Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On average, up to 12% of liveborn infants in the developed world are born prior to term. These rates have increased as a consequence of assisted reproductive technology and earlier intervention for either maternal or fetal well-being. The causes of birth prior to term are many ( Table 15.1 ). The care of the premature neonate has improved dramatically over the past 100 years, during which time mortality rate has fallen from 40 deaths for each 1000 live births at the turn of the 20th century, to the current rates of four deaths per 1000 live births in the developed world. These improvements are a direct result of enhanced maternal health and access to quality obstetric and neonatal intensive care. Birth weight remains the major risk factor for neonatal mortality. The past 2 decades have witnessed a number of significant advancements in neonatal care, most notably maternal administration of antenatal steroids, the ability to replace surfactant, use of inhaled nitric oxide (iNO), increased scientific evidence for routine practices, and superior equipment, such as ventilators and incubators. In addition, an increased number of neonatal conditions requiring intensive care are being recognized antenatally, which allows focused resuscitation and timely intervention by specialist teams. This is particularly relevant for neonates with congenitally malformed hearts, particularly premature infants, who represent the most critical and potentially vulnerable patients. Despite regionalized perinatal health care, from 10% to 30% of those born with extremely low weight ( Box 15.1 ) are delivered outside tertiary neonatal centers. Although overall survival for premature infants generally has improved, mortality remains high, particularly at the limits of viability ( Table 15.2 ). The outcome for neonates born outside tertiary centers is less favorable when compared with those patients delivered and resuscitated at perinatal centers specialized in coping with those at high risk. Survival varies by center and country, particularly at the very early gestational ages (<25 weeks), due to highly variable resources, approach to antenatal counseling, and resuscitation practices. The survival for infants less than 23 weeks of gestation remains very poor, with operative delivery and resuscitation not recommended in many centers. Survival with no or minimal disability for infants born at 23 and 24 weeks is 6% to 20%. Death in the first week of life is common, and delivery room mortality remains a concern. Survival at 25 and 26 weeks approaches 60% to 75% and 75% to 85%, respectively. Discharge without major morbidities occurs in approximately 30% of infants born at 25 weeks and 50% at 26 weeks. The contribution of cardiovascular performance and systemic hemodynamics to ongoing neonatal morbidity is poorly understood. Enhanced cardiovascular monitoring and earlier therapeutic intervention may prove to be a necessary step toward improving survival further and minimizing adverse neurodevelopmental sequelae.
| Maternal | Placental | Fetal | Miscellaneous |
|---|---|---|---|
| Preeclampsia Systemic hypertension Renal failure Diabetes mellitus Infection of the urinary tract Chronic disease |
Intrauterine infection, or premature rupture of membranes Placental abruption Antepartum hemorrhage Uterine stretch (multiple pregnancies, polyhydramnios, uterine abnormality) |
Chromosomal abnormality Fetal distress Hydrops fetalis Congenital infection (e.g., toxoplasmosis, rubella, cytomegalovirus) |
Cervical incompetence Idiopathic Familial |
Preterm: A neonate born prior to 37 weeks of completed gestation
Near-term: A neonate between the 34th and 37th weeks of gestation (subpopulation of preterm)
Low birth weight: A neonate born weighing <2500 g
Very low birth weight: A neonate born weighing <1500 g
Extremely low birth weight: A neonate born weighing <1000 g
Perinatal mortality rate: The number of stillbirths and early neonatal deaths, those occurring within 6 days of birth, per 1000 live births and stillbirths
Neonatal mortality rate: The number of neonates dying in the first 4 weeks, specifically within 27 completed days of life, for each 1000 live births
Intrauterine growth retardation: Growth parameters below the third centile for corrected gestational age. Asymmetric retardation is characterized by sparing of the head, the circumference of the head being greater than the third centile.
| Birth Weight (g) | Births (%) | Neonatal Mortality per 1000 Live Births in Each Subgroup |
|---|---|---|
| >2500 | 92.4 | 0.9 |
| <2500 | 7.6 | 48 |
| <1000 | 1.4 | 214 |
The condition of the infant at birth is dependent, in part, on intrauterine well-being and growth. Intrauterine growth retardation is the failure of the fetus or infant to achieve his or her predetermined genetic potential. Typically, the preterm infant is less than the third centile for weight, length, and head circumference. The consequences to the developing heart include cardiac hypertrophy, abnormal diastolic performance, and impaired vascular relaxation. Doppler interrogation of fetal and neonatal mitral valvar velocities revealed lower E wave amplitude compared with normal mature mitral E peaks. Impaired early left ventricular filling may relate to a diminished ability to relax and higher muscular stiffness. The implications may include impaired myocardial performance, hypertension, and hypotension. Poor glycemic control during pregnancy, particularly in the setting of maternal diabetes, is a known risk factor for structural heart disease and hypertrophic cardiomyopathy. In severe cases, where there is placental malfunction leading to retardation of growth, the same vascular and myocardial dysfunction may occur as described previously.
The preterm infant undergoes dramatic cardiorespiratory changes at birth, which coincide with improved lung compliance and termination of the placental circulation. These critical adaptive changes:
Include increased pulmonary blood flow, to approximately 20 times fetal levels
Occur in part due to the exposure of the pulmonary vascular bed to higher alveolar concentrations of oxygen than the relatively hypoxic intrauterine environment. Other metabolically active substances, such as metabolites of prostaglandin, bradykinins, or histamine, may play some role through inducing pulmonary vasodilation.
Include alteration in flow through fetal channels such as the arterial duct and oval foramen, which may last for many days. The major change in flow through fetal channels is either a direct result of increased flow to the lungs or improved systemic arterial tensions of oxygen. Increased left atrial pressure secondary to improved pulmonary venous return causes displacement of the flap of the oval foramen over the rims of the fossa, thus abolishing any right-to-left atrial flow. The pattern of flow through the arterial duct is significantly altered as lung compliance improves and pulmonary vascular resistance decreases. An increase in systemic vascular resistance also occurs once the compliant placenta is removed from the systemic circuit, and as a result of systemic vasoresponsiveness to increased tensions of oxygen. This will also contribute to increased transductal flow. The architecture of the arterial duct prior to term differs such that ductal tone is less responsive to oxygen, thus delaying closure and potentially contributing to excessive flow to the lungs and compromised systemic flow. The administration of surfactant can alter transductal flow significantly through reduced pulmonary vascular resistance. There is evidence of functional closure by 6 hours in some immature patients, although this is rare. Changes in transductal flow may have a major impact on end-organ perfusion; in particular, the relationship of augmented cardiac output on cerebral reperfusion hemodynamics and intraventricular hemorrhage is subject to recent investigation.
Include improved left and right ventricular outputs to meet the metabolic needs of immature neonate with insufficient thermoregulatory mechanisms and increased work of breathing. The transition from right to left ventricular dominance occurs over hours and is secondary to increased left atrial preload and left ventricular afterload. In total, there is a threefold increase in left ventricular output, which is necessary to meet the increased demands of the body. The enhanced ability of the left ventricle to increase its output is related, in part, to elimination of constraint by the pressure-loaded right ventricle.
