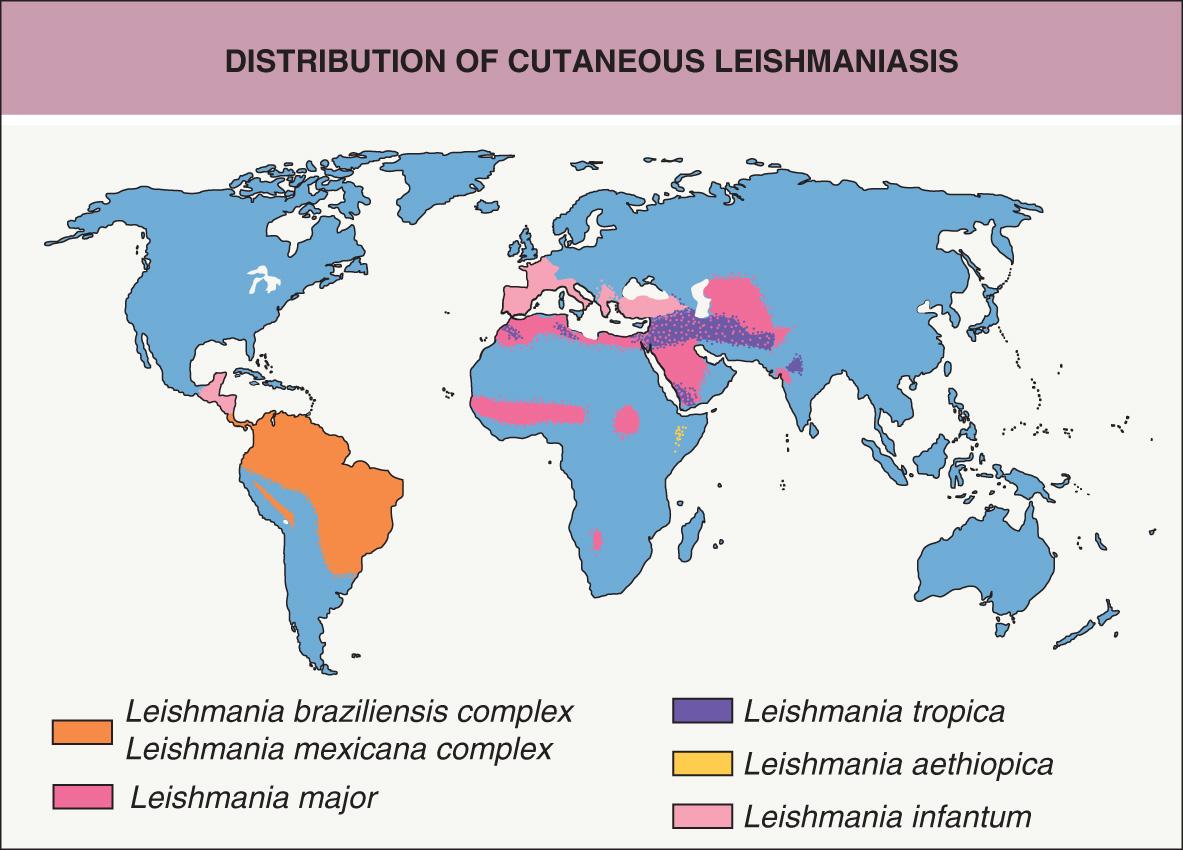
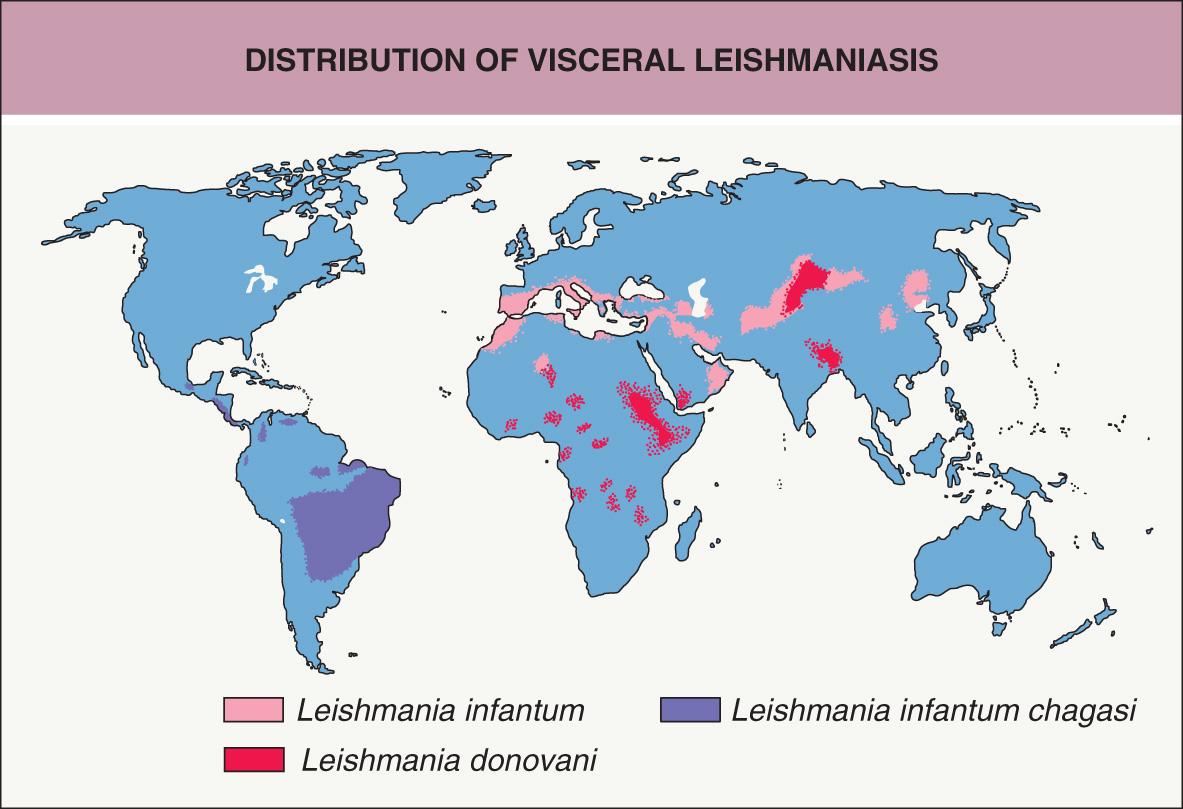
Worldwide, there are approximately 2 million new cases of leishmaniasis annually, with cutaneous or mucocutaneous disease in >75% of affected individuals; it is estimated that 12 million people are currently infected . Over 90% of cutaneous infections with Leishmania occur in the Middle East (Afghanistan, Algeria, Iran, Iraq, Saudi Arabia, Syria) and South America (Brazil, Peru, Colombia) ( Table 83.2 ), but the disease is also found in the Mediterranean basin, sub-Saharan Africa, Central Asia, and India (see Fig. 83.1 ). South-central Texas is the only endemic area for cutaneous leishmaniasis in the US; most infections diagnosed in the US are acquired outside of the country . Mucocutaneous leishmaniasis is endemic in several countries in Central and South America. Although the visceral form of leishmaniasis has a worldwide distribution, it is seen most frequently in Africa and Asia .
