Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Older reduction tip rhinoplasty techniques are effective in altering tip contour and definition, yet they depend on aggressive cartilage resection, morselization, and sacrifice of tip supports to achieve these goals. Weakening of the crura in this manner, when subjected to long-term forces of contracture, may lead to tip distortion and commonly seen postrhinoplasty deformities. Beginning in the 1980s, advancements in understanding of nasal tip anatomy and dynamics allowed for technical innovations in tip alteration that emphasize more conservative handling of the tip while better preserving structural support and functional integrity. Despite these developments, the incidence of revision rhinoplasty remains considerable. Kamer, in a 1981 review, reported rates of revision rhinoplasty in the range of 8% to 15%, while more recent reports place the incidence closer to 5% in the hands of experienced surgeons. The senior author (P.A.A.) previously reported a 6% revision rate in a cohort of his patients. The general decline in revision rates has been attributed in part to increasing acceptance and employment of open rhinoplasty approaches but may also be due to better public understanding of the need to choose experienced rhinoplasty surgeons when undergoing this procedure.
Residual and iatrogenic aesthetic deformities are the primary indications for revision; however, a functional deficit coexists in roughly two-thirds of patients. While the authors’ experience reflects a higher revision rate for mid-vault abnormalities, several studies spanning five decades suggest tip deformities are the leading reason for revision surgery. Failures of philosophy and ability to accurately diagnose and properly implement techniques during the primary procedure account for the patterns of deformities seen. Even when accurate diagnosis is possible, the capacity to execute surgical goals may be diminished in revision surgery for several reasons: (1) tip anatomy is typically distorted, (2) tip supports are often compromised, necessitating augmentation procedures, (3) aesthetic goals are sometimes supplanted by functional needs, and (4) the skin envelope is often scarred and inelastic, rendering redrapage unpredictable and less forgiving.
This chapter will discuss the most frequently seen postrhinoplasty lobule deformities and summarize indications and techniques for their correction.
The techniques available for manipulation of the nasal tip are widely known. Yet, the challenge is in knowing when to apply specific techniques to achieve the appropriate correction. Another way of looking at this is that the surgeon must have both a clear aesthetic understanding of the surgical goals as well as the technical expertise to recognize which procedures will achieve them.
In the revision scenario it is especially important to have a clear conceptual framework with which to create a surgical plan. The Tripod Concept, first advanced by Jack Anderson, M.D., is widely taught in training programs and still represents a useful algorithm for nasal tip reduction. However, the Tripod Concept was conceived at a time when reduction tip rhinoplasty using a closed technique was the norm. Thus, it does not provide for understanding of techniques for achieving greater projection or for better understanding of the need for tip stabilization in open cases. In addition, the Tripod Concept predates the further characterization of the intermediate crura, and so it does not address the effects of alteration of this structure to achieve refinement of the lobule.
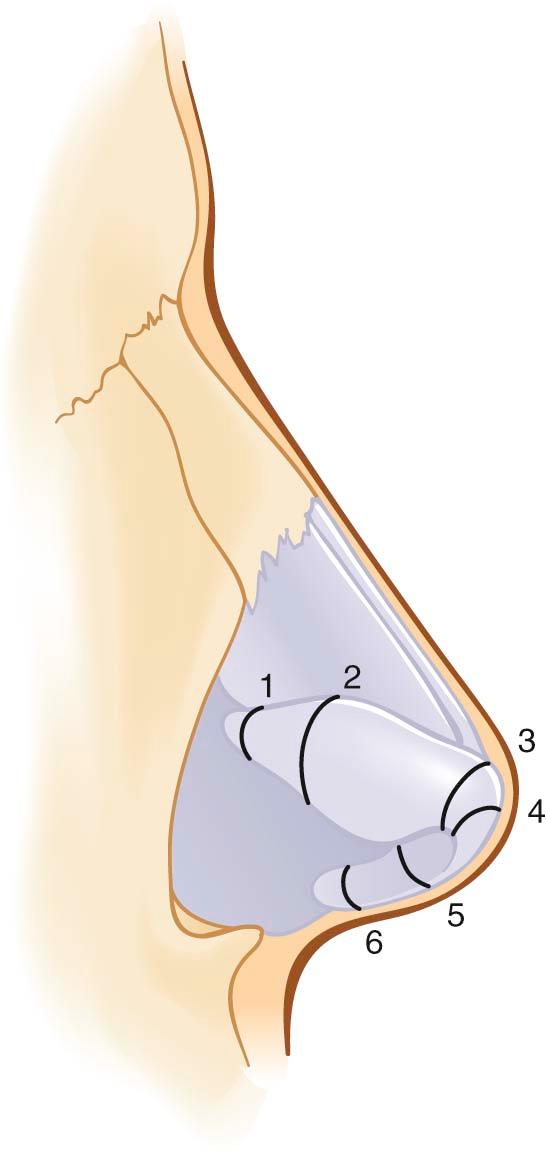
A contemporary model of nasal tip dynamics, termed the M-arch model, has been proposed in an effort to expand on the Tripod Concept ( Figure 20-1 ). This model views the lower lateral cartilages as paired parabolic cartilaginous arches having their vertices at the tip-defining points. The most significant determinants of tip-alteration are the overall length of the arch and the specific site of the alteration ( Figure 20-2 ). Shortening the arch in close proximity to the vertex will have a greater effect on deprojection (such as a vertical lobule division), while shortening by the same amount farther from the tip-defining point will have a greater influence on rotation (such as a lateral crural overlay technique). Furthermore, shortening of the arch lateral to the tip-defining point serves to deproject, rotate, and shorten the nose, whereas shortening medial to this point will deproject, counterrotate, and lengthen the nose.