Extremely preterm neonates represent a patient population highly vulnerable to morbidity and mortality in the immediate hours after birth. The resuscitation may be challenging, and delivery outside of a center with a specialized neonatal team with tertiary level neonatal intensive care is associated with a threefold greater risk of mortality or major morbidity. Resuscitation should be conducted according to the steps of the Neonatal Resuscitation Program, which is designed to meet the needs of these patients during this critical transitional period.
Temperature regulation during stabilization is important because preterm neonates may rapidly lose heat via evaporation of amniotic fluid, conductive loss through contact with cold surfaces, and convective loss into the relative cool air of the room. Several interventions have been demonstrated to improve temperature after stabilization including increase in ambient room temperature, occlusive polyethylene wrapping prior to drying, application of a polyethylene or woolen hat, and the use of heated, humidified ventilator gas. Specialized warming mattresses may be used. Close monitoring is important to avoid both hypothermia and iatrogenic hyperthermia.
Delayed cord clamping remains controversial, although it has become standard practice in some units. In lambs, early cord clamping is associated with a rapid decline in right atrial preload unless a ventilation-associated increase in pulmonary blood flow has occurred. Clamping the umbilical cord is associated with significant changes in cerebral blood flow and oxygen extraction that may be mitigated if ventilation is established prior to clamping. Human studies suggest that placental transfusion (delayed cord clamping or umbilical cord milking) is associated with a reduced risk of intraventricular hemorrhage, reduced frequency of blood transfusions, less hypotension, and decreased mortality as compared with immediate cord clamping. In spontaneously breathing preterm infants following an otherwise uncomplicated preterm birth, delayed cord clamping may be beneficial, although concerns have been raised about the impact on cerebral blood flow and requirement for postnatal resuscitation. There remains uncertainty as to the optimal management of nonvigorous preterm infants in whom delay in resuscitation may be detrimental.
Respiratory management in the delivery room focuses on attaining adequate functional residual capacity to promote pulmonary blood flow and oxygenation in the least invasive manner to which the preterm infant will respond. Preterm neonates are at risk of surfactant deficiency and retained fetal lung fluid, which contribute to poor lung compliance. In addition, these patients may have inadequate respiratory muscle strength to compensate. Spontaneously breathing preterm infants should have continuous positive airway pressure applied to help establish and maintain functional residual capacity if they demonstrate respiratory distress or work of breathing. Surfactant replacement is indicated for neonates where adequate recruitment requires high distending pressures or significant oxygen supplementation (typically greater than FiO2 0.3), particularly with classic findings of respiratory distress syndrome on chest radiography. Nonvigorous infants, those with heart rate less than 100 beats/min, and those with irregular breathing or apnea require positive-pressure ventilation and consideration for intubation according to the steps recommended by the Neonatal Resuscitation Program.
Resuscitation of the term infant should begin in room air because the most likely causes of hypoxemia are related to inadequate recruitment of functional residual capacity and not oxygen delivery. However, there is ongoing debate regarding the most appropriate gas for preterm infants. Studies comparing resuscitation using high oxygen concentration (65% to 100%) as compared with low oxygen concentration (21%) have been done; however, intermediate levels have not been studied. Exposure to high concentrations of oxygen may create undesirable effects such as oxygen free radicals, and initial resuscitation in 100% oxygen has not been shown to be beneficial for survival or the reduction in risk of chronic lung disease, retinopathy of prematurity, or intraventricular hemorrhage. Initial resuscitation using 21% to 30% oxygen is recommended. Once saturation monitoring is established, the use of an oxygen blender to titrate delivery to achieve saturations comparable with a term neonate at a similar age following birth is recommended.
Fetal myocardial tissue consists of 70% noncontractile tissue, compared with 40% in the mature adult heart. Histologic studies have shown that the myocytes making up the left ventricular myocardium are aligned circumferentially in the mid wall and longitudinally in the subepicardial and subendocardial layers of the walls. Studies of isolated myocardial tissue in fetal and adult lambs suggest that fetal myocardium is less compliant. Ventricular myocytes change considerably as they transition from fetal to postnatal life. The immature sarcomere and contractile apparatus is relatively disorganized. Myofibrils are irregular and scattered along the interior of the cell. Intrauterine and early postnatal cardiac growth is a combination of both hyperplasia and hypertrophy. Exposure of the developing rodent heart to dexamethasone led to cardiac hypertrophy, characterized by myocytes that were longer and wider, with increased volume. Biventricular hypertrophy is a recognized complication of exposure of the preterm myocardium to prolonged and high doses of steroids. Neonates born to mothers who had received a single antenatal course of steroids had higher systolic blood pressures and increased myocardial thickness, suggesting modified myocardial development. The nature of these changes may relate to earlier transition from a phase of hyperplasia to hypertrophy. The functional consequence of an enlarged hypertrophic myocardium, with a reduced overall number of myocytes, is unknown.
In contrast to adults, immature myocytes lack transverse tubules, are smaller in size, and have a greater ratio of surface area to volume. They are more reliant on transsarcolemmal fluxes of calcium for contraction and relaxation. The high ratio of surface area to volume, and the subsarcolemmal location of myofibrils, support direct calcium delivery to and from the contractile proteins. The sodium-calcium exchanger is the major conduit for attachment of calcium to, and release from, the contractile elements.
The control mechanisms governing contraction and relaxation in the immature heart are poorly understood but thought to be substantially different from the fully mature heart. In the mature heart, graded control of release of calcium is related to so-called L-type activity, which triggers release from the sarcoplasmic reticulum. Graded control of release in immature myocytes is thought to be related to factors influencing the activity of the sodium-calcium channel. Recently isoproterenol-induced β-adrenergic stimulation of sodium-calcium exchanger was identified in guinea pig ventricular myocytes. An improved understanding of factors that govern myocardial contractility and relaxation may facilitate more physiologically appropriate choice of therapeutic interventions in premature infants.
At physiologic heart rates, the immature myocardium shows a positive relationship, albeit that contractility falls with extreme tachycardia. Both the force-rate trajectory and the optimal heart rate reflect myocytic function and global myocardial contractile behavior. Developmentally, the immature myocardium has been shown to exhibit a higher basal contractile state and a greater sensitivity to changes in afterload. The intolerance of the immature myocardium to increased afterload may be attributable to differences in myofibrillar architecture, or immaturity of receptor development or regulation. The Frank-Starling law appears less applicable to the immature myocardium.