| COUNTRIES WITH THE HIGHEST INCIDENCE OF LEISHMANIASIS | |
|---|---|
| Old World cutaneous leishmaniasis | Afghanistan, Algeria, Iran, Iraq, Saudi Arabia, Syria |
| New World cutaneous leishmaniasis | Brazil, Peru, Colombia |
| Mucocutaneous/mucosal leishmaniasis | Bolivia, Brazil, Peru |
| Visceral leishmaniasis | Brazil, Ethiopia, India, Kenya, Somalia, South Sudan, Sudan. |
Old World cutaneous leishmaniasis is usually due to L. major or L. tropica , and less often L. infantum (Europe) or L. aethiopica (Ethiopia and Kenya) (see Table 83.1 ). In the New World, cutaneous leishmaniasis is caused primarily by subspecies of L. mexicana and the L. braziliensis complex, whereas mucocutaneous/mucosal disease is associated with the latter organisms. Diffuse cutaneous leishmaniasis is most commonly associated with L. amazonensis . Infections with L. donovani (e.g. India, Bangladesh, the Sudan) and L. infantum (e.g. Europe, especially in the setting of HIV infection) as well as the subspecies L. infantum chagasi (e.g. Central and South America; previously known as L. chagasi ) are the major causes of visceral leishmaniasis ( Table 83.3 ). The species of Leishmania can also vary within a particular geographic region. For example, in the Middle East, L. major is found in rural areas where the primary animal reservoirs are desert rodents, whereas L. tropica is endemic in urban areas .
| EPIDEMIOLOGY AND CLINICAL PATTERNS OF VISCERAL LEISHMANIASIS | ||
|---|---|---|
| Type of disease | Major species | Major geographic distribution |
| Kala-azar (60% 10–20 years of age) |
Leishmania donovani | India, China (north of Yangtze River), Kenya, Sudan |
| Infantile kala-azar (90% <10 years of age) |
L. infantum | Central Asia, China, Iraq, France, Italy, Egypt, elsewhere in the Mediterranean basin, Saudi Arabia |
| L. infantum chagasi | Brazil, Colombia, Venezuela, Central America, Mexico | |
| Oronasal kala-azar | L. infantum * | France |
| Post-kala-azar dermal leishmaniasis | L. donovani L. infantum † L. amazonensis |
India, China, Kenya Mediterranean basin, South America |
| Atypical kala-azar complex (typically in adults) |
L. tropica L. amazonensis L. braziliensis * |
Northeast Saudi Arabia South America South and Central America |
* Especially in immunocompromised hosts.
† Controversial (see Table 83.1 ).
Canine and rodent species act as the main reservoirs for Leishmania (see Table 83.1 ). Transmission between these species (as well as to humans) is via sandflies, primarily of the genera Phlebotomus (Old World) and Lutzomyia (New World). Human-to-human spread of L. tropica can also occur. In general, humans contract leishmaniasis as accidental hosts when they intrude into the sandfly's habitat. Overall, the disease is seen most commonly in men between 20 and 40 years of age, but Old World cutaneous leishmaniasis occurs more often in children .
Leishmania spp. are obligate intracellular parasites that exist in two forms: the promastigote and the amastigote. In the gut of the sandfly, the organisms multiply as extracellular flagellated promastigotes. Following migration to the proboscis, the parasites are inoculated (in the promastigote form) via the sandfly bite. Once inoculated into the skin, the parasites are rapidly engulfed by the host's mononuclear phagocytes, where they transform into amastigotes and multiply via binary fission ( Fig. 83.3 ). The incubation time from infection until the first clinical manifestation can vary from ≤2 weeks for cutaneous lesions (typically several weeks to 2 months) to >2 years for mucocutaneous lesions or visceral involvement (typically 3 to 9 months) .
The clinical manifestations of leishmaniasis depend on the species of Leishmania (see Table 83.1 ), the host’s cell-mediated response, and the ability of the parasite to evade host defense mechanisms . A robust Th1 response with production of interleukin-2 (IL-2) and interferon-γ (IFN-γ) is associated with quicker resolution, whereas a lack of a Th1 response and/or the development of a Th2-type response with production of IL-4 and IL-10 is associated with disease progression . Depending on the type of immune response, l -arginine metabolism within infected macrophages occurs via two alternative pathways: (1) Th2 cytokines promote its catabolism by arginase to produce l -ornithine, which favors parasitic growth; or (2) Th1 cytokines promote nitric oxide synthase-induced generation of l -citrulline plus nitric oxide, and the latter increases host resistance via NLRP3 (NLR family pyrin domain-containing-3) inflammasome-derived IL-1β . Resistance of L. amazonensis and L. braziliensis promastigotes to nitric oxide in vitro correlates with poorer clinical outcomes. Mucocutaneous disease is associated with the infection of Leishmania organisms with Leishmania RNA virus-1 (LRV1); this virus is recognized by human Toll-like receptor 3, leading to a proinflammatory cascade that subverts the immune response to Leishmania , and allows disease progression . L. donovani has been shown to induce epigenetic changes via macrophage DNA methylation that down-regulate host defense mechanisms, allowing parasitic replication and survival . Human genetic factors include HLA variants that contribute to leishmaniasis risk and IL2RA variants that reduce IL-2-dependent responses and thereby increase susceptibility to cutaneous and visceral leishmaniasis .
