Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Probiotics are live microorganisms that, when consumed in adequate amounts by an adult host, are believed to and in many instances have been shown to confer health benefits.
The best-known probiotics belong to the genera Bifidobacteria , Lactobacillus , and Saccharomyces .
Extensive clinical evidence indicates that probiotics can reduce the risk of necrotizing enterocolitis (NEC) and late-onset sepsis in term and very low birth weight infants. Further work is needed to ensure safety in extremely low birth weight infants.
The baseline incidence of conditions such as NEC and other inflammatory conditions is an important consideration in deciding whether to initiate the administration of probiotics in a neonatal intensive care unit.
Several probiotics dampen inflammation by inhibiting TLR4 and TLR2 and by stimulating expression of antiinflammatory mediators. Several probiotics improve intestinal barrier function by strengthening the mucus layer and tight junctions between enterocytes. Many probiotics increase energy harvest by producing short-chain fatty acids, amino acids, vitamins, and secondary bile acids.
Many probiotics alter the intestinal microbiota by selectively competing for human milk oligosaccharides and by producing bacteriocins.
Probiotics are live microorganisms that, when consumed in adequate amounts, are believed to and in many instances have been shown to confer health benefits in adult hosts. In older children, the gut microbiome is relatively stable and the addition of probiotics can potentiate intestinal homeostasis, nutrition, and mucosa immunity. However, in neonates, particularly in the extremely low birth weight (ELBW) ones, early introduction of probiotics evokes debate. The proponents who advocate for the administration of probiotics emphasize that these agents could neutralize the dysbiosis associated with the acquisition of hospital-acquired gram-negative flora. Probiotics may not be natural, but neither are the nosocomial gram-negative bacilli. The opponents argue that the sequential appearance of gram-positive and gram-negative bacteria and anaerobes in the neonatal intestine at specific stages of development might have a natural rationale that we might not quite understand yet. They emphasize that the intention might be to promote health, but the safety of administering live bacteria in ELBW infants is not assured; recall that these bacteria may have caused sepsis-like illness in some infants. The opponents question that the administration of live bacteria, even if apparently advantageous in mature adults and in many premature infants, could still be an underappreciated mistake in some that might not necessarily fix an earlier mistake that enabled the overgrowth of potentially harmful bacteria.
In neonatal intensive care units (NICUs), families now increasingly ask clinicians whether they should be adding probiotics to the feedings of their premature or critically ill infants, and if so, for help in choosing products. These questions create a dilemma, given that none of the currently available probiotic preparations are recognized as therapeutic agents. These are perceived as dietary supplements, and there is indeed some room for criticism of the scientific rigor and the “number needed to treat.” Our neonatologists, pediatricians, and allied personnel long for guidance for these questions.
In this chapter, we have summarized the current information on the types of probiotics, available pharmaceutical preparations, effects, likely mechanism(s) of action, and evidence that favors and negates the impact of probiotics. Wherever possible, we provide evidence-based information to guide both clinicians and parents about the potentially protective effects of probiotics against necrotizing enterocolitis, sepsis, and other inflammatory conditions. In areas where sufficient evidence is available, we have tried to include information on the individual probiotic strains or combinations that may be effective and the clinical contexts that warrant further research. We have included a brief section on prebiotics and synbiotics, because those are perceived by many as potentially safer. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the quality of evidence.
The International Scientific Association for Probiotics and Prebiotics defines probiotics as live microorganisms that confer a health benefit to the recipient when administered in adequate amounts. This definition does not include transplant of fecal microbiota or dead organisms. Many probiotic species are known and are commercially available ( Table 18.1 ). Many probiotics have been accorded the GRAS (generally recognized as safe) status by the Food and Drug Administration (FDA) in the United States and have been safely used in food based either on a history of use before 1958 or on published scientific evidence, and they need not be approved by the FDA before being used. Probiotics listed with GRAS status in the United States are listed in Table 18.1 ( https://www.fda.gov/food/generally-recognized-safe-gras/microorganisms-microbial-derived-ingredients-used-food-partial-list ).
| Bacillus coagulans GBI 30, 6086 (activated, inactivated, and spores) b |
| B. coagulans strain Unique IS2 spores preparation |
| B. coagulans SANK 70258 spore preparation |
| B. coagulans SBC37-01, spore preparation |
| B. coagulans SNZ1969 spore preparation |
| Bacteroides xylanisolvens strain DSM23964 |
| Bifidobacterium animalis subsp. lactis strain Bf-6 |
| Bifidobacterium breve M-16 |
| Bifidobacterium lactis strain Bb12 and Streptococcus thermophilus strain Th4 |
| Bifidobacterium longum BB536 |
| B. animalis subsp. lactis strains Bf-6, HN019, Bi-07, B1-04, and B420 |
| Carnobacterium maltaromaticum strain CB1 (viable and heat treated a ) |
| Lactobacillus acidophilus La-14 |
| L. acidophilus, Lactobacillus lactis, and Pediococcus acidilactici |
| L. acidophilus NCFM |
| Lactobacillus casei subsp. rhamnosus strain GG |
| L. casei strain Shirota |
| Lactobacillus fermentum strain CECT5716 |
| Lactobacillus plantarum strain 299v |
| Lactobacillus reuteri strain DSM 17938 |
| L. reuteri strain NCIMB 30242 |
| Lactobacillus rhamnosus strain HN001 |
| L. rhamnosus strain HN001 produced in a milk-based medium |
| Propionibacterium freudenreichii ET-3, heat killed a |
| Saccharomyces cerevisiae strain ML01, carrying a gene encoding the malolactic enzyme from Oenococcus oeni and a gene encoding malate permease from Schizosaccharomyces pombe |
| S. cerevisiae strain P1Y0, a variant of S. cerevisiae parent strain UCD2034 |
| Streptococcus salivarius K12 |
a The term “probiotic” is formally limited to live organisms.
b US Food and Drug Administration. GRAS notices. https://www.accessdata.fda.gov/scripts/fdcc/?set=GRASNotices . GRAS , Generally recognized as safe.
