Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The principal manifestation of most endocrine diseases is over- or undersecretion of one or more hormones, but the causes of endocrine disease are not unique to endocrinology as a subspecialty of medicine. Major causes of endocrine disease that are shared with diseases of other organ systems include benign or malignant proliferation of endocrine cells; destruction of endocrine cells by autoimmune, infectious, or other infiltrative processes; mutations in genes expressed by endocrine cells; and alterations in endocrine cell function caused by metabolic abnormalities or drugs. The understanding of hormone action and endocrine diseases has been improved not only by classic physiology and biochemistry but also by newer technologies such as whole-exome sequencing, metabolomics, and bioinformatics.
Endocrine action, by which a hormone secreted into the blood stream acts at a distance, can be contrasted with paracrine action, which is when a growth factor or other signaling molecule secreted from one cell acts on adjacent cells, and autocrine action, when a cell secretes a signaling molecule that acts on the same cell. However, the distinction among endocrine, paracrine, and autocrine actions is not sharp. In some cases, a factor such as parathyroid hormone–related peptide (PTHrP) that acts physiologically in paracrine fashion during normal bone development may act as an endocrine factor in the syndrome of humoral hypercalcemia of malignancy ( Chapter 227 ).
Two broad categories of hormone synthesis are responsible for the synthesis of peptide hormones and steroid hormones, including the active form of vitamin D, thyroid hormones, catecholamines, and other nonpeptide hormones. In the former category, hormone structure is encoded genetically, and mRNA translation yields a protein precursor (pre-prohormone) that is generally cleaved through successive steps to yield the mature secreted product. Some protein precursors such as proopiomelanocortin contain multiple hormonal products, in this case adrenocorticotropic hormone (ACTH), melanocyte-stimulating hormone (MSH), and endorphins. In certain situations, inappropriate secretion of immature hormones creates a pathologic condition (e.g., excessive proinsulin secretion by insulinomas). Post-translational modifications occur for some hormones, such as disulfide bond formation for vasopressin and insulin; C-peptide cleavage for insulin; and glycosylation of the pituitary glycoprotein hormones, thyroid-stimulating hormone (TSH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH). Mutations in genes that encode peptide hormones can lead to disruption of normal hormone synthesis or secretion, a rare cause of hormone deficiency. Peptide hormones are typically stored in secretory granules, and they are secreted by an exocytosis process that is regulated by calcium (Ca 2+ ) and other factors. For steroids and other nonpeptide hormones, hormone synthesis is accomplished by a series of enzymatic steps that act on precursors (cholesterol for steroid hormones; aromatic amino acids for thyroid hormones, catecholamines, and related compounds). Mutations in genes encoding enzymes responsible for one or more steps in hormone synthesis can lead to hormone deficiency and/or excess of another hormone, as in congenital adrenal hyperplasia ( Chapter 214 ).
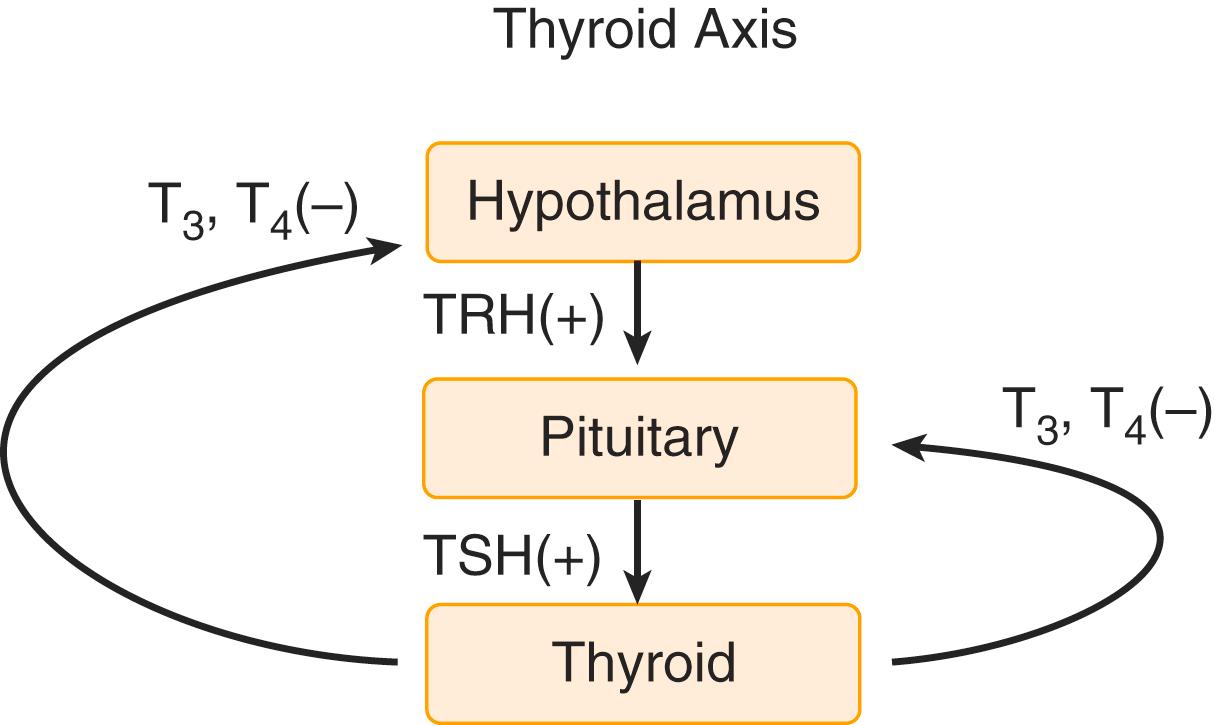