IFN-γ is the most potent cytokine involved in the induction of activity against organisms residing within macrophage phagolysosomes. It leads to the production of oxygen species and activates naive CD4 + cells to become Th1 cells (see Fig. 4.10 ). The latter differentiation process is aided by IL-12, which stimulates natural killer (NK) cells to produce IFN-γ . Tumor necrosis factor (TNF) produced by macrophages and NK cells amplifies the IFN-γ driven macrophage activation . Consequently, use of TNF inhibitors increases the risk of developing leishmaniasis, especially the visceral form. Recent studies have also highlighted the role of TNF-dependent IL-32γ in stimulating the production of proinflammatory cytokines and microbicidal molecules in human macrophages infected with New World Leishmania spp. . In addition, Th17 cells can potentially contribute to both host resistance and tissue damage in patients with leishmaniasis.
Animals that have recovered from L. tropica or L. donovani infections acquire immunity against reinfection from the same species of Leishmania , but not against other species. Similarly, humans with New World cutaneous leishmaniasis have been inoculated successfully with L. tropica . However, it has been reported that surviving an episode of visceral leishmaniasis confers lifelong immunity against all types of leishmaniasis.
Cutaneous leishmaniasis is divided into two subsets based on the geographic region where the infection is acquired: Old World and New World. These two groups differ with regard to the causative organisms, vectors, reservoirs, clinical presentation, and prognosis . Both Old World and New World cutaneous leishmaniasis usually begin as a small, well-circumscribed papule at the inoculation site. This lesion may slowly enlarge over several weeks into a nodule or plaque and then become ulcerated or verrucous ( Figs 83.4 & 83.5 ). Exposed sites such as the face, neck, arms, and legs are most commonly involved. For example, the chiclero ulcer results from infection on the ear in forest workers who collect gum from the chicle tree in Mexico and Central America. The lesions of leishmaniasis are often solitary but may be multiple, with the formation of satellites or lymphatic spread (sporotrichoid pattern; Fig. 83.6 ). The majority of acute cutaneous infections resolve spontaneously within several months with scarring (cicatricial stage; Fig. 83.7 ), but a minority become chronic or disseminated.
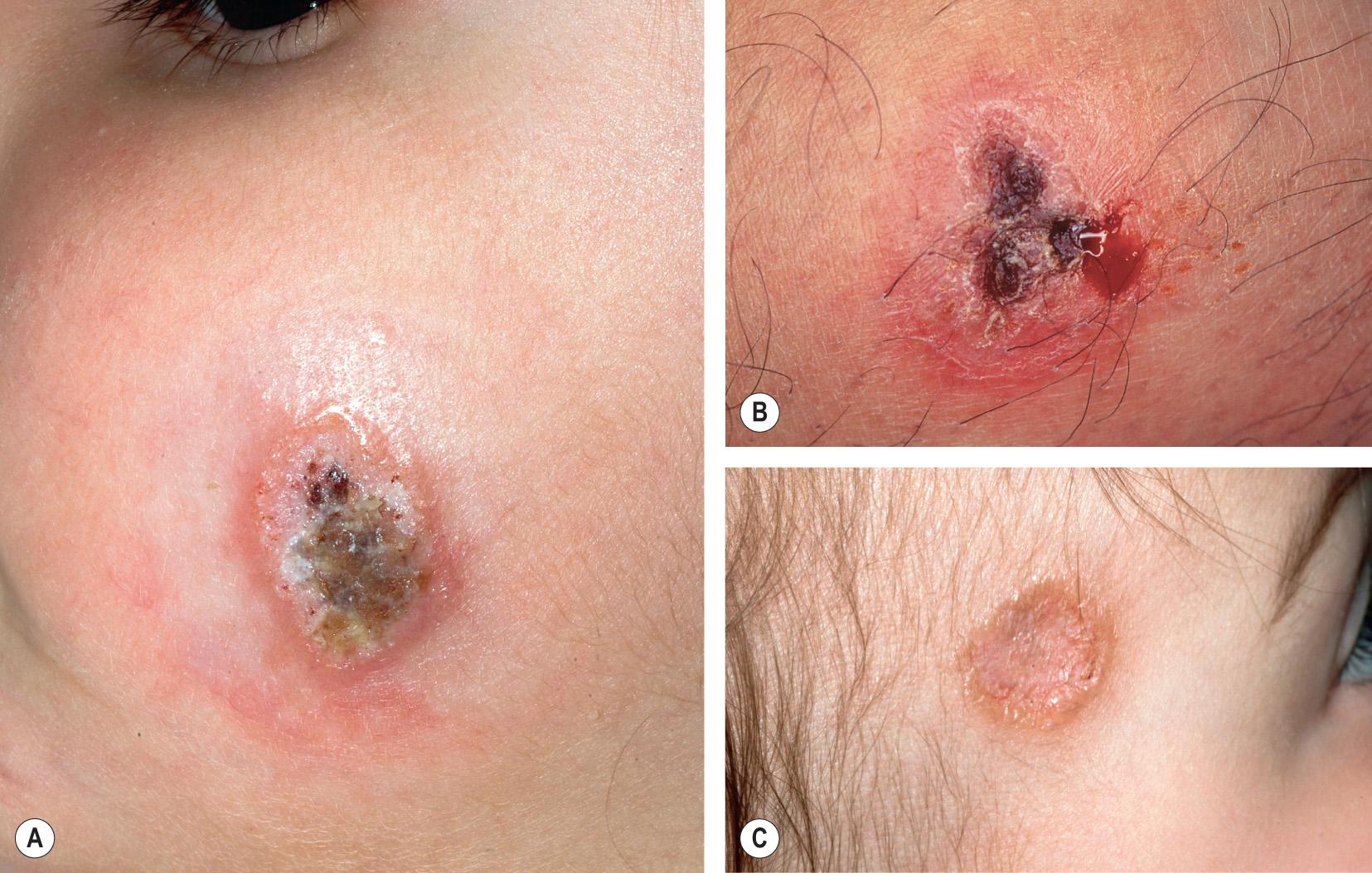



Several clinical forms of Old World cutaneous leishmaniasis have been described, including zoonotic, anthroponotic, recidivans, and lupoid leishmaniasis. Zoonotic cutaneous leishmaniasis (rural, moist, or early ulcerative form) usually has a mild, rapid course and is caused by L. major . Anthroponotic cutaneous leishmaniasis (urban, dry, or late ulcerative form), has a more chronic course and is caused by L. tropica . Leishmaniasis recidivans is a chronic, destructive form that is characterized by recurrence at the site of an original ulcer, generally within 2 years and often at the edge of the scar . Anthroponotic or, less frequently, zoonotic cutaneous leishmaniasis occasionally develops into chronic lupoid leishmaniasis, which clinically and histologically (epithelioid granulomas surrounded by lymphocytes) resembles the lupus vulgaris form of cutaneous tuberculosis. The amastigotes are few in number and difficult to find in lupoid leishmaniasis, making establishment of the diagnosis more challenging.
