Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Preoperative planning begins with a thorough history and physical examination to determine the cause and location of hip pain, the general medical condition of the patient, and the functional goals of the patient.
Radiographic evaluation is helpful in determining the cause of hip arthroplasty failure and in assessing component type, component alignment, bone stock, and infectious or osteolytic processes.
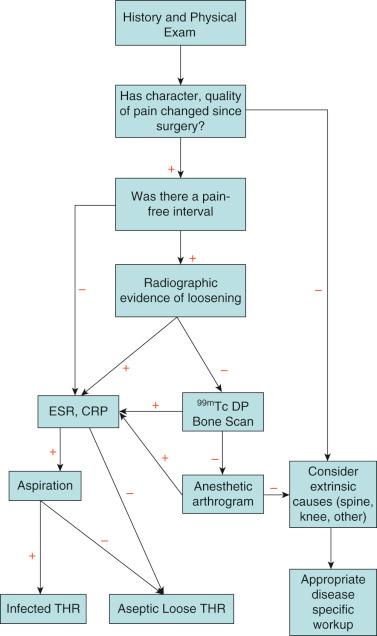
Infection is a source of primary hip arthroplasty failure that should not be missed; evaluation requires familiarity with diagnostic algorithms.
Bearing and trunnion failures require surgeon knowledge of surveillance and diagnostic methods.
Using appropriate techniques and tools during component removal allows bone stock preservation at the time of revision.
Templating allows the surgeon to anticipate the need for specific surgical instruments, components, and bone grafts intraoperatively.
Revision total hip arthroplasty (THA) is a complex procedure associated with inferior patient outcomes, higher rates of complications, and greater hospital resource use compared with primary THA. Furthermore, the number of revision THA procedures is expected to increase in proportion to the substantial increase in primary THA procedures. Historically, much effort has been placed on improving implant design, materials, and surgical techniques to improve outcomes of revision surgery. Although these efforts have generated many benefits, preoperative planning is an imperative, but often overlooked, step in anticipating the added challenges of revision surgery and minimizing complications. The process of preoperative planning for revision THA surgery is not algorithmic but rather includes three consistent steps.
First, the surgeon must diagnose the specific mode and cause of failure. Patient complaints can often be vague; thus, a thorough history, physical examination, and diagnostic evaluation are required to determine why revision surgery is indicated. Second, the surgeon must identify the goals of surgery. This entails identifying the technical goals of surgery, such as improving abductor tension or improving alignment of the acetabulum, and determining the patient-oriented goals of surgery, such as reducing hip pain or preventing hip dislocation. The patient must actively contribute to the goals of surgery and be made aware of the risks of surgery. Third, the surgeon must create a surgical plan that involves templating, anticipating alternative surgical methods, and ensuring that all necessary implants, instruments, and bone grafts are readily available on the day of surgery. The entire preoperative planning process is critical to the success of the surgery.
The preoperative planning process begins during the patient's first office visit. The surgeon should listen carefully to the patient's complaints and begin to establish the surgeon–patient relationship and embark on the process of shared decision making with the patient. The history and physical examination should be thorough and should include significant detail about the hip and general medical conditions. Hospital records, previous radiographs, and all previous operative reports, with implant labels, should be brought to the visit or obtained from the initial hospital, as the case may be.
Patients often present with reports of pain, wound drainage, or instability of the hip ( Fig. 89.1 ). The pain should be defined in terms of its quality, severity, onset, progression, and location, as well as alleviating and exacerbating factors. The type of pain can be suggestive of a diagnosis. Aseptic loosening commonly presents with pain, which is worse with activity and is improved with rest. Pain in the groin or the gluteal region can be suggestive of a loose acetabular component, whereas pain in the thigh is suggestive of problems of the femoral component. Groin pain occasionally can be due to hernias, lymphadenopathy, psoas abscess, or various gynecologic or genitourinary causes. Start-up pain or pain with walking a few steps is also a hallmark of a loose femoral component. If the patient had a pain-free interval after surgery, existing pain may be due to late infection, aseptic loosening, stress fracture, or osteolysis. Persistent pain after surgery without a pain-free interval is suggestive of early infection, failure to obtain initial implant stability, periprosthetic fracture, or misdiagnosis of the original problem. Constant pain, pain at rest, or night pain may be due to infection or malignancy. Pain associated with a decreased range of motion (ROM) is a sign of infection, heterotopic ossification, subsidence, or protrusio acetabuli. Acute pain is associated with hip dislocation, acute liner dissociation, or periprosthetic fracture. Patients with lumbar spine disease may be more active after hip arthroplasty, causing exacerbation of their neurogenic claudication. Metal-on-metal (MOM) bearing failures and modular stem-neck or neck-head trunnion corrosion may present with new-onset groin pain, grinding, limp, abductor weakness, masses, or no symptoms at all. Ceramic bearing failures may present with squeaking, crepitus, or sudden nonspecific pain in the case of implant fracture.
Thigh pain, although sometimes associated with a loose femoral component, is more commonly associated with well-fixed porous ingrowth or press-fit femoral components. Persistent thigh pain with no radiographic evidence of loosening has been described in 12% to 41% of patients with cementless implants, although with modern implants and techniques, it is probably less common now. Some patients with persistent thigh pain have also been found to have well-fixed femoral components at the time of surgery. Femoral component revision can be indicated for continued thigh pain despite well-fixed components, although this should be undertaken with caution owing to the lack of predictability of the surgical outcome. Tip-of-stem pain may be caused by modulus mismatch between a stiff cementless femoral stem and the less stiff surrounding bone, although this usually improves over time.
Hip instability is another common chief complaint. For these patients, a history of dislocation, including the number of dislocations, the timing of dislocation relative to the date of surgery, the position of the leg at the time of dislocation, the surgical approach used for the index procedure, and the method of reduction of the hip should be elicited. For patients who have symptoms of instability without dislocation, identifying the position of the leg when instability arises is important. Preoperative live fluoroscopy may be obtained to demonstrate the positions of impingement and instability, although a careful examination under anesthetic can accomplish the same purpose. Causes of instability include inadequate soft tissue tension, component malposition, polyethylene wear, bony impingement, adverse local tissue reactions (ALTR) and history of extensive spine fusion, especially if done after a successful and stable hip replacement. Patients with dual mobility bearings may experience acute pain and limited mobility without a clearly shortened or rotated extremity.
Intrinsic hip pain after hip arthroplasty must be distinguished from pain from extrinsic causes ( Box 89.1 ). Intrinsic causes of pain include mechanical loosening, sepsis, stress fracture, implant failure, modulus mismatch, and subluxation or impingement. Extrinsic causes of pain include lumbar spine disease, neurogenic or vascular claudication, trochanteric pain syndrome related to bursitis, abductor avulsion, tendinitis or abductor deficiency, peripheral nerve dysfunction, abductor or iliopsoas tendinitis, femoral or inguinal hernia, and malignancy. A snapping hip may be confused with hip subluxation. Nonunion of the greater trochanter or painful hardware at the trochanter from cerclage wires or a trochanter fixation plate produces pain over the trochanter. Spinal stenosis can create radicular pain in the hip, thigh, and gluteal region. Vascular claudication from aortoiliac artery stenosis or in the gluteal branches can cause pain that is worse with activity, better with rest, and also present in the calf if distal run-off is poor. Although vascular claudication is typically due to atherosclerotic disease, it may also be caused by vascular injury during the primary surgery or by malpositioned acetabular screws.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here