Negative feedback regulation is the general principle that governs normal hormone synthesis and secretion. For endocrine glands whose growth and hormone secretion are stimulated by pituitary trophic hormones (gonads, adrenal cortex, thyroid), the hormone secreted by the gland acts directly on cognate pituitary trophic cells (e.g., cortisol acting on ACTH-secreting pituitary corticotrophs) to suppress hormone secretion ( Fig. 203-1 ). Conversely, a physiologically meaningful reduction in target gland hormone secretion leads to increased pituitary trophic hormone secretion. In many other cases, negative feedback regulation operates without the pituitary as an intermediate (e.g., PTH secretion from the parathyroid glands regulates extracellular Ca 2+ homeostasis, and Ca 2+ feeds back directly on parathyroid cells via a Ca 2+ sensing receptor to regulate PTH secretion). Chronic hormone deficiency with resultant loss of negative feedback can lead to hypersecretion of the cognate trophic hormone and even to neoplastic proliferation of trophic hormone–secreting cells. Examples include Nelson syndrome ( Chapter 205 ) in which corticotroph tumors form after adrenalectomy, and tertiary hyperparathyroidism in which parathyroid adenomas occur in the setting of chronic hypocalcemia ( Chapter 227 ). In some adrenal cortical disorders, hormone deficiency leads to loss of negative feedback of trophic hormone secretion, which in turn causes pathologic hypersecretion of alternative steroid hormones. The various forms of congenital adrenal hyperplasia ( Chapter 214 ) are caused by mutations in one of the several enzymes in the cortisol biosynthetic pathway. The most common such mutation, which is 21-hydroxylase deficiency, can lead to virilization in female infants, with excessive adrenal androgen secretion caused by ACTH stimulation in the face of inability to synthesize cortisol. Inhibition of enzymatic steps in hormone synthesis, such as aromatase inhibitors to decrease estrogen formation in estrogen receptor–positive forms of breast cancer ( Chapter 183 ), may be an important therapeutic target.
Hormone hypersecretion syndromes, in which excessive hormone secretion occurs in the face of “normal” levels of the factor that ordinarily suppresses the cognate hormone, are by definition caused by some intrinsic defect in negative feedback suppression. This defect may be caused by neoplastic proliferation of hormone-secreting cells, so that “basal” hormone secretion from the increased mass of cells exceeds physiologic levels. This defect also may be due to alterations in the intrinsic “set-point” for negative feedback suppression of hormone secretion. In practice, it may be impossible to differentiate between these two mechanisms, and they are not mutually exclusive.
Hormone secretion is subject to many additional forms of regulation beyond simple negative feedback suppression. These regulatory mechanisms include metabolic, neural, and other internal and environmental inputs. The temporal pattern of hormone secretion is often related to diurnal rhythms, as classically seen for cortisol, and also pulsatility. Changes in gonadotropin secretion during the menstrual cycle ( Chapter 218 ) and during the course of puberty ( Chapter 214 ) are striking examples of complex regulation of temporal patterns of hormone secretion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here