New World cutaneous leishmaniasis has a wide clinical spectrum, including plaque-like, sporotrichoid, pustular, impetigo-like, eczematoid, sarcoid-like, lupoid, erysipeloid, papulotuberous, verrucous , disseminated, and diffuse presentations.
Disseminated cutaneous leishmaniasis , which most often results from L. braziliensis or L. amazonensis infection, is characterized by multiple (10 to >300) secondary lesions, either in proximity to or distant from the primary site. The lesions resemble those of classic cutaneous leishmaniasis, including papules and small nodules that may have an acneiform appearance, and ulceration is common ( Fig. 83.8B ). Up to 25% of affected individuals have concomitant mucosal disease, and patients may have systemic symptoms such as fever and malaise. Disseminated skin disease most likely results from early hematologic spread, and it is associated with decreased production of IFN-γ and TNF .
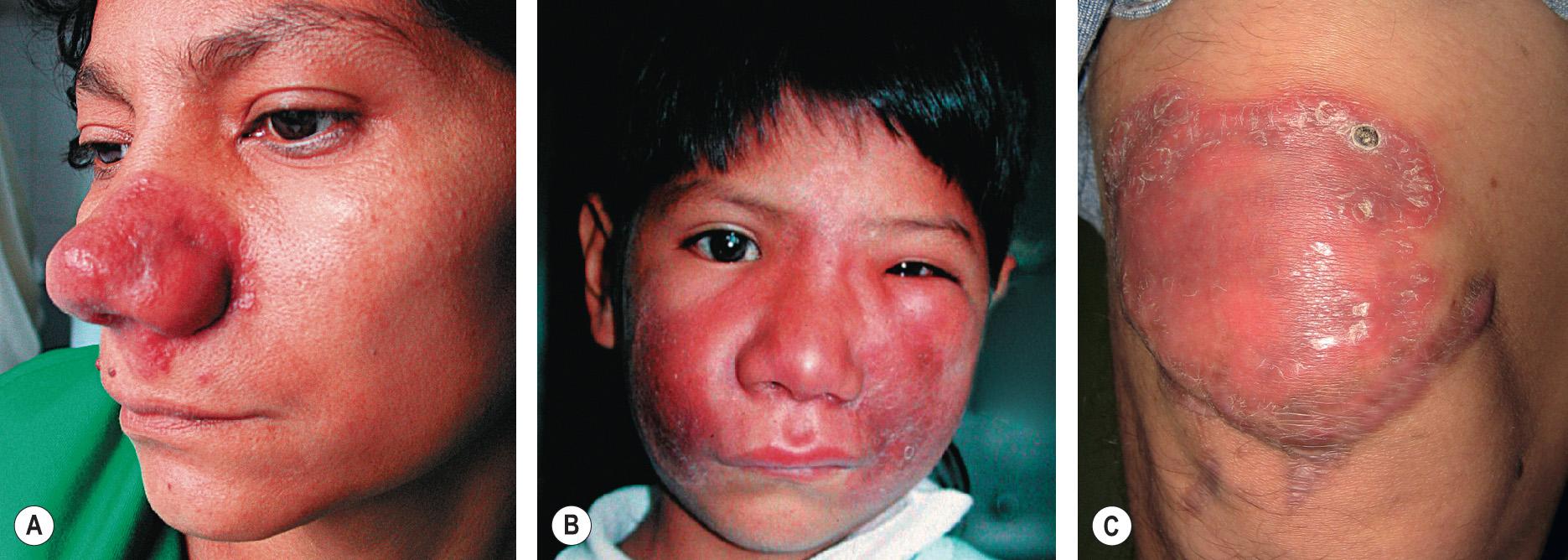
Diffuse cutaneous leishmaniasis is a rare presentation that develops in the setting of reduced cell-mediated immunity, analogous to lepromatous leprosy. L. aethiopica (in Africa) and L. amazonensis (in the Americas) are the most common pathogens (see Table 83.1 ). Multiple nodular and keloid-like lesions on the face and limbs are usually observed ( Fig. 83.8A ); ulceration is uncommon but occasionally occurs secondary to trauma. Nasal infiltration and mucosal ulceration may develop due to spread from nearby skin lesions, but destruction of the nasal septum is rare. There may also be laryngeal and pharyngeal involvement .

After a variable time period ranging from a few months to more than 20 years, mucocutaneous/mucosal disease develops in some patients infected with Leishmania spp. in the Viannia subgenus (known as the L. braziliensis complex), most commonly L. braziliensis and occasionally L. panamensis , L. guyanensis , or hybrid genotypes . Mucosal lesions range from edema of the lips and nose to perforation of the nasal septum or (less often) the laryngeal cartilage or palate. Infiltration and/or ulceration of the mucosal surfaces of the nose, lips, and oropharynx are typical features ( Figs 83.9 & 83.10 ); ocular or genital involvement is rare. In some patients, there is extensive loss of tissue in both the mouth and nose, causing a characteristic “tapir face” known as espundia. Hoarseness may result from vocal cord involvement .


Visceral leishmaniasis, or kala-azar, occurs when the parasite spreads to the bone marrow, spleen, and liver . It is primarily caused by L. donovani in adults and L. infantum or L. chagasi in children. The incubation period ranges from 1 to 36 months. Fever, wasting, cough, lymphadenopathy, and hepatosplenomegaly are the most common systemic findings ( Table 83.4 ). There may be an abrupt onset or slow progression, and fever may be continuous or intermittent. Additional complications include enteritis, oronasal or gastrointestinal hemorrhage, pneumonia, and nephritis, which may lead to death . Cutaneous manifestations may be disease-specific papules, nodules, or ulcers at infected sites as well as nonspecific findings such as purpura, hyperpigmentation, xerosis, and kwashiorkor-like hair discoloration.
