Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
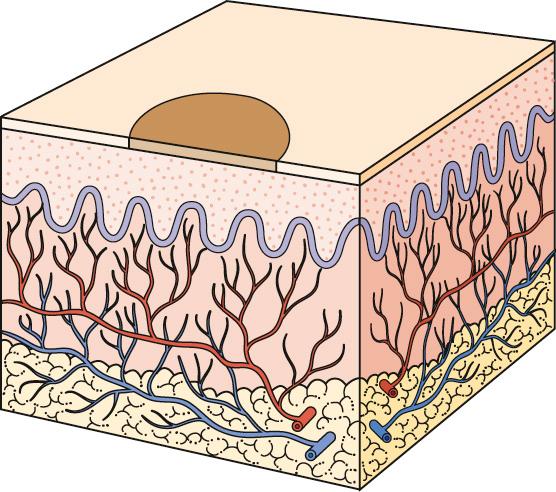
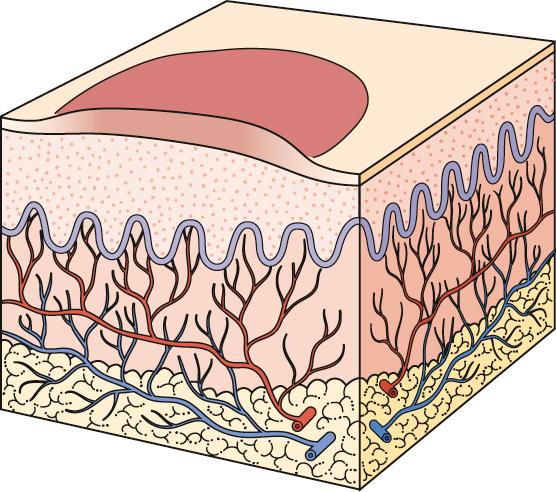
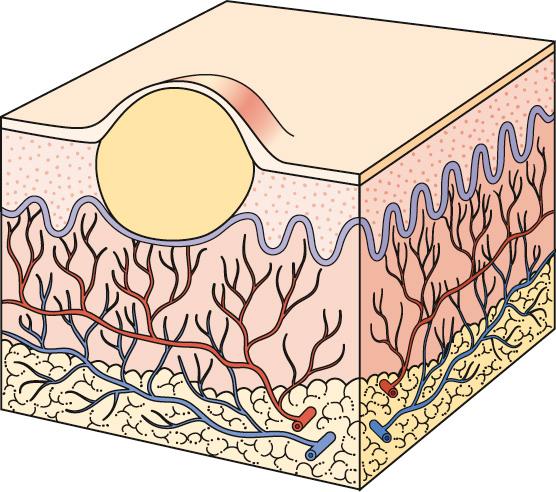
The skin is divided into three layers: the epidermis, the dermis, and the subcutaneous tissue. The skin is thicker on the dorsal and extensor surfaces than on the ventral and flexor surfaces.
The epidermis is the outermost part of the skin; it is stratified squamous epithelium. The thickness of the epidermis ranges from 0.05 mm on the eyelids to 1.5 mm on the palms and soles. The microscopic anatomy of the dermoepidermal junction is complex; it is discussed in detail in Chapter 16 . The innermost layer of the epidermis consists of a single row of columnar cells called basal cells. Basal cells divide to form keratinocytes, which comprise the spinous layer. The cells of the spinous layer are connected to each other by intercellular bridges or spines, which appear histologically as lines between cells. The keratinocytes synthesize insoluble protein, which remains in the cell and eventually becomes a major component of the outer layer (stratum corneum). The cells continue to flatten, and their cytoplasm appears granular (stratum granulosum); they finally die as they reach the surface to form the stratum corneum. There are three types of branched cells in the epidermis: the melanocyte, which synthesizes pigment (melanin); the Langerhans cell, which serves as a frontline element in immune reactions of the skin; and the Merkel cell, which serves as a mechanoreceptor important for light touch.
The dermis varies in thickness from 0.3 mm on the eyelid to 3.0 mm on the back; it is composed of three types of connective tissue: collagen, elastic tissue, and reticular fibers. The dermis is divided into two layers: the thin upper layer, called the papillary layer, is composed of thin, haphazardly arranged collagen fibers; the thicker lower layer, called the reticular layer, extends from the base of the papillary layer to the subcutaneous tissue and is composed of thick collagen fibers that are arranged parallel to the surface of the skin. Histiocytes are wandering macrophages that accumulate hemosiderin, melanin, and debris created by inflammation. Mast cells, located primarily around blood vessels, manufacture and release histamine and heparin.