The consequences of hemodynamic instability include necrotizing enterocolitis, intraventricular hemorrhage, and periventricular leukomalacia, all of which may lead to mortality or adverse neurodevelopmental outcomes. Intraventricular hemorrhage occurs in up to three-tenths of infants born with very low weight, most commonly in the first 7 hours of life. The origin of the hemorrhage is the germinal matrix, an immature network of capillaries highly susceptible to hypoxemia, hypercapnia, and altered cerebral blood flow. Periventricular leukomalacia is a loss of white matter in the watershed areas around the lateral cerebral ventricles secondary to hypoxic-ischemic injury. The infant born at very low weight is highly susceptible to such morbidities, necessitating focused cardiovascular monitoring and targeted intervention in a timely fashion.
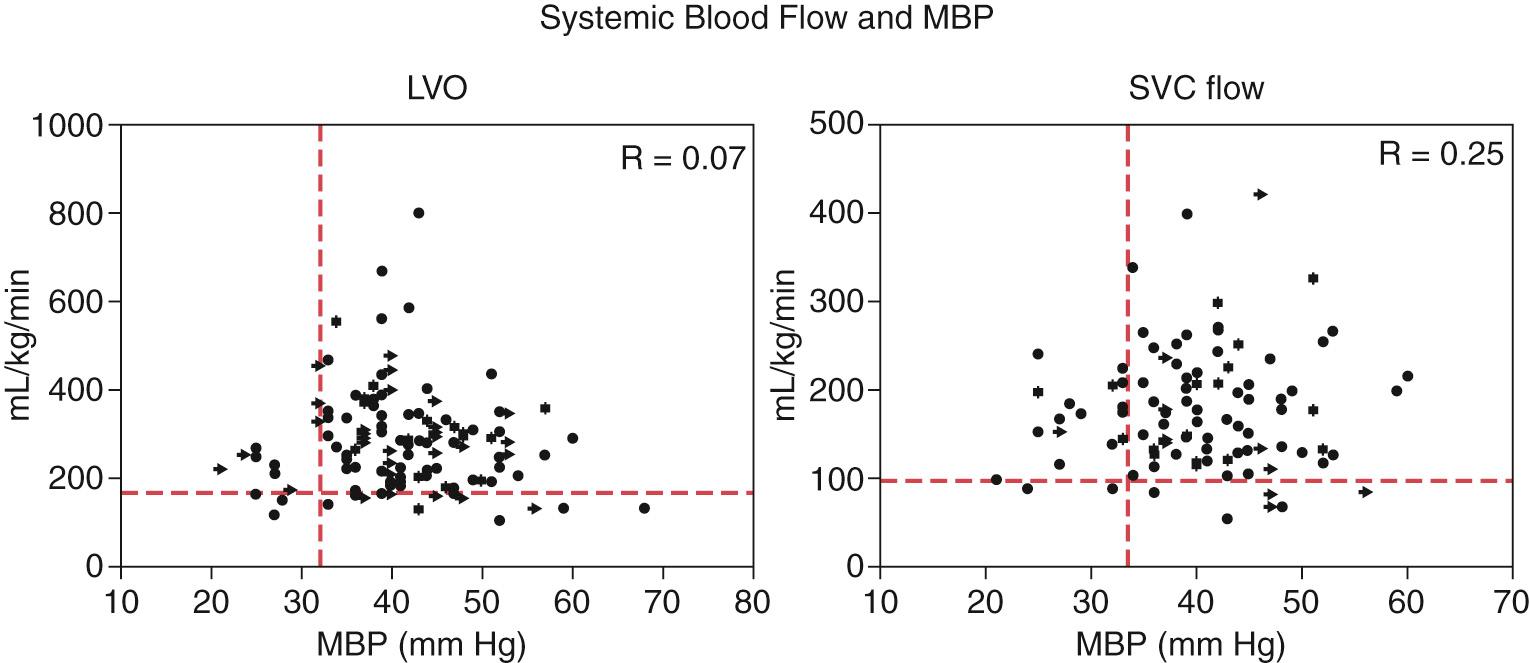
The determination of hemodynamic stability in premature infants is fraught with uncertainty, myths, and dogma without scientific validity. Suboptimal systemic blood flow is usually suspected on the basis of tachycardia, delayed capillary refill time, hypothermia, oliguria, altered blood pressure, metabolic acidosis, and increased levels of lactate in the plasma. Blood pressure readings are readily available at the bedside as a continuous stream of data from indwelling arterial lines, or periodically using a validated oscillometric cuff method. The approach to monitoring and guiding therapeutic intervention has relied on using mean arterial pressure as a surrogate of the adequacy of tissue perfusion and oxygenation. This reasoning is based on an assumed proportionality between blood pressure and systemic blood flow. In 1992 a report from the former British Paediatric Association stressed the importance of monitoring blood pressure to guide early therapeutic intervention and thus prevent adverse neurologic sequelae. It was suggested that mean arterial pressure equivalent to the gestational age in weeks is adequate as a minimum value. The group also suggested the need to establish accurate normative ranges for systolic and diastolic blood pressure. Unfortunately, achieving a mean blood pressure equal to gestational age has now become dogma and the standard on which therapy is based. Normative centiles for systolic blood pressure that take into account both gestational age at birth and postnatal age have been developed but are rarely used. Monitoring blood pressure in isolation is problematic for a number for reasons. First, blood pressure is but one surrogate of circulatory stability. Second, the concept of numeric hypotension as mean blood pressure less than gestational age in weeks has not been validated against indexes of perfusion of end organs. Third, important changes in either systolic or diastolic blood pressure may be missed. The systolic pressure indicates the pressure generated by the left ventricle and is therefore reflective of cardiac output ( Fig. 15.1A ). Diastolic pressure reflects global vascular resistance and local perfusion of the tissues (see Fig. 15.1B ). In neonates with a hemodynamically significant arterial duct, diastolic pressure is oftentimes compromised in isolation of changes in mean arterial pressure. This may have an unappreciated adverse effect on coronary arterial perfusion and subsequently on myocardial performance. The relationship between mean blood pressure and cardiac output is also weak ( Fig. 15.2 ). The finding of neonates with numeric hypotension but no clinical or biochemical signs of systemic flow, and conversely patients with normal or high blood pressure but signs of circulatory compromise, is not uncommon. It must be recognized that blood pressure is but a surrogate of perfusion and not the end point of interest. Although mean arterial pressure may be a guide to cardiovascular health, clinicians should pay attention to systolic and diastolic pressure when making decisions regarding the most appropriate intervention.