| SYSTEMIC FEATURES OF VISCERAL LEISHMANIASIS ( L. DONOVANI ) | |
|---|---|
| Clinical features | Proportion affected (%) |
| Age <9 years | 20 ( L. infantum and L. chagasi more commonly affect children and infants) |
| Age <15 years | 45 |
| Fever | 85–100 |
| Wasting | 70–100 |
| Loss of appetite | 60–75 |
| Cough | 70–85 |
| Epistaxis | 45–55 |
| Diarrhea | 25–55 |
| Vomiting | 2–35 |
| Splenomegaly | 90 (adults); >95 (children) |
| Hepatomegaly | 55–65 |
| Lymphadenopathy | 55–85 (uncommon outside of Africa) |
| Jaundice | 2–7 |
| Edema | 2–7 |
| Laboratory findings | |
| Globulin >30 g/l | 95 |
| Albumin <30 g/l | 90 |
| Anemia | 60–90 |
| Leukopenia | 85 |
| Thrombocytopenia | 75 |
| Elevated bilirubin | 15 |
| Elevated liver transaminases | 20 |
| Elevated alkaline phosphatase | 40 |
| Positive Leishmania serology | 95 |
| Parasitologically proven | 95 |
Post-kala-azar dermal leishmaniasis develops as a sequela of untreated or treated visceral leishmaniasis ( Fig. 83.11 ). This form of cutaneous leishmaniasis is most commonly seen in Sudan and India, where it occurs in 50% and 10% of patients cured of visceral leishmaniasis, respectively . Onset may be up to 20 years after treatment . Skin findings include hypopigmented macules, malar erythema, skin-colored nodules, and verrucous papules .

Co-infection of HIV and leishmaniasis can alter the progression and presentation of leishmaniasis, especially the visceral form (see Ch. 78 ). HIV infection increases the risk of developing visceral leishmaniasis 100- to over 2000-fold. Co-infection often results in an atypical clinical presentation, reduced therapeutic response, and increased mortality. Chronic immune activation from the Leishmania infection may lead to increased HIV load and accelerated progression of AIDS, while the immunosuppressed state from the HIV infection creates an ideal environment for parasitic growth . Co-infection with HIV is thought to be present in 2% to >10% of patients with visceral leishmaniasis who live in Leishmania -endemic areas .
Histologically, cutaneous lesions typically show ulceration, pseudoepitheliomatous hyperplasia, and a mixed inflammatory infiltrate composed of histiocytes, lymphocytes, plasma cells, and neutrophils. Amastigotes present within dermal macrophages, especially those in the papillary dermis ( Fig. 83.12 ), are evident in ∼50% of skin biopsies. Over time, lesions develop an increasing number of giant cells and fewer parasites; in longstanding cutaneous leishmaniasis, tuberculoid granulomas with caseation necrosis may be observed. In the cicatricial stage, the epidermis becomes flattened and hyperpigmented in areas with dermal fibrosis. Identical changes are seen in mucosal lesions. In diffuse cutaneous leishmaniasis, numerous amastigotes are present within foamy histiocytes; in contrast, the disseminated form features a primarily lymphoplasmacytic infiltrate with few amastigotes. The parasite can be detected in the lymph nodes, bone marrow, and spleen in patients with visceral leishmaniasis.
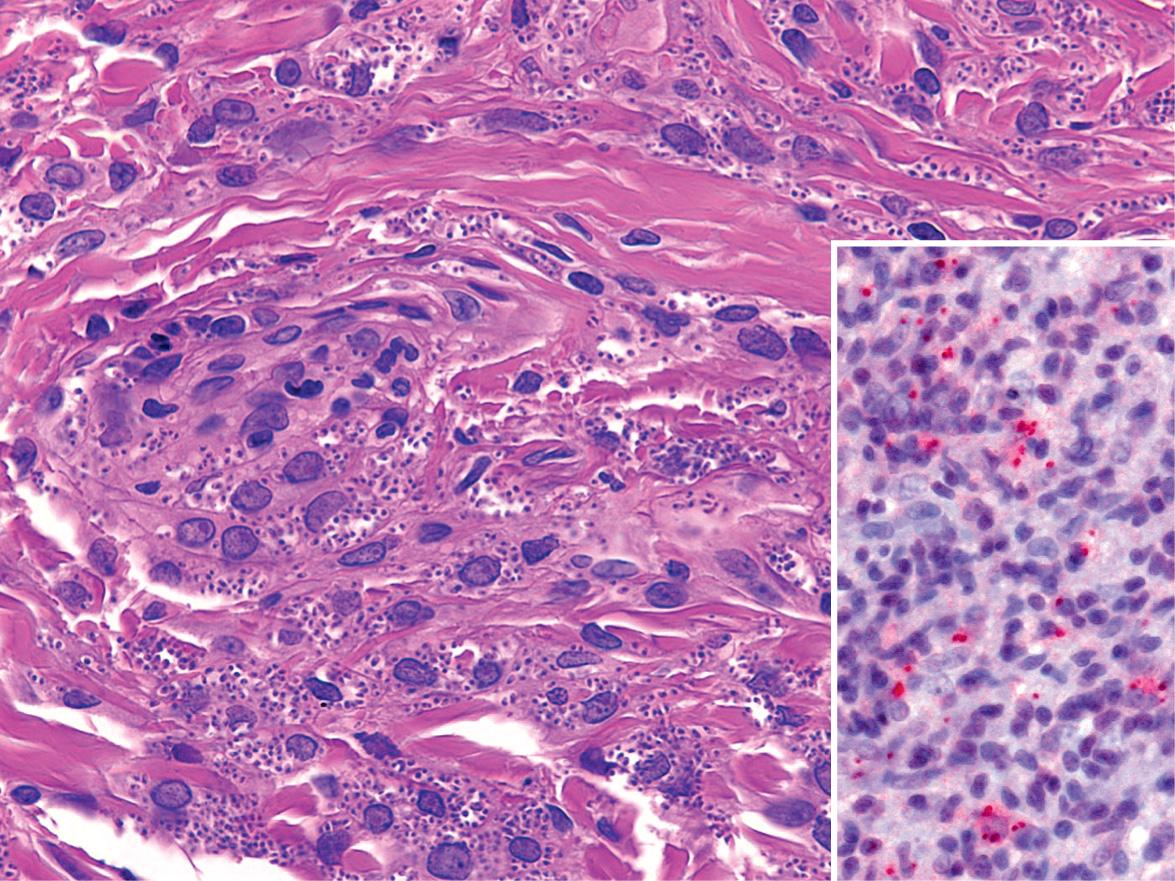
The diagnosis of cutaneous leishmaniasis can be confirmed by demonstrating the presence of amastigotes in dermal macrophages within skin biopsy specimens, tissue impression smears (touch preparations), and smears obtained by dermal scraping or needle aspiration of skin lesions . Although routine hematoxylin and eosin staining allows the visualization of the amastigotes, Giemsa, Wright, or Feulgen stains can help to identify the organisms in smears and tissue: the cytoplasm appears blue, the nucleus pink and the kinetoplast a deep red ; CD1a immunostaining can also highlight the amastigotes (see Fig. 83.12 ). The edge of a relatively new ulcer is the location of choice for obtaining dermal scrapings, a biopsy specimen, or a needle aspirate; the latter two types of samples may be used for culture and polymerase chain reaction (PCR)-based assays (see below) .