The sensations of touch and pressure are received by Meissner and Vater–Pacini corpuscles. The sensations of pain, itch, and temperature are received by unmyelinated nerve endings in the papillary dermis. A low intensity of stimulation created by inflammation causes itching, whereas a high intensity of stimulation created by inflammation causes pain. Therefore scratching converts the intolerable sensation of itching to the more tolerable sensation of pain and eliminates pruritus.
The autonomic nervous system supplies the motor innervation of the skin. Adrenergic fibers innervate the blood vessels (vasoconstriction), hair erector muscles, and apocrine glands. Autonomic fibers to eccrine sweat glands are cholinergic. The sebaceous gland is regulated by the endocrine system and is not innervated by autonomic fibers. The anatomy of the hair follicle is described in Chapter 24 .
What could be easier than the diagnosis of skin disease? The pathology is before your eyes! Why then do non-dermatologists have such difficulty interpreting what they see?
There are three reasons. First, there are literally hundreds of cutaneous diseases. Second, a single entity can vary in its appearance. A common seborrheic keratosis, for example, may have a smooth, rough, or eroded surface and a border that is either uniform or as irregular as a melanoma. Third, skin diseases are dynamic and change in morphology. Many diseases undergo an evolutionary process: herpes simplex may begin as a red papule, evolve into a blister, and then become an erosion that heals with scarring. If hundreds of entities can individually vary in appearance and evolve through several stages, then it is necessary to recognize thousands of permutations to diagnose cutaneous entities confidently. What at first glance appeared to be simple to diagnose may later appear to be simply impossible to identify.
Dermatology is a morphologically oriented specialty. As in other specialties, the medical history is important; however, the ability to interpret what is observed is even more important. The diagnosis of skin disease must be approached in an orderly and logical manner. The temptation to make rapid judgments after hasty observation must be controlled.
The recommended approach to the patient with skin disease is as follows:
History. Obtain a brief history, noting duration, rate of onset, location, symptoms, family history, medications, allergies, occupation, and previous treatment.
Distribution. Determine the extent of the eruption by having the patient disrobe completely.
Primary lesion. Determine the primary lesion. Examine the lesions carefully; a handheld magnifier and a dermatoscope are valuable aids for studying skin lesions. Determine the nature of any secondary or special lesions.
Differential diagnosis. Formulate a differential diagnosis.
Tests. Obtain a biopsy and perform laboratory tests, such as skin biopsy, potassium hydroxide examination for fungi, skin scrapings for scabies, Gram stain, fungal and bacterial cultures, cytology (Tzanck test), Wood's light examination, patch tests, dark field examination, and blood tests.
Distribution. The skin should be examined methodically. A visual scan over wide areas is inefficient. It is most productive to mentally divide the skin surface into several sections and carefully study each section. For example, when studying the face, examine the area around each eye, the nose, the mouth, the cheeks, and the temples.
During an examination, patients may show small areas of their skin, tell the physician that the rest of the eruption looks the same, and expect an immediate diagnosis. The remainder of the eruption may or may not look the same. Patients with rashes should receive a complete skin examination to determine the distribution and confirm the diagnosis. Decisions about quantities of medication to dispense require visualization of the big picture. Many dermatologists now advocate a complete skin examination for all of their patients. Some dermatologists advocate a case-by-case approach, since some patients with a focused problem, such as a plantar wart, may be reluctant to undergo a complete skin examination.
Primary Lesions and Surface Characteristics. Lesions should be examined carefully. Standing back and viewing a disease process provides valuable information about the distribution. Close examination with a magnifying device provides much more information. Often the primary lesion is identified and the diagnosis is confirmed at this step. The physician should learn the surface characteristics of all the common entities and gain experience by examining known entities. A skin-colored papule might be a wart, sebaceous hyperplasia, or a basal cell carcinoma. The surface characteristics of many lesions are illustrated throughout this book.
Most skin diseases can be managed successfully with the numerous agents and techniques available. If a diagnosis has not been established, medications should not be prescribed; this applies particularly to prescription of topical steroids. Some physicians are tempted to experiment with various medications and, if the treatment fails, to refer the patient to a specialist. This is not a logical or efficient way to practice medicine.
Most skin diseases begin with a basic lesion that is referred to as a primary lesion. Identification of the primary lesion is the key to accurate interpretation and description of cutaneous disease. Its presence provides the initial orientation and allows the formulation of a differential diagnosis. Definitions of the primary lesions and their differential diagnoses are listed and illustrated on pp. 3 to 11 .