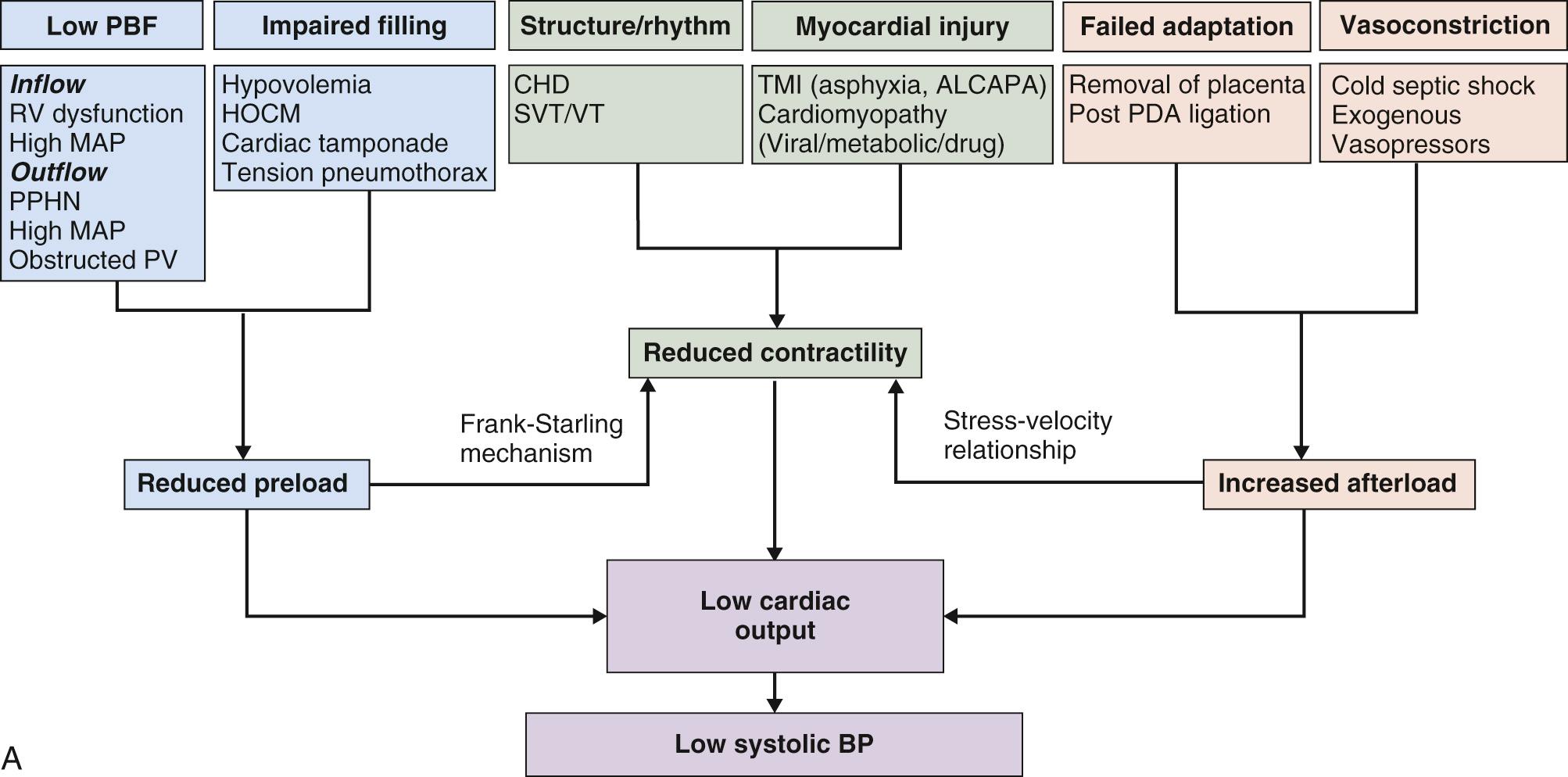
The rationale for treating hypotension is based on two important considerations. First, the cerebral circulation becomes pressure-passive below a critical level for blood pressure ( Fig. 15.3 ). The autoregulatory mechanism is thought to fail below a mean arterial pressure of 30 mm Hg. There is also evidence suggesting that neonates with hypotension have impaired cerebral oxygenation, as determined by near-infrared spectroscopy, and are at increased risk of intracranial hemorrhage or periventricular leukomalacia. Other investigators have shown no relationship between blood pressure and cerebral blood flow. Second, associations have been shown between adverse neurologic consequences and systemic hypotension. There is a significant body of evidence, nonetheless, which challenges these assumptions. For example, there are data suggesting that the association of hypotension to injury to the white matter and adverse neurodevelopmental outcome is not one of cause and effect, but an epiphenomenon. Studies with superior designs and larger numbers have failed to demonstrate any positive association between blood pressure and adverse neurologic outcomes. When corrected for associated risk factors, such as intrauterine growth retardation, postnatal use of steroids, and chronic lung disease, the association between hypotension and abnormal neurodevelopmental outcomes was lost. The discrepancy between individual studies may reflect the fact that the association is much more complex than any direct effect of blood pressure on cerebral blood flow ( Fig. 15.4 ). There may be concurrent changes in cardiac output and regional differences in flow of blood independent of blood pressure that are influencing cerebral perfusion, but these studies have not been performed.
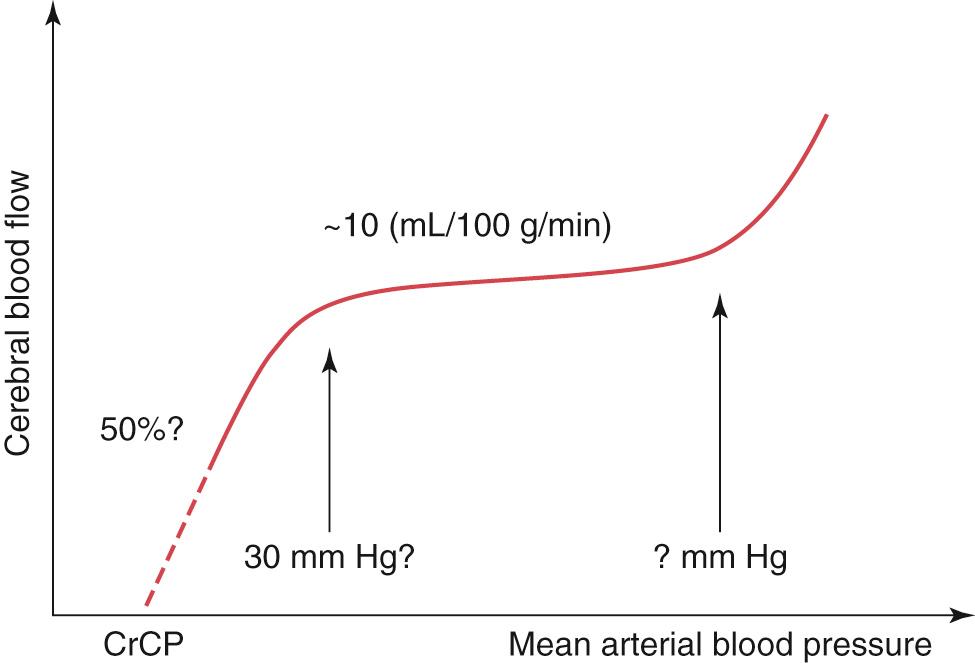
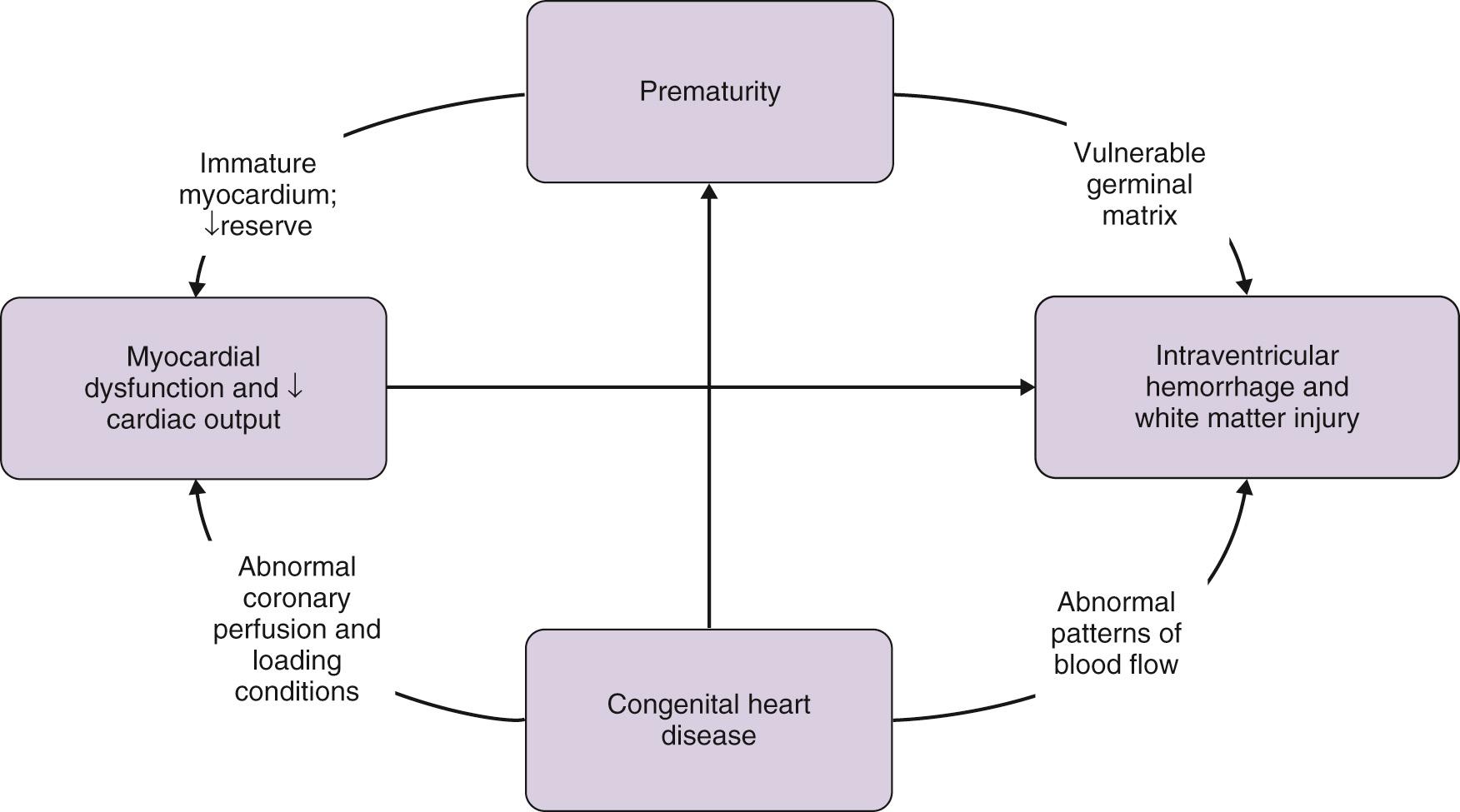
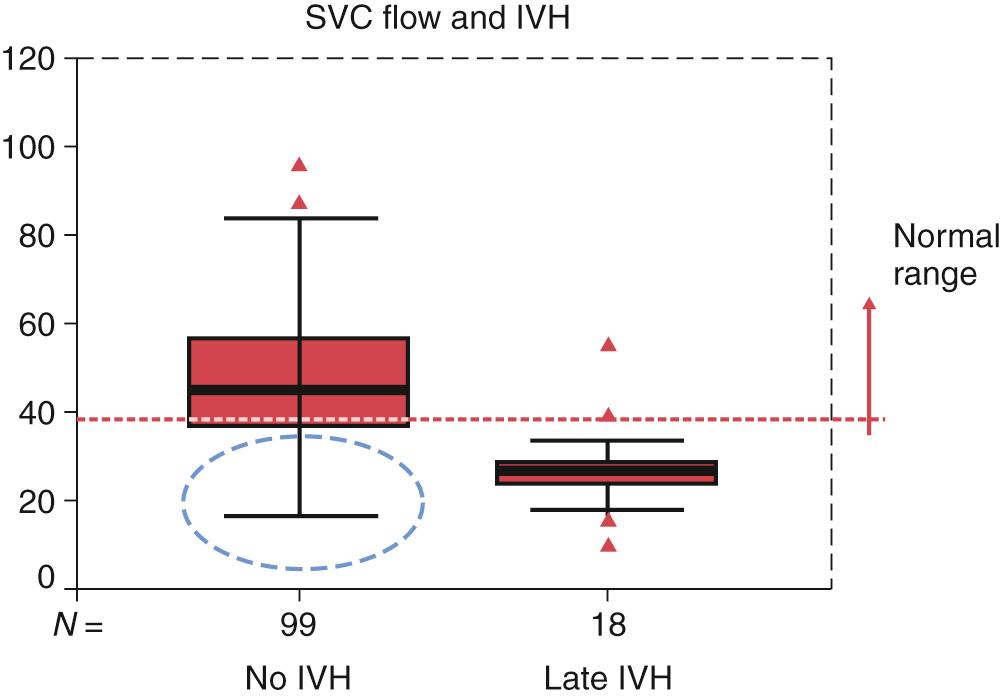
Failure of the neonatal transition may lead to myocardial dysfunction, low cardiac output, and hypotension, which may compromise perfusion of the end organs with consequent damage. The vulnerability of the cerebral circulation in the first 72 hours of life increases the likelihood of injury to the brain more than any other organ. It is essential that the systemic flow be monitored adequately at all stages. Tachycardia and capillary refill time are poorly validated and nonspecific