The same principles may be applied to understanding of the relative effects of arch-lengthening maneuvers such as suture or tip-grafting techniques. Suture techniques such as the lateral crural steal effectively increase the vertical arch segment by borrowing length from the more horizontal segment just lateral to the tip-defining point. Lobular grafts, on the other hand, achieve improvements in projection by adding apparent length or vertical height to the M-arch. In our practice, columellar struts are routinely used to stabilize the length and strength of the medial crura and thereby uphold the nasal tip projection without, in and of themselves, actually increasing arch length.
The M-arch model allows for application of specific arch-altering maneuvers to achieve simultaneous predictable changes in nasal length, projection, rotation, and tip definition. Division at the medial crural feet will generate tip deprojection and some counterrotation and may be used to diminish excessive flaring of the medial crural footplates if the soft tissue attachments between the footplates have been released. Division in the mid-medial crus may be used to adjust columellar asymmetries, in addition to providing counterrotation and deprojection. Division at the angle or junction of the medial and intermediate crus will yield primarily tip deprojection and vertical shortening and may also diminish a hanging infratip lobule. Division within the intermediate crus or at the dome will deproject the tip and engender greater acuity of the domal arch, thus producing lobular refinement. Asymmetric division in this region may be used to improve lobule symmetry with sutures concealed within the infratip. Division in the mid-lateral crus, known as a lateral crural overlay, represents the most powerful maneuver for obtaining rotation along with deprojection. Finally, division at the hinge area will achieve mild tip deprojection and rotation. This setback technique is preferred when lobular contour is acceptable; however, this is rarely the circumstance in revision tip surgery. Furthermore, occasionally it can lead to crural in-flaring and obstruction within the vestibule, so we avoid this maneuver if possible. In our practice, the vertical lobule division and lateral crural overlay are the workhorse techniques for obtaining the desired alterations in major nasal parameters.
Vertical arch manipulations represent extraordinarily powerful techniques for achieving predictable changes in lobular contour. In fact, it is the experience of the authors that such techniques are the only reliable method for accomplishing meaningful modification of tip projection and rotation. Maneuvers that do not cause real or apparent changes in arch length cannot, therefore, achieve real or apparent changes in tip projection. By example, traditional methods for achieving changes in projection or rotation, such as full transfixion incisions, resection of the nasal spine, shortening of the caudal septum, and cephalic crural excision, among others, are not dependable options and most often are conducive to postrhinoplasty tip destabilization and pollybeak deformity.
Postrhinoplasty tip deformities can be categorized as those caused by either undertreatment or overresection of preexisting abnormalities. Persistent primary deformities comprise aesthetic problems that were not adequately treated during the primary procedure. These may be attributed to an oversight in diagnosis or failure to properly account for postoperative soft tissue healing. Common deformities include (1) a persistently overprojected or underprojected nasal tip, (2) a counterrotated or ptotic tip, (3) a wide, boxy, bulbous or asymmetric tip, (4) a discordant alar–columellar relationship, and (5) a broad or flared alar base.