Secondary lesions develop during the evolutionary process of skin disease or are created by scratching or infection. They may be the only type of lesion present, in which case the primary disease process must be inferred. The differential diagnoses of secondary lesions are listed and illustrated on pp. 12 to 16 .
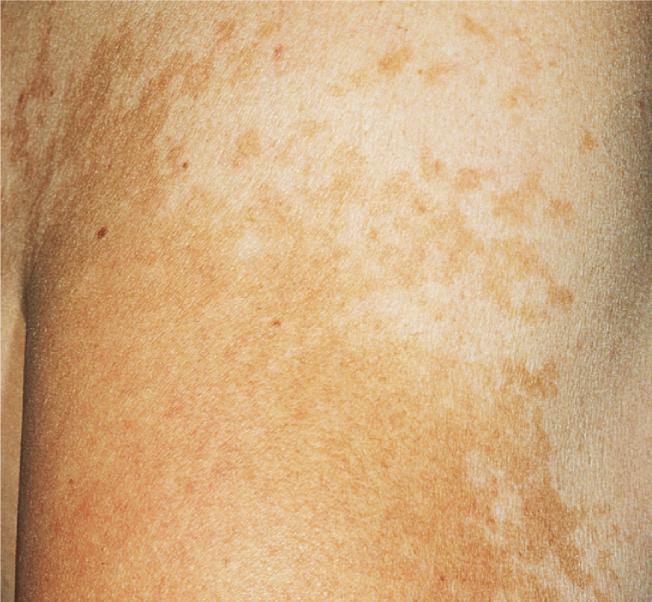
A circumscribed, flat discoloration that may be brown, blue, red, or hypopigmented
Becker nevus ( p. 871 )
Erythrasma ( p. 492 )
Fixed drug eruption ( p. 563 )
Freckles ( p. 779 )
Junction nevus ( p. 864 )
Lentigo ( p. 779 )
Lentigo maligna ( p. 880 )
Melasma ( p. 780 )
Photoallergic drug eruption ( p. 771 )
Phototoxic drug eruption ( p. 768 )
Stasis dermatitis ( p. 118 )
Tinea nigra palmaris
Ink (tattoo)
Maculae ceruleae (lice)
Mongolian spot
Ochronosis





An elevated solid lesion up to 0.5 cm in diameter; color varies; papules may become confluent and form plaques
Acrochordon (skin tag) ( p. 793 )
Adenoma sebaceum ( p. 1003 )
Basal cell carcinoma ( p. 815 )
Closed comedones (acne) ( p. 217 )
Flat warts ( p. 449 )
Granuloma annulare ( p. 992 )
Lichen nitidus
Lichen sclerosus ( p. 321 )
Milia ( p. 252 )
Neurofibroma ( p. 1000 )
Nevi (dermal) ( p. 863 )
Pearly penile papules ( p. 415 )
Pseudoxanthoma elasticum
Senile sebaceous hyperplasia ( p. 812 )
Skin tags (acrochordons) ( p. 793 )