In longer-standing lesions of leishmaniasis, parasites may be scarce. In this context, the delayed skin reaction test (Montenegro skin test or Leishman reaction), which uses leishmanial antigens to induce a cell-mediated response, has traditionally been an important diagnostic tool. A phenolated suspension of killed promastigotes is injected intradermally, usually on the volar aspect of the forearm. The test is considered positive if a papule >5 mm in diameter forms at the site of inoculation after 48–72 hours (see Fig. 83.5 ) . It is positive in up to 90% of patients with cutaneous and mucocutaneous leishmaniasis of over 3 months’ duration and is invariably negative in patients with diffuse cutaneous (anergic) leishmaniasis . However, this test (which is not approved by the US Food and Drug Administration [FDA]) cannot distinguish between past and present infections, so it is most useful in patients who do not reside in areas where leishmaniasis is endemic; positivity develops while the skin lesions are still active, and the test remains positive long after spontaneous cure. The test is usually negative during the febrile phase of visceral leishmaniasis, but it often becomes positive after cure.
For culturing Leishmania , specialized media are required, e.g. Nicolle–Novy–MacNeal (NNM) media or chick embryo media. Cultures are positive in approximately 40% of cases. Serologic and immunologic tests are also available, e.g. indirect immunofluorescence, ELISA, immunoprecipitation, and isoenzyme electrophoresis. Serologic testing is most useful for visceral and occasionally mucocutaneous disease, although it is not specific due to cross-reactivity (e.g. with Chagas disease antibodies) . PCR-based methods represent the most sensitive and specific diagnostic tests, and their availability is increasing . An FDA-approved real-time PCR assay for the diagnosis of leishmaniasis is available through the Centers for Disease Control and Prevention (CDC) .
The differential diagnosis of cutaneous leishmaniasis includes persistent arthropod bite reaction, basal cell carcinoma, tuberculosis, non-tuberculous mycobacterial infections, and subcutaneous mycoses; other infectious causes of lesions in a lymphocutaneous pattern are listed in Table 77.17 . Mucocutaneous leishmaniasis can resemble paracoccidioidomycosis and tertiary syphilis. In addition, granulomatosis with polyangiitis (formerly Wegener granulomatosis) and angiocentric NK/T-cell lymphoma should be considered when ulcerative mucocutaneous lesions affect the central part of the face. Cocaine-induced nasal ulcerations can also mimic the mucosal involvement of leishmaniasis. Histologic examination allows distinction among these diseases . The histologic differential diagnosis includes other infections characterized by parasitized macrophages (see Table 77.18 ) and even neoplasms such as squamous cell carcinoma when pseudoepitheliomatous hyperplasia is present. The morphology and distribution of diffuse cutaneous leishmaniasis can mimic lepromatous leprosy; however, in the former the eyebrows are spared and the lesions are usually less infiltrative .
Factors to consider in the treatment of leishmaniasis include the region of the world in which the infection was acquired, the species of Leishmania, the site(s) and severity of the infection, and host factors such as immune status and age. The benefit of therapy needs to be balanced with the goal of minimizing drug toxicity. Without treatment, Old World cutaneous leishmaniasis typically resolves within 2–4 months ( L. major ) or 6–15 months ( L. tropica ). Indications for systemic treatment of Old World cutaneous leishmaniasis include (1) an immunocompromised host; (2) >4 lesions of substantial size (e.g. >1 cm) or individual lesion(s) measuring ≥5 cm; (3) markedly enlarged regional lymph nodes; and (4) involvement of the mucosa, face, ears, genitalia, fingers, toes, or skin overlying a joint . Local therapy or, if the lesions are healing spontaneously within 6 months, observation are options for patients who do not meet these criteria.
New World cutaneous leishmaniasis caused by L. mexicana resolves within 3 months in >75% of cases. In contrast, cutaneous disease caused by L. braziliensis and L. panamensis spontaneously heals in less than 10% and 35% of cases, respectively. Therefore, systemic treatment is indicated when L. braziliensis complex infection is suspected in order to accelerate healing, decrease scarring (especially in cosmetically sensitive sites), and prevent dissemination, relapse, or the development of mucosal disease .
Parenteral pentavalent antimonials and miltefosine are first-line systemic treatments for cutaneous and mucocutaneous/mucosal leishmaniasis, whereas liposomal amphotericin B is the treatment of choice for visceral leishmaniasis . Table 83.5 summarizes treatment regimens for cutaneous and mucocutaneous/mucosal leishmaniasis . Table 83.6 lists frequent adverse reactions to drugs used for the treatment of leishmaniasis. Additional interventions that have shown some efficacy for cutaneous and (in combination with other agents) mucocutaneous/mucosal leishmaniasis include heat therapy , cryotherapy, photodynamic therapy, and oral allopurinol.