By contrast, aggressive reductive efforts at primary surgery may give rise to the spectrum of overresected nasal tip deformities. Examples of these abnormalities include (1) an underprojected, collapsed tip, often in combination with a pollybeak deformity, (2) an overrotated tip, leading to a shortened nasal appearance, (3) an excessively narrowed, pinched tip, (4) alar-columellar contour irregularities caused by bossae formation, alar retraction or a hanging columella, or grafts that have become visible or palpable, (5) an aggressively narrowed alar base, and (6) external soft tissue irregularities caused by excessive soft tissue thinning or unsatisfactory scar formation. Associated functional consequences may typically include external valve collapse, caudal septal instability, and vestibular stenosis.
The desirable revision tip rhinoplasty candidate has a clearly defined and realistic complaint. One must remember that the degree of subjective concern that a patient experiences bears no direct relationship to the objective severity of the defect. Thus, reasonable distress over a minor deformity is not, as such, a contraindication to surgery. Equally important, the defect must be technically treatable in the surgeon's hands. The quality of cutaneous health and vascularity should be used as the yardstick to measure technical suitability rather than the absolute number of prior surgeries. A patient with a real, definable complaint and a history of four prior rhinoplasties may be a reasonable revision candidate, whereas a patient having had only one prior procedure may be a poor candidate in the presence of severe scarring or vascular compromise.
A sound rapport must be developed with the prospective patient, one that will weather potential postoperative problems. The patient must be medically fit and psychologically prepared for yet another surgery. He or she must clearly understand and accept the likely range of outcomes, the limitations, and risks of surgery. In our own practice, we apply the above selection criteria stringently before embarking on revision surgery.
While technical preferences vary from surgeon to surgeon, most experienced revision rhinoplasty surgeons today prefer the open approach for revision tip surgery because of the undistorted exposure it affords. We believe that open rhinoplasty is the approach of choice for both primary and revision cases unless an equivalent improvement can be obtained with a closed approach. This is seldom the case in our estimation. It is our perception that closed revision rhinoplasty approaches more often result in common postrhinoplasty deformities such as persistent overprojection, underrotation, tip asymmetry, contour deformities from graft distortion and migration, and soft tissue irregularities owing to a compromised plane of dissection, as well as bossae and pinched tip formation resulting from overly aggressive resection. The open approach offers distinct, well-described advantages in the form of more precise dissection, careful exposure and diagnosis of complex deformities, accurate measurement of proposed tip-altering maneuvers, and suture stabilization of both native cartilage as well as grafts. The avoidance of vestibular incisions near the internal nasal valve will also decrease the likelihood of incipient valve obstruction or vestibular stenosis postoperatively, which is more common following revision rhinoplasty.
Our preferred incision is the midcolumellar, inverted gull-wing design. If planned and closed carefully, this incision rarely, if ever, is cause for scar revision. If open rhinoplasty was performed previously, we will incise through the existing scar unless it is unfavorable, in which case it is revised. We routinely elevate the columellar flap following this incision, while the marginal incisions are made during scissor dissection over the domes and lateral crura. This permits more accurate identification of the crural margins. Occasionally, severe scarring may necessitate first making the marginal incisions, followed by retrograde dissection over the domes. We elevate as much as possible in the supraperichondrial plane, thereby maintaining scarred soft tissue on the flap. This helps to preserve flap vascularity and to prevent “buttonholing,” and it better delineates the residual extent of the alar cartilages. At times, one may find that infiltration of the scar tissue with local anesthetic can aid in hydrodissection.
Extreme care must be exercised in multiple revision cases since thick scar tissue often complicates the dissection. Those surgeons who routinely perform revision rhinoplasty need not be told of how difficult this dissection can be. Alar cartilage remnants may be abnormally thin, tenuous, and easily penetrated by an excessively deep dissection. In fact, scar tissue is sometimes the only tip support remaining in the severely deformed tip. Similarly, the subdermal plane may be filled with scar, predisposing to dermal ischemia with an overly shallow dissection. The safest initial approach in the heavily scarred patient may be to leave a rind of scar tissue on the crura. This can be further painstakingly dissected and excess scar tissue may be discarded or saved for soft tissue augmentation elsewhere. To compensate for the thick, inelastic skin that is often encountered in a revision case, it is necessary to undermine the soft tissue envelope widely to encourage favorable redrapage. Once the tip and dorsum have been adequately exposed, precise corrective maneuvers may be undertaken.