measures of systemic flow. In isolation, capillary refill time is inaccurate, highly subjective, and a poor overall predictor of the adequacy of perfusion. The measurement of cardiac output at the bedside is a useful adjunct to the clinical assessment, and there are normative data for both right and left ventricular outputs. The normal range for cardiac output in normal premature infants is between 170 and 320 mL/kg per minute. These measurements should be interpreted in context in the early neonatal period due to the effects of transductal shunting. Left ventricular output reflects flow to the central nervous system because the cerebral circulation is preductal, and its accuracy has been validated using cardiac magnetic resonance imaging. Measurement of superior vena cava flow has been proposed as an alternative method of assessing the adequacy of systemic flow, because it is not confounded by atrial or ductal shunts. Although cardiac magnetic resonance imaging data have raised some questions about measurement accuracy, the relationship between superior vena cava flow and outcomes shows a consistent trend. Reduced flow in the superior caval vein is common in premature infants in the first 24 hours, reaching a nadir between 8 and 12 hours, which coincides with increased systemic vascular resistance. Neonates with the lowest flow are at greatest risk of intraventricular hemorrhage ( Fig. 15.5 ). When 3-year neurodevelopmental assessment was performed, low superior caval venous flow remained significantly associated on multiple logistic regression analysis, when adjusted for gestation and birth weight, with an abnormal developmental quotient and the combined end point of death and abnormal developmental quotient. Both blood pressure and systemic flow are important determinants of the likelihood of altered perfusion, and neither should be monitored nor treated in isolation, without consideration of the influence of the other. Decisions about circulatory adequacy should include a comprehensive assessment of systemic perfusion, and echocardiography assessment of cardiac output may be an invaluable adjunct tool. Other bedside tools such as near-infrared spectroscopy, noninvasive cardiac output monitoring, and heart rate variability have been explored in selected patient populations and may continue to evolve into additional adjunctive monitoring modalities, although further investigation is needed.