| TREATMENT RECOMMENDATIONS FOR LEISHMANIASIS | ||
|---|---|---|
| Cutaneous leishmaniasis | ||
| Drugs of choice | Sodium stibogluconate * | 20 mg/kg/day IV or IM × 20 days Various intralesional regimens, e.g. 0.2–5 ml (5 sites/lesion intradermally for 0.1 ml/cm 2 until blanched) every 3–21 days for 5–8 sessions or until healing |
| Meglumine antimonate * | ||
| Miltefosine ** | 50 mg BID if weight is 30–44 kg and TID if weight is ≥45 kg × 28 days | |
| Alternatives | Paromomycin 15% and MBCL 12% ointment | Topically BID × 10 days, wait 10days, then repeat |
| Paromomycin 15% and gentamicin 0.5% cream | Topically daily for 20 days | |
| Pentamidine | 3–4 mg/kg IV or IM every other day × 3–4 doses | |
| Fluconazole † | 200 mg/day or 6–8 mg/kg/day PO × 6 weeks | |
| Liposomal amphotericin B † | 3 mg/kg/day IV on days 1–5 + 10 or days 1–7 | |
| Amphotericin B deoxycholate | 0.5–1 mg/kg IV daily or every other day for a total dose of 15–30 mg/kg | |
| Mucocutaneous leishmaniasis | ||
| Drugs of choice | Sodium stibogluconate * | 20 mg/kg/day IV or IM × 28 days |
| Meglumine antimonate * | ||
| Liposomal amphotericin B | ∼3 mg/kg/day IV for a total dose of ∼20–60 mg/kg | |
| Amphotericin B deoxycholate | 0.5–1 mg/kg IV daily or every other day for a total dose of ∼20–45 mg/kg | |
| Miltefosine ** | 50 mg BID if weight is 30–44 kg and TID if weight is ≥45 kg × 28 days | |
| Alternative | Pentamidine | 2–4 mg/kg IV or IM every other day or 3 times per week for ≥15 doses |
* Doses refer to mg of pentavalent antimony – 100 mg/ml for sodium stibogluconate (Pentostam®), 85 mg/ml for meglumine antimonate (Glucantime®).
** FDA-approved for the treatment of cutaneous and mucosal leishmaniasis due to L. braziliensis , L. guyanensis , and L. panamensis in patients ≥12 years of age.
† Limited evidence of efficacy; other azole antifungals that have been utilized (with variable results) include ketoconzaole (600 mg/day or 10 mg/kg/day PO × 4 weeks) and itraconzaole (7 mg/kg/day PO × 3 weeks).
| ADVERSE SIDE EFFECTS OF THE MOST COMMONLY USED DRUGS FOR LEISHMANIASIS | ||
|---|---|---|
| Drug | Side effect | Incidence |
| Intralesional pentavalent antimony | Localized pain, erythema, edema | 25–50% |
| Parenteral pentavalent antimony | Raised amylase/lipase and/or LFTs | >50% |
| Myalgia, arthralgia | 25–50% | |
| Abdominal pain/nausea | 25–50% | |
| Thrombocytopenia/leukopenia | <25% | |
| ECG changes or cardiotoxicity | <25% | |
| Miltefosine | Motion sickness | >50% |
| Nausea, vomiting and diarrhea | 25–50% | |
| Elevated serum creatinine | 25–50% | |
| Mildly elevated LFTs | <25% | |
| Teratogenicity * | >50% | |
| Pentamidine | Nausea, vomiting and diarrhea | >50% |
| Hyperglycemia | <25% | |
| Cardiotoxicity | <25% | |
* Contraindicated during pregnancy. Contraception is required during administration and for 2 months after the drug is discontinued.
Drugs or vaccines that completely prevent leishmanial infection have not yet been developed. The best form of protection is to avoid the bite of the sandfly and eliminate animal reservoirs. Personal protection includes applying DEET-based repellants, bed netting, permethrin-treated clothing, and sleeping in minimal-risk areas. People are at increased risk of bites in the early morning and late evening .
Amebas (ameboid protozoa) are single-celled eukaryotes characterized by movement via pseudopodia (temporary cytoplasmic extensions). Organisms in this group that can produce cutaneous disease include enteric pathogens (e.g. Entamoeba histolytica ) and free-living amebas such as Acanthamoeba spp. and Balamuthia mandrillaris . E. histolytica has a worldwide distribution and may infect the skin via inoculation or extension from the gastrointestinal tract. B. mandrillaris and Acanthamoeba spp. can cause skin infections and granulomatous encephalitis in immunocompromised and (for B. mandrillaris ) immunocompetent patients. Acanthamebiasis may present with papules, nodules, and ulcers on the trunk and extremities in patients with advanced HIV infection (see Ch. 78 ).
Amebiasis due to Entamoeba histolytica usually affects the gastrointestinal tract and rarely spreads to the skin
The skin can become involved by extension of rectal amebiasis to the anus, perianal skin or vulva, as well as by a fistula from a liver abscess to the skin of the abdominal wall
Cutaneous lesions are usually painful ulcers or verrucous plaques
Amebiasis in humans is primarily a gastrointestinal infection caused by Entamoeba histolytica . However, there can be extraintestinal manifestations, including cutaneous involvement .
E. histolytica infection results in approximately 50 million cases of invasive disease worldwide each year, causing 100 000 deaths annually . Infection is associated with poor sanitation, crowded living facilities, and lower socio-economic status. In high-income countries, risk factors include a history of travel to or residence in high-prevalence areas, institutionalization, immunosuppression, and sexual behavior (especially men having sex with men). Humans are the reservoir for the disease, and an asymptomatic carrier may excrete up to 45 million cysts a day in the stool. Transmission of amebiasis is fecal–oral via contaminated hands, water, or food and oral–anal sex.
Once the cyst is ingested, it makes its way to the colon, where it becomes a trophozoite. Although trophozoites can be excreted, cysts represent the primary excreted form . Infection of intestinal mucosa depends upon interaction of lectins on the surface of the ameba with mucin glycoproteins on the intestinal epithelium . The main mechanism by which E. histolytica produces disease is through tissue lysis . The trophozoites kill target cells upon direct contact, due in part to the release of proteolytic enzymes, e.g. cathepsin B and collagenase. The trophozoites also have the capacity to destroy neutrophils, resulting in release of their intracellular contents, which further contribute to the destruction of host tissues. The mechanisms of defense against E. histolytica include mucosal immune responses (e.g. antiamebic IgA antibodies), cell-mediated immune defense (e.g. cytotoxic T lymphocytes and production of lymphokines such as IFN-γ, which activate macrophages to kill the trophozoites), and non-immune defenses (e.g. production of mucus by colonic mucosa, inhibiting amebic adherence to and lysis of the mucosa).
Patients with symptomatic amebiasis due to E. histolytica typically develop colitis and present with abdominal pain, tenesmus, bloody diarrhea, and mucosal ulcerations . Extraintestinal complications, which can occur from hematogenous spread via invasion through the gastrointestinal epithelium, include hepatic abscesses, empyema and pericardial effusions . The skin is affected in <1% of patients with amebiasis. Skin involvement occurs as a result of extension of rectal amebiasis to the anus, perianal skin, or vulva; spread to the abdominal wall from a colostomy or after surgical drainage of a liver abscess; or inoculation of the penis during anal intercourse. Primary cutaneous amebiasis via external inoculation is exceedingly rare but has been reported on the face .
