Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The practitioner frequently has the opportunity to manage the child for whom the chief complaint is a “swollen eye” ( Fig. 84.1 ). Some children have trivial or self-limited disorders, but others can have sight- or life-threatening problems. Noninfectious causes of the swollen eye can often be distinguished from infectious causes by a detailed history of the onset and progression of the eye swelling. Infectious causes of eye swelling are usually acute in presentation. Differentiating preseptal (common) and orbital (rare) causes of eye swelling is critical to management and can usually be accomplished based on the physical examination.
The noninfectious causes of swelling of or around the eye include (1) blunt trauma (leading to the proverbial “black” eye), (2) tumor, (3) local edema, and (4) allergy. In cases of blunt trauma, history provides the key to the diagnosis. Eyelid swelling continues to increase for 48 hours and then resolves over several days. Tumors that characteristically involve the eye include hemangioma of the lid, ocular tumors such as retinoblastoma and choroidal melanoma, and orbital neoplasms such as neuroblastoma and rhabdomyosarcoma. Other tumors reported to cause orbital involvement are Langerhans cell histiocytosis and granulocytic sarcoma. , Tumors usually cause gradual onset of proptosis in the absence of inflammation. Orbital pseudotumor (idiopathic orbital inflammation), an inflammatory disorder of the orbital tissues, manifests as eyelid swelling, red eye, pain, and decreased ocular motility. Hypoproteinemia and congestive heart failure cause eyelid swelling due to local edema; characteristic findings are bilateral, boggy, nontender, nondiscolored soft tissue swelling. Allergic inflammation includes angioneurotic edema or contact hypersensitivity. Superficially, allergic inflammation can resemble acute infection; however, the presence of pruritus and the absence of tenderness are helpful distinguishing characteristics.
The anatomy of the eye is important for an understanding of its susceptibility to spread infection from contiguous structures. Veins that drain the orbit, the ethmoid and maxillary sinuses, and the skin of the eye and periorbital tissues ( Fig. 84.2 ) constitute an anastomosing and valveless network. This venous system provides opportunities for spread of infection from one anatomic site to another and predisposes to involvement of the cavernous sinus.