Patency of the arterial duct is a common problem in preterm babies, especially those born with extremely low weight. Although functionally essential for the normal fetal circulation, persistent ductal patency may have significant effects in preterm infants that include pulmonary overcirculation and systemic hypoperfusion. Persistent patency is found in approximately half of babies born at less than 29 weeks’ gestation and/or weighing less than 800 g.
Ductal closure is not immediate, particularly in infants born with extremely low weights, and occurs in two stages. Functional closure, which is a dynamic process that may be reversed if the ambient conditions change to favor patency, depends on the vasoconstricting action of humoral and biochemical factors on the muscular layer of the duct. This constriction results in the development of a zone of profound hypoxia in the media, which is the sentinel stimulus for irreversible closure. Anatomic closure depends on the architectural remodeling of the ductal wall. It consists of extensive neointimal thickening, and loss of smooth muscle cells from the inner media. The remodeling effects start at the pulmonary end, progressing toward the aortic insertion. Both vasodilator prostaglandins, especially PgE 2 and nitric oxide, oppose ductal closure during fetal life. In the second trimester, intimal cushions are formed that closely resemble the pathologic intimal thickening seen in atherosclerotic disease. The media is supplied with oxygen from either the lumen or its mural vessels. The thickness of the avascular zone, adjacent to the lumen, plays a critical role in determining the degree of hypoxia and subsequent remodeling of the ductal wall. Constriction of the circumferential and longitudinal muscle in the ductal wall leads to compaction, increased avascular thickness, and limits luminal supply of oxygen to both the avascular zone and the medial muscle. The resultant hypoxia induces expression of vascular endothelial growth factor or cell death, depending on its severity. The geographic distribution of expression corresponds with the distribution and intensity of mural hypoxia. The biologic consequences of these changes include a decline in tissue distensibility and increased contractile potential. The ductal wall of fetuses during late gestation has a high level of intrinsic tone, which is further increased after delivery by unopposed oxygen-induced contractile forces. After delivery, the increase in arterial content of oxygen, along with the decrease in circulating prostaglandins following placental separation, and reduced intraluminal blood pressure, contribute toward ductal closure. As transductal flow decreases, the wall becomes progressively more ischemic and eventually fibrotic.
The duct remains patent in up to four-fifths of infants born prior to term and weighing less than 1200 g. Such infants have no mural vessels in the medial layer and are nourished entirely via transluminal diffusion or from adventitial vessels. The immature duct, when studied experimentally, has also been shown to have less intrinsic tone and lacks both intimal folds and circumferential medial musculature. It is less responsive to oxygen and more sensitive to prostaglandin E 2 and nitric oxide. It is possible for the immature infant to develop comparable hypoxia in the medial muscle but only if transluminal flow is completely obliterated. Even when the duct constricts, profound hypoxia in the medial wall and anatomic remodeling fails to develop. A progressive increase in levels of nitric oxide synthetase in the ductal mural vessels after the first 15 days of life makes the preterm duct even less sensitive to prostaglandins. Nonsteroidal antiinflammatory agents therefore are less likely to be effective. In baboons, coadministration of an inhibitor of nitric oxide synthase, along with indomethacin, leads to increased contractility and luminal obliteration of the preterm duct. Gestational age may impact on the response to nonsteroidal antiinflammatory agents, although the evidence for this is limited. Gestational age less than 33 weeks at treatment was associated with greater likelihood of response to indomethacin in one small study, although echocardiography was not used universally. Advanced gestational age has also been associated with a reduced likelihood of response to second course indomethacin in those infants who have had a persistent hemodynamically significant ductus arteriosus after one course of nonsteroidal antiinflammatory therapy. However, other studies have identified a greater likelihood of response in infants of older gestational age. It is likely that other ambient conditions have a significant impact on response to indomethacin regardless of gestation. The presence of infection, prenatal exposure to maternal medications such as indomethacin tocolysis or magnesium sulfate for prevention of intraventricular hemorrhage, and platelet count are some factors that have been implicated.
It is important to emphasize the difference between pulmonary artery pressure and pulmonary artery resistance. When there is an anatomically large communication between the aorta and pulmonary artery, the pressure will be equal in each. However, the net flow through this communication is dependent on the differences between the systemic and pulmonary vascular resistance. Commonly, in clinical vernacular, “pulmonary hypertension” is used synonymously with elevated pulmonary vascular resistance; however, they are not the same. Pulmonary hypertension is defined as elevated pressure in the pulmonary artery: this can be seen when (1) there is an anatomically large ductus or ventricular septal defect, where the systemic pressure is transmitted into the pulmonary vascular bed, and (2) when there is elevated pulmonary vascular resistance, which results in elevated pulmonary artery pressure relatively independent of the amount of flow into the pulmonary vascular bed. It is clinically important to distinguish between the two clinical scenarios.
The presence of a persistent ductus arteriosus may have widely varied clinical implications depending on the circulatory circumstances and the balance of pulmonary and systemic arterial resistance. A patent arterial duct may be pathologic in the setting of a marked difference between the systemic and pulmonary vascular resistance, where the net flow across the ductus is left to right and the volume of shunt is high, leading to the classical symptoms described subsequently. For neonates in whom the pulmonary and systemic resistances are approximately equal, the ductus arteriosus, regardless of its size, may have relatively small volume of shunt and be of minimal clinical significance. In situations where either pulmonary artery resistance is high (e.g., pulmonary hypertension) or systemic delivery of pulmonary venous return is poor (e.g., significant left ventricular dysfunction, or anatomic obstruction to systemic flow, such as in coarctation of the aorta, or hypoplastic left heart syndrome), the presence of an open arterial duct may be beneficial or even lifesaving. Echocardiography assessment of the ductus arteriosus should include both assessment of shunt volume and surveillance for anatomic or physiologic contraindications to ductal treatment before treatment decisions are made.