Syringoma ( p. 814 )
Acne ( p. 215 )
Atopic dermatitis ( p. 149 )
Cat-scratch disease ( p. 610 )
Cherry angioma ( p. 917 )
Cholinergic urticaria ( p. 191 )
Chondrodermatitis nodularis ( p. 808 )
Eczema ( p. 90 )
Folliculitis ( p. 349 )
Insect bites
Leukocytoclastic vasculitis ( p. 734 )
Miliaria
Polymorphous light eruption ( p. 757 )
Psoriasis ( p. 264 )
Scabies ( p. 571 )
Urticaria ( p. 176 )



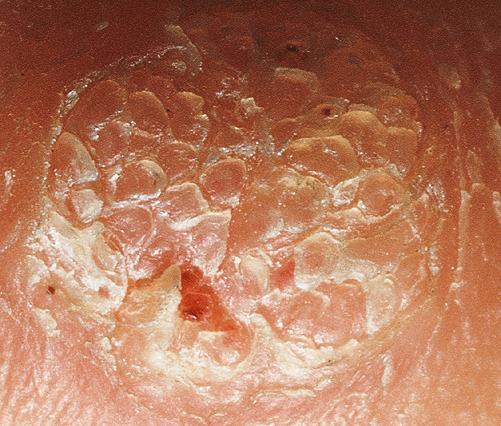














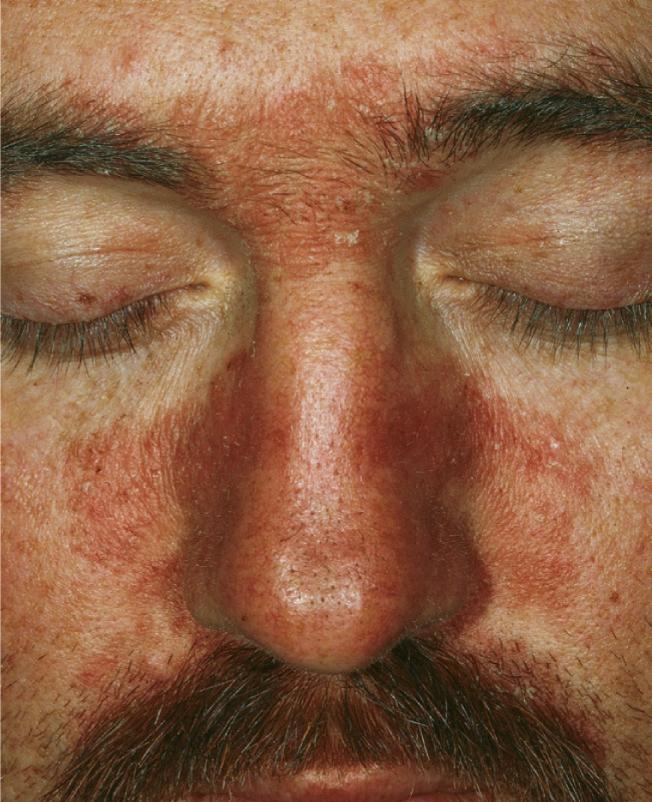
A circumscribed, elevated, superficial, solid lesion more than 0.5 cm in diameter, often formed by the confluence of papules
Chronic cutaneous (discoid) lupus erythematosus ( pp. 676 , 954 )
Cutaneous T-cell lymphoma ( p. 844 )
Eczema ( p. 90 )
Lichen planus ( p. 313 )
Paget disease ( p. 855 )
Papulosquamous (papular and scaling) lesions ( p. 264 )
Pityriasis rosea ( p. 310 )
Psoriasis ( p. 264 )
Seborrheic dermatitis ( p. 304 )
Sweet syndrome ( p. 740 )
Syphilis (secondary) ( p. 388 )
Tinea corporis ( p. 493 )
Tinea pedis ( p. 486 )
Tinea versicolor ( p. 520 )














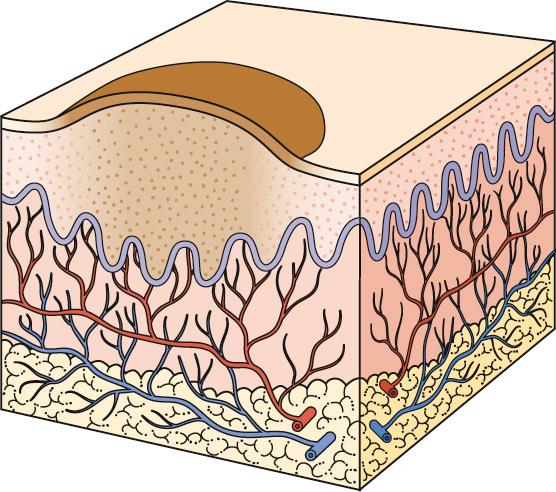
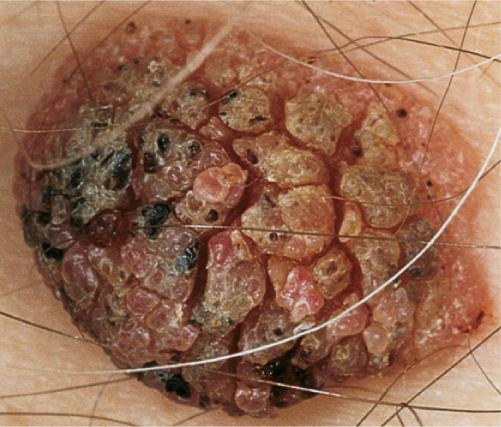
A circumscribed, elevated, solid lesion more than 0.5 cm in diameter; a large nodule is referred to as a tumor
Basal cell carcinoma ( p. 815 )
Cutaneous T-cell lymphoma ( p. 844 )
Erythema nodosum ( p. 726 )