Cutaneous lesions can present as verrucous plaques or ulcers with a gray–white necrotic base ( Fig. 83.13 ). Ulcerative lesions are usually painful and somewhat oval in shape, with irregular borders and intervening areas of unaffected skin. One characteristic of these ulcers is extensive tissue destruction.

Histologically, ulcerated lesions have central necrosis with adjacent pseudoepitheliomatous hyperplasia. Mixed inflammatory infiltrates are present in the dermis and can extend into the subcutaneous tissue. Within the ulcerated and necrotic areas, it is possible to identify the trophozoites of E. histolytica . They have ample, finely granular eosinophilic cytoplasm, eccentric nuclei, and prominent nucleoli, and some may contain phagocytized red cells. Chronic lesions show prominent irregular epidermal hyperplasia and inflammatory infiltrates, with few organisms present. Touch and wet drop preparations from the pus may also be utilized to identify the trophozoites . Examination of fresh stool has a low yield for demonstrating the trophozoite, and multiple stool samples must be obtained . Where available, PCR may be used for detection. Once the diagnosis is established, evaluation of other body sites for involvement is recommended.
A diagnosis of amebiasis should be considered in patients with painful anogenital ulcers. In high-income countries, a patient with colitis and necrotic cutaneous ulcers would more likely have inflammatory bowel disease-associated pyoderma gangrenosum. Other infectious causes of skin ulcers, e.g. streptococci, dimorphic or opportunistic fungi, tuberculosis, and mixed bacterial flora (phagedenic or tropical ulcer), should be excluded. Verrucous lesions in the anogenital region may be confused with condylomata acuminata and squamous cell carcinoma.
Oral metronidazole is the drug of choice for amebiasis due to E. histolytica : for adults, 500–750 mg three times daily for 7–10 days and for children, 35–50 mg/kg/day divided into three doses for 10 days. Other medications that have been used include diloxanide, tinidazole, pentamidine, and iodoquinol .
B. mandrillaris is a free-living ameba that causes a rare, usually fatal encephalitis in immunocompetent individuals
Skin infection presents weeks to months prior to hematogenous spread to the central nervous system (CNS)
Slowly growing, indurated plaques favor the central face and occur less often on the extremities
B. mandrillaris is a free-living ameba that can infect the skin and subsequently lead to fatal encephalitis.
At least three genera of free-living amebas cause disease in humans, including Naegleria , Acanthamoeba , and Balamuthia . These amebas are found worldwide in the soil and (especially for the former two organisms) fresh water. Cutaneous infection with B. mandrillaris or Acanthamoeba spp. may precede development of granulomatous encephalitis. Such infections may be acquired from exposure of microabrasions or open wounds in the skin to soil and water sources; encephalitis can also result from infection of the nasal/respiratory mucosa via inhalation. Naegleria fowleri infection can cause acute, fatal encephalitis but is not known to have skin manifestations.
B. mandrillaris is an uncommon but increasingly recognized cause of encephalitis, with approximately 200 cases reported worldwide to date, including >90 in the US . Most of the affected individuals resided in warmer regions, including Latin America and the southern US . Unlike Acanthamoeba infections, which only affect immunocompromised patients, most B. mandrillaris infections occur in immunocompetent individuals, favoring children as well as the elderly; the male:female ratio is ∼2–3:1 . In addition, nearly 50% of the B. mandrillaris infections identified in the US have been in individuals of Hispanic ethnicity . Transmission of B. mandrillaris via solid organ transplantation has also been described.
B. mandrillaris is a free-living ameba that can exist both as a dormant cyst and as an infectious trophozoite. Because B. mandrillaris can cause disease in immunocompetent hosts, it is thought to be more virulent than Acanthamoeba . However, clinically unaffected individuals have been shown to have antibodies against B. mandrillaris . The presence of predisposing factors such as local disruption of the skin or mucosal barrier is likely required for infection. The trophozoites feed on human cells and spread to the CNS hematogenously .
B. mandrillaris causes a subacute to chronic granulomatous encephalitis that has a mortality rate of >80% . In a subset of patients, CNS involvement is preceded by the development of a slowly expanding, indurated, asymptomatic plaque on the central face or less often other sites such as an extremity (especially around the knee), the gluteal area, or the oral mucosa ( Fig. 83.14 ). A skin lesion may be present for 5–8 months before the organism disseminates to the CNS . As the plaque enlarges, it may become infiltrative (see Fig. 83.14B ) and occasionally ulcerates. Although there is usually a single skin lesion, local “satellite” lesions or involvement of multiple sites can occur. Neurologic manifestations are similar to those in other forms of meningoencephalitis and include headache, altered mental status, cranial nerve dysfunction, and seizures; however, the symptoms may have an insidious onset and chronic course.
The diagnosis of B. mandrillaris infection is often made at autopsy or by skin biopsy . In the dermis of affected skin, there is a mixed granulomatous infiltrate with many giant cells, but usually few identifiable trophozoites . Immunohistochemical staining or PCR-based analysis of skin specimens can provide definitive diagnosis . Culture and isolation of B. mandrillaris requires a complex medium containing fetal bovine serum or a specialized cell type (e.g. monkey kidney cells, human lung fibroblasts) . Examination of the cerebrospinal fluid (CSF) may show motile amebic trophozoites with pseudopodia formation. Brain imaging in patients with advanced disease reveals calcified, mass-like lesions .
Considering the poor prognosis of B. mandrillaris encephalitis, early diagnosis when the disease is limited to the skin is critical. Multiagent therapy for a prolonged period (e.g. 12 months) is recommended, with reported regimens including miltefosine together with various combinations (2–5 drugs) of pentamidine, sulfadiazine, flucytosine, an azole antifungal, liposomal amphotericin B, a macrolide antibiotic (clarithromycin or azithromycin), and albendazole . However, controlled trials are lacking. Surgical excision of cutaneous lesions should also be considered when possible. .
▪ Chagas disease: American trypanosomiasis, Chagas–Mazza disease ▪ African trypanosomiasis: African sleeping sickness
Although the genus Trypanosoma consists of at least 20 species of protozoa, only two are known to cause human disease. Chagas disease (American trypanosomiasis) is caused by T. cruzi infection and transmitted by reduviid bugs, while African trypanosomiasis is caused by T. brucei infection and transmitted by tsetse flies.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here