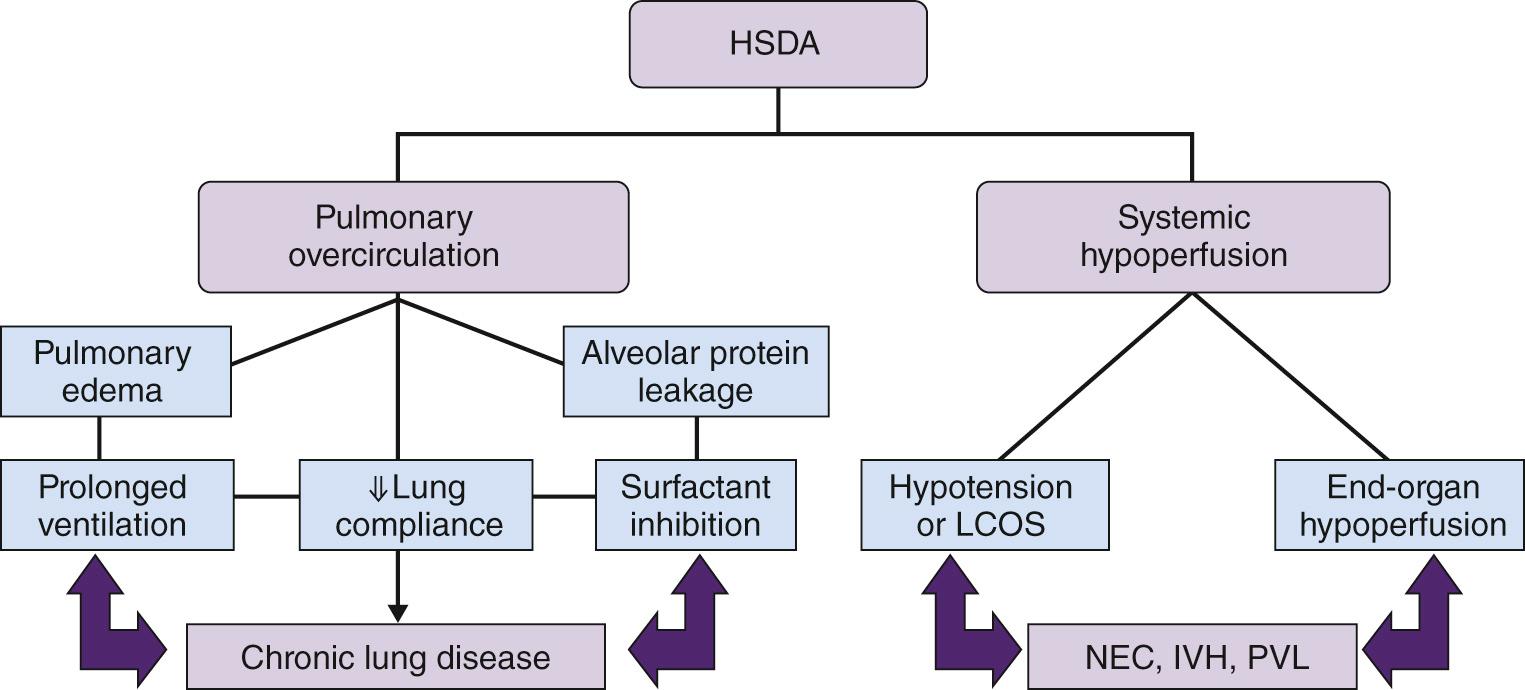
Failure of ductal closure, coinciding with the normal postpartum fall in pulmonary vascular resistance, results in a left-to-right transductal shunt. The consequences may include pulmonary overcirculation and/or systemic hypoperfusion, both of which may be associated with significant morbidity ( Fig. 15.6 ). The clinical impact is dependent on the magnitude of the shunt and the ability of the infant to initiate compensatory mechanisms. These infants are less capable of compensating and are prone to developing left ventricular failure, which may lead to alveolar edema and/or low cardiac output syndrome. The increased pulmonary flow and accumulation of interstitial fluid secondary to the large ductal shunt contribute to decreased lung compliance. The cumulative effects of increasing or prolonged ventilator requirements and myocardial dysfunction may increase the risk of chronic lung disease. Systemic flow may also be compromised with left-to-right ductal shunts due to retrograde diastolic flow in the aorta and the arteries supplying organs such as the kidneys and gut; this may be worsened by the effects of supplemental oxygen, hypocarbia, or both (see later). The redistribution of systemic flow is significantly altered even with shunts of small volume. Oftentimes there may be significant hypoperfusion to the kidneys and gastrointestinal tract before a hemodynamically significant duct is clinically suspected. This may lead to significant morbidity, including renal insufficiency, necrotizing enterocolitis, intraventricular hemorrhage, and myocardial ischemia. Early detection and targeted intervention may potentially improve long-term neonatal outcomes.
The classical clinical features include a continuous murmur, hyperactive precordium, bounding pulses, and wide pulse pressure. More commonly, a systolic murmur is audible that radiates widely across the precordium and back. However, in many of those born prior to term, cardiac auscultation is unremarkable. In the first week of life, despite the presence of a large duct, typical clinical signs are often absent. Such a situation is widely recognized as the silent duct, most likely due to continued elevation of pulmonary vascular resistance. Surfactant, by assisting the natural postnatal fall in pulmonary arterial resistance, has been shown to alter the timing of clinical presentation, specifically, by increasing the volume of the systemic-to-pulmonary shunt, which leads to an earlier clinical presentation. The existence of a hemodynamically significant but silent duct has been confirmed by cardiac catheterization and detailed echocardiographic evaluation. Such a situation should be suspected in a setting of delayed hypotension during the second and third days, failure of oxygenation, increasing requirements for ventilator support, or metabolic acidosis. The infant is more likely to present with both systolic and diastolic hypotension due to the inability of the immature myocardium to compensate for shunting at high volume throughout the cardiac cycle.
Although not very sensitive, chest radiography may show cardiomegaly and/or signs of pulmonary congestion, whereas the electrocardiogram may show signs of left atrial or ventricular enlargement. The latter may be more useful for the identification of subendocardial ischemia secondary to low coronary arterial perfusion pressures in neonates with a large duct, although this association has not been formally evaluated.
Echocardiography is the primary tool for assessment of the ductus arteriosus. Echocardiography confirmation of ductal significance prior to treatment is standard of care in many institutions due to the unreliability of clinical assessment, a desire to avoid the side effects of unnecessary medication, and the potential complications of indomethacin administration to neonates with duct dependent circulation (left-sided congenital heart disease [CHD]). The determination of ductal significance using echocardiography involves assessment of size, patterns of transductal flow, systemic and/or end-organ perfusion, and characterization of the degree of volume loading of the heart.