Furuncle ( p. 354 )
Hemangioma ( p. 905 )
Kaposi sarcoma ( p. 921 )
Keratoacanthoma ( p. 802 )
Lipoma
Lymphoma ( p. 843 )
Melanoma ( p. 875 )
Metastatic carcinoma ( p. 860 )
Neurofibromatosis ( p. 998 )
Prurigo nodularis ( p. 115 )
Sporotrichosis
Squamous cell carcinoma ( p. 836 )
Warts ( p. 445 )
Xanthoma ( p. 996 )









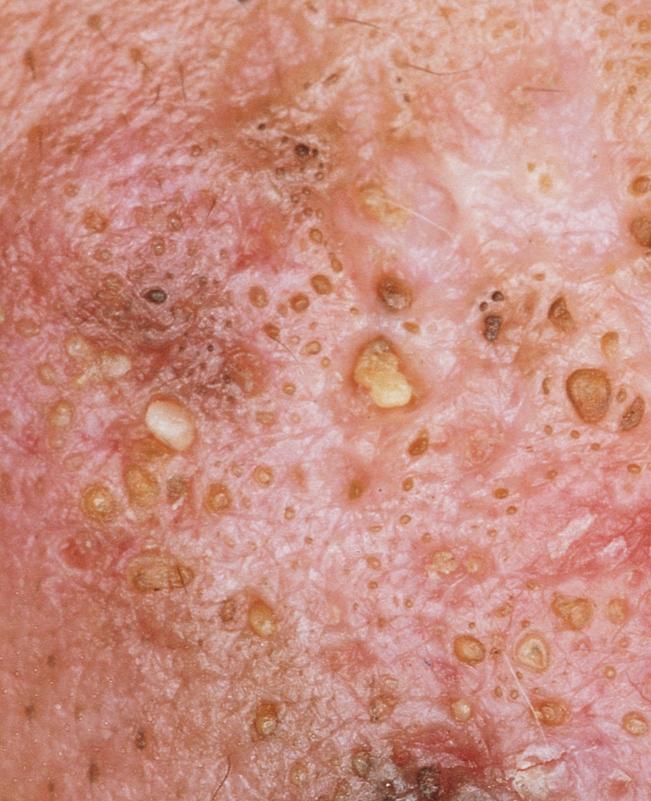
A circumscribed collection of leukocytes and free fluid that varies in size
Acne ( p. 215 )
Candidiasis ( p. 508 )
Chickenpox ( p. 464 )
Dermatophyte infection ( p. 483 )
Dyshidrosis (pompholyx) ( p. 106 )
Folliculitis ( p. 349 )
Gonorrhea (disseminated) ( p. 410 )
Herpes zoster ( p. 469 )
Hidradenitis suppurativa ( p. 260 )
Impetigo ( p. 331 )
Pseudomonas folliculitis ( p. 362 )
Psoriasis ( p. 264 )
Pyoderma gangrenosum ( p. 743 )
Rosacea ( p. 256 )
Scabies ( p. 571 )
Varicella ( p. 464 )









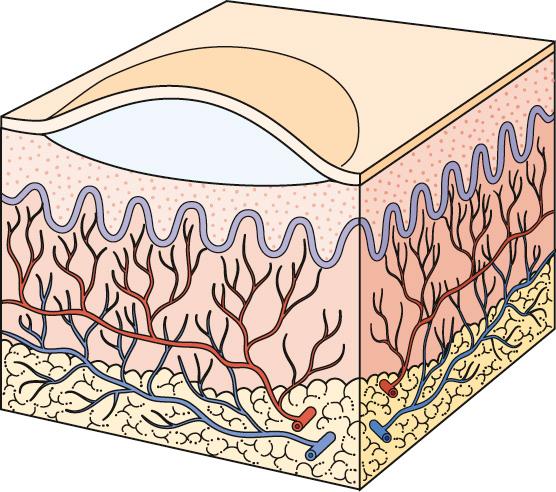
A circumscribed collection of free fluid up to 0.5 cm in diameter
Benign familial chronic pemphigus ( p. 658 )
Cat-scratch disease ( p. 610 )
Chickenpox ( p. 464 )
Dermatitis herpetiformis ( p. 635 )
Eczema (acute) ( p. 90 )
Herpes zoster ( p. 469 )
Impetigo ( p. 331 )
Lichen planus ( p. 313 )
Pemphigus foliaceus ( p. 641 )
Porphyria cutanea tarda ( p. 763 )
Scabies ( p. 571 )
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here