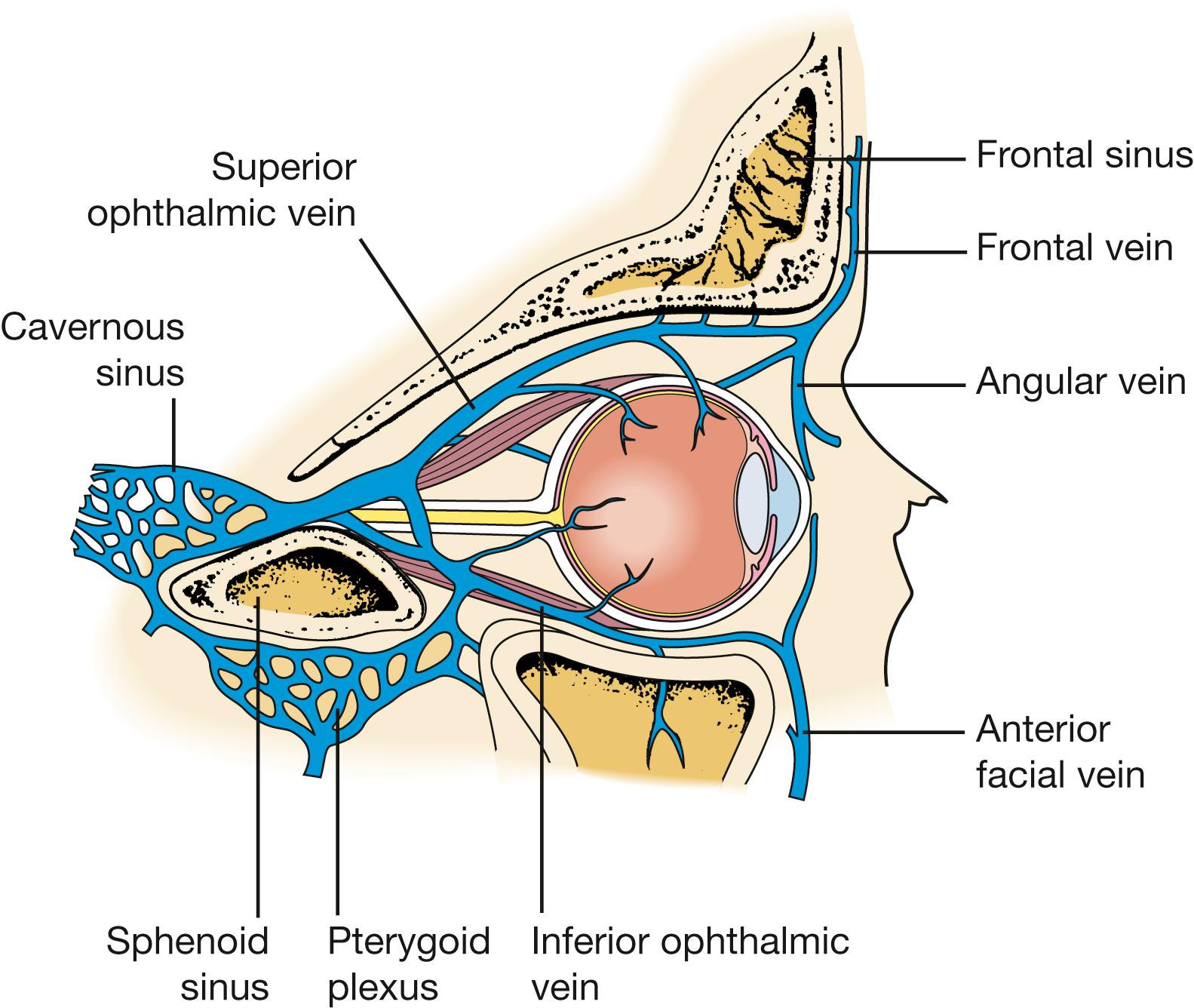
Fig. 84.3 demonstrates the relationship between the eye and the paranasal sinuses. The roof of the orbit is the floor of the frontal sinus, and the floor of the orbit is the roof of the maxillary sinus. The medial wall of the orbit is formed by the frontal maxillary process, the lacrimal bone, the lamina papyracea of the ethmoid bone, and a small part of the sphenoid bone. Infection originating in the mucosa of the paranasal sinuses can spread to involve the bone (osteitis with or without subperiosteal abscess) and the intraorbital contents. Orbital infection can occur through natural bony dehiscences in the lamina papyracea of the ethmoid or frontal bones or through foramina through which the ethmoidal arteries pass.
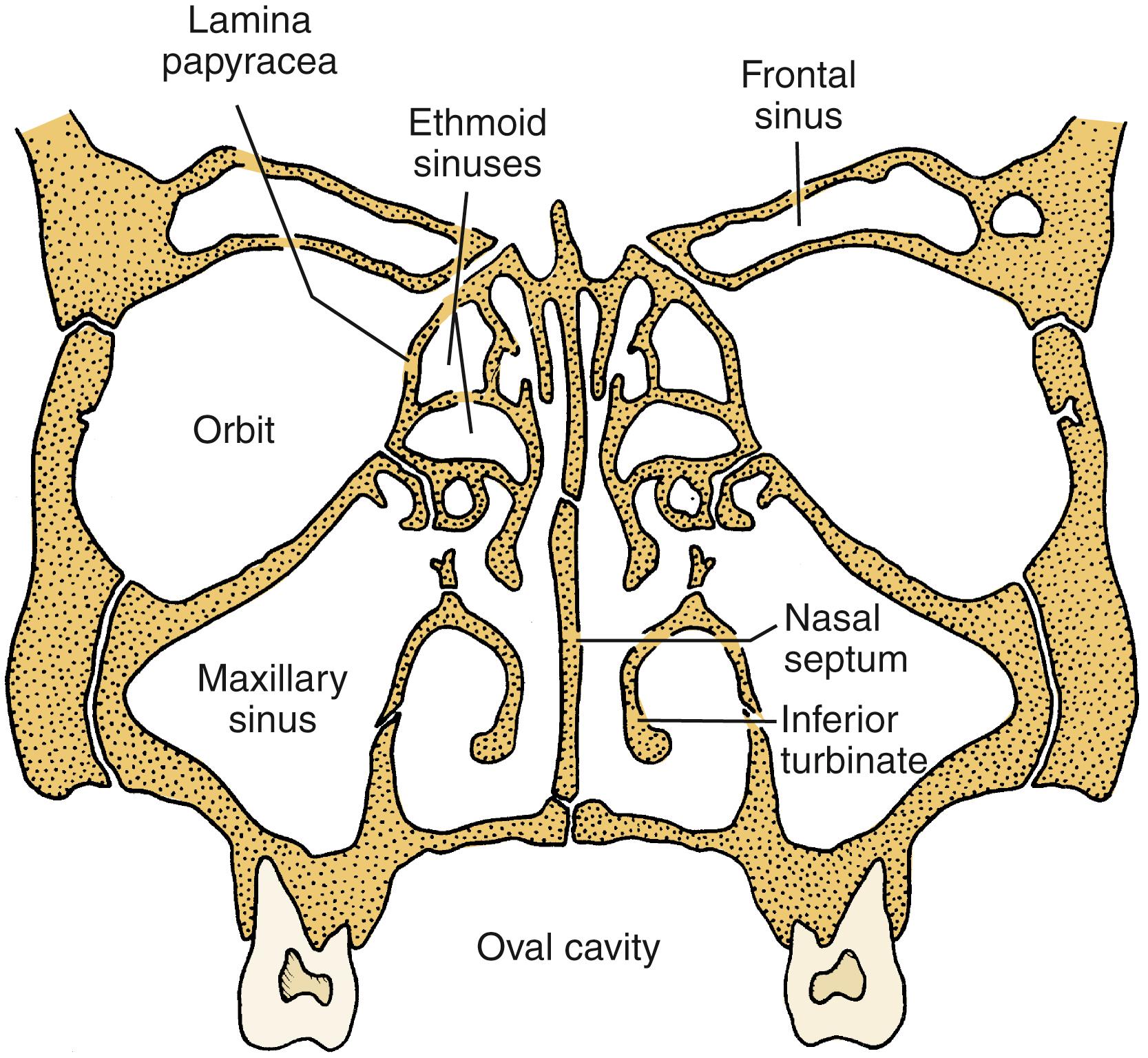
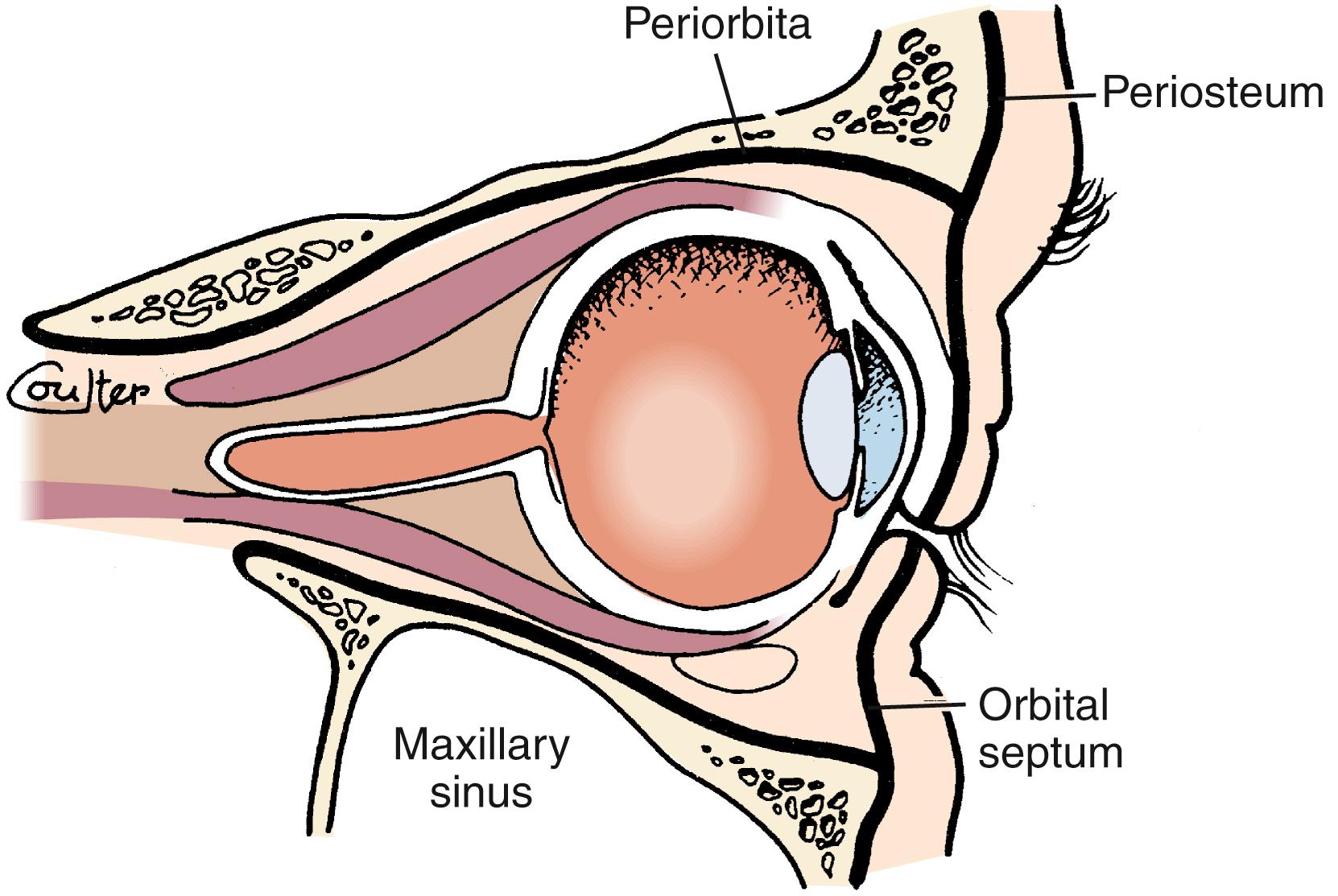
Fig. 84.4 shows the position of the orbital septum, a connective tissue extension of the periosteum (or periorbita) that is reflected into the upper and lower eyelids. Infection of tissues anterior to the orbital septum are described as periorbital or preseptal. The septum provides a nearly impervious barrier to spread of infection to the orbit. Although preseptal cellulitis or periorbital cellulitis (the terms may be used interchangeably) often is considered a diagnosis, either term is an inadequate diagnostic label unless accompanied by a modifier that indicates likely pathogenesis. In the remainder of this chapter, preseptal cellulitis is the preferred term.
Infectious causes of preseptal cellulitis occur in the following three settings: (1) secondary to a localized infection or inflammation of the conjunctiva, eyelids, or adjacent structures (e.g., conjunctivitis, hordeolum, acute chalazion, dacryocystitis, dacryoadenitis, impetigo, traumatic bacterial cellulitis); (2) secondary to hematogenous dissemination of nasopharyngeal pathogens to the periorbital tissue; and (3) as a manifestation of inflammatory edema in patients with acute sinusitis ( Box 84.1 ).
Conjunctivitis
Hordeolum
Dacryoadenitis
Dacryocystitis
Bacterial cellulitis (trauma)
Bacteremic periorbital cellulitis
Acute sinusitis
Inflammatory edema
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here