The size of the duct is obtained from a suprasternal short-axis view ( Fig. 15.7A ) using two-dimensional or color Doppler. A transductal diameter less than 1.5 mm is associated with retrograde or absent postductal aortic diastolic flow. A diameter of more than 1.5 mm resulted in a positive likelihood ratio of 5.5 and a negative likelihood ratio of 0.22 for prediction of the need for therapeutic intervention. In a prospective study of 116 neonates, transductal diameter was the most accurate echocardiographic marker in predicting clinical and hemodynamic significance. However, reliance on a single measurement may lead to error for several reasons. First, the measurement of internal ductal diameter may be difficult, even with clear two-dimensional images and the measurement using color Doppler may be influenced by gain settings. Second, the transductal diameter is not consistent throughout, often with tapering at the pulmonary end, and shunt volume is determined by the smallest diameter which may not be accurately identified depending on the imaging plane and both patient and operator factors. Third, the studies investigating the predictive value of ductal diameter were limited by small sample sizes. Finally, using an absolute cutoff does not consider the relationship between ductal size and infant size. Some studies have proposed indexing ductal and left pulmonary artery (LPA) diameter, although this approach may also be questionable, particularly in established shunts. A large ductus with high-volume left-to-right shunt may significantly increase flow in the branch pulmonary arteries, and this may result in LPA dilation and reduce the value of indexing.
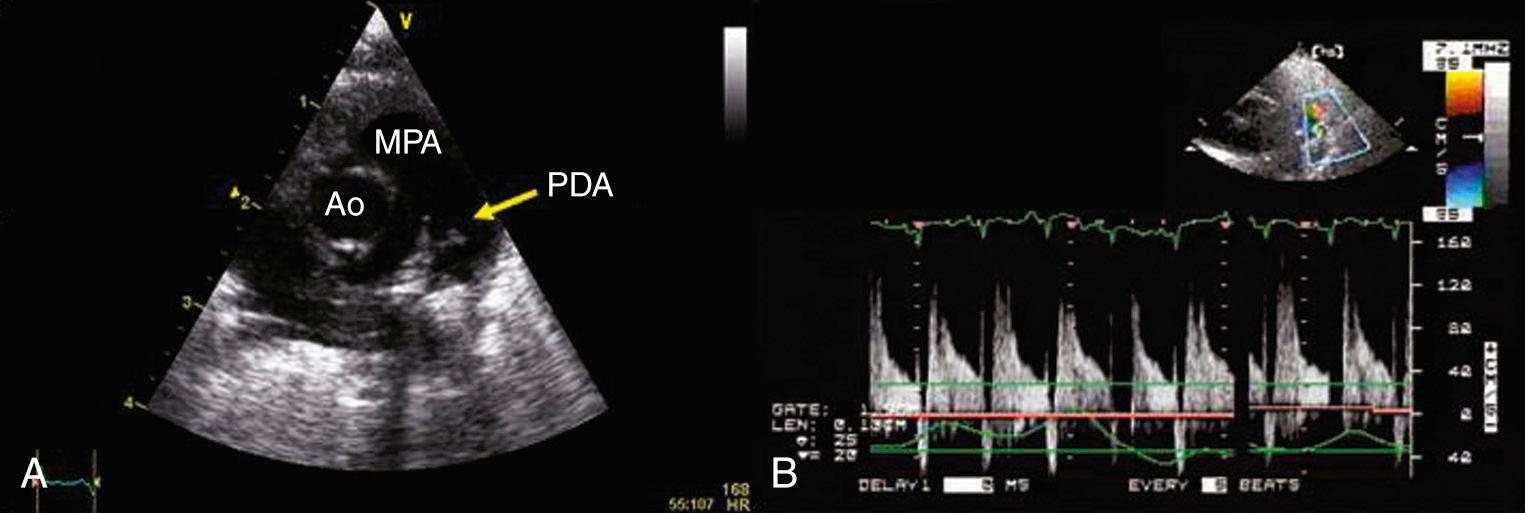
The pattern of transductal flow , estimated using pulse wave Doppler interrogation from a suprasternal short-axis view, can also be used to characterize ductal significance. High-velocity, continuous left-to-right flow is predictive of imminent functional closure, whereas a low-velocity pulsatile left-to-right flow pattern is likely to be clinically significant (see Fig. 15.7B ).
Cross-sectional echocardiography has also been used to quantify the degree of volume overload. Specifically, estimates of left atrial or left ventricular size have been used as surrogates of pulmonary overcirculation and/or volume loading. Although the measurement is standardized, it is not very specific and is prone to error dependent on the operator. The presence of a large atrial septal defect permitting left-to-right shunting will lead to further augmentation of pulmonary flow, potentially overestimating the magnitude of the ductal shunt.
Left ventricular output is significantly higher in preterm infants with a hemodynamically significant ductal shunt. Minimal angle of insonation with the left ventricular outflow tract in the apical five-chamber view is important to ensure accurate measurement.
Interrogation of descending thoracic aorta diastolic flow at the level of the diaphragm has been investigated using cardiac magnetic resonance imaging. Flow reversal during diastole is highly associated with shunt volume. Evidence of end-organ hypoperfusion may be also inferred from Doppler assessment of the patterns of flow in the mesenteric, cerebral, or renal arteries. Specifically, reversal or absence of diastolic perfusion is pathognomonic of a hemodynamically significant duct.
The aims of treatment are to reduce pulmonary overcirculation and improve systemic blood flow. The decision to treat is based on both clinical and echocardiographic findings, although the optimal time and method of ductal closure remain uncertain. Treatment should be classified as supportive intensive care strategies and therapeutic interventions aimed at closing the duct.
Strategies that minimize pulmonary overcirculation in a fashion comparable to that used for congenital cardiac defects should be considered. This can be achieved by accepting P co 2 between 45 and 55 mm Hg, arterial pH of 7.25 to 7.35, and oxygen saturations between 88% and 93%. Improvements in oxygenation and lung compliance may also be achieved by increasing the positive end-expiratory pressure to levels that maintain optimal recruitment, minimize atelectasis-induced lung injury, and lead to improvements in myocardial performance and cardiac output by reducing left ventricular afterload. Reduced hematocrit is associated with both lower pulmonary vascular resistance and decreased oxygen delivery to the tissues which may result in a compensatory increase in cardiac output and peripheral vasodilation. Avoidance of anemia in the presence of a hemodynamically significant ductus arteriosus may be beneficial.
The optimal treatment for hypotension and/or systemic hypoperfusion is strategies aimed at increasing pulmonary vascular resistance and closure of the duct and, in the absence of left ventricular dysfunction, not cardiotropic support. Excessive α-adrenergic stimulation, by agents such as dopamine or epinephrine, should be avoided because the increased systemic vascular resistance may lead to increased left-to-right shunting or may further compromise an already dysfunctional left ventricle. Dobutamine or newer inodilators currently under investigation, such as milrinone, may be preferred if there is associated left ventricular dysfunction, although medications that reduce systemic vascular resistance (e.g., milrinone) should be avoided in neonates with low diastolic arterial pressure because further reduction may compromise coronary artery perfusion pressure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here