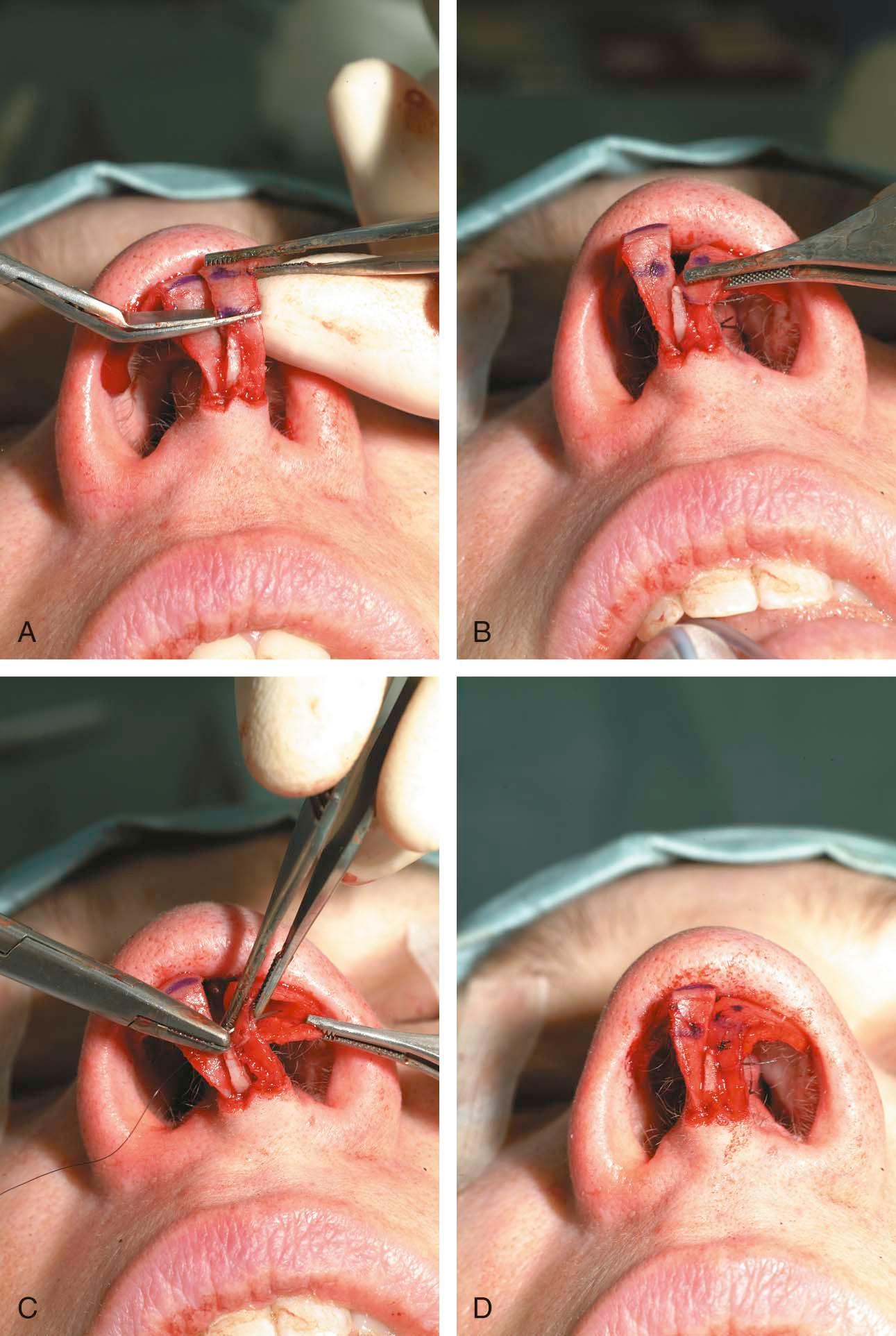
Prior to any division, the cartilage is extensively released from vestibular skin in the surrounding region to allow for cartilage advancement. The location for arch division is chosen in accordance with the desired alterations in tip dynamics. The cut ends of cartilage are then overlapped from 2 mm up to 6 mm in some cases and are secured with 6-0 nylon mattress sutures. Two buried sutures are placed in every case, the first to set the length of overlap, and the second to set the longitudinal axis of the neoarch. Alternatively, 4-0 Vicryl sutures may be used in the lateral crus to fixate the cartilage segments through the underlying vestibular skin. This is sometimes preferred since it may be technically challenging to bury sutures in this location. Overlapping suture fixation is a critical component of this technique in order to avert inflaring or collapse of the arch upon contraction of the skin–soft tissue envelope. In general, the cartilage segment closest to the tip-defining point represents the overlying segment when overlapped ( Figure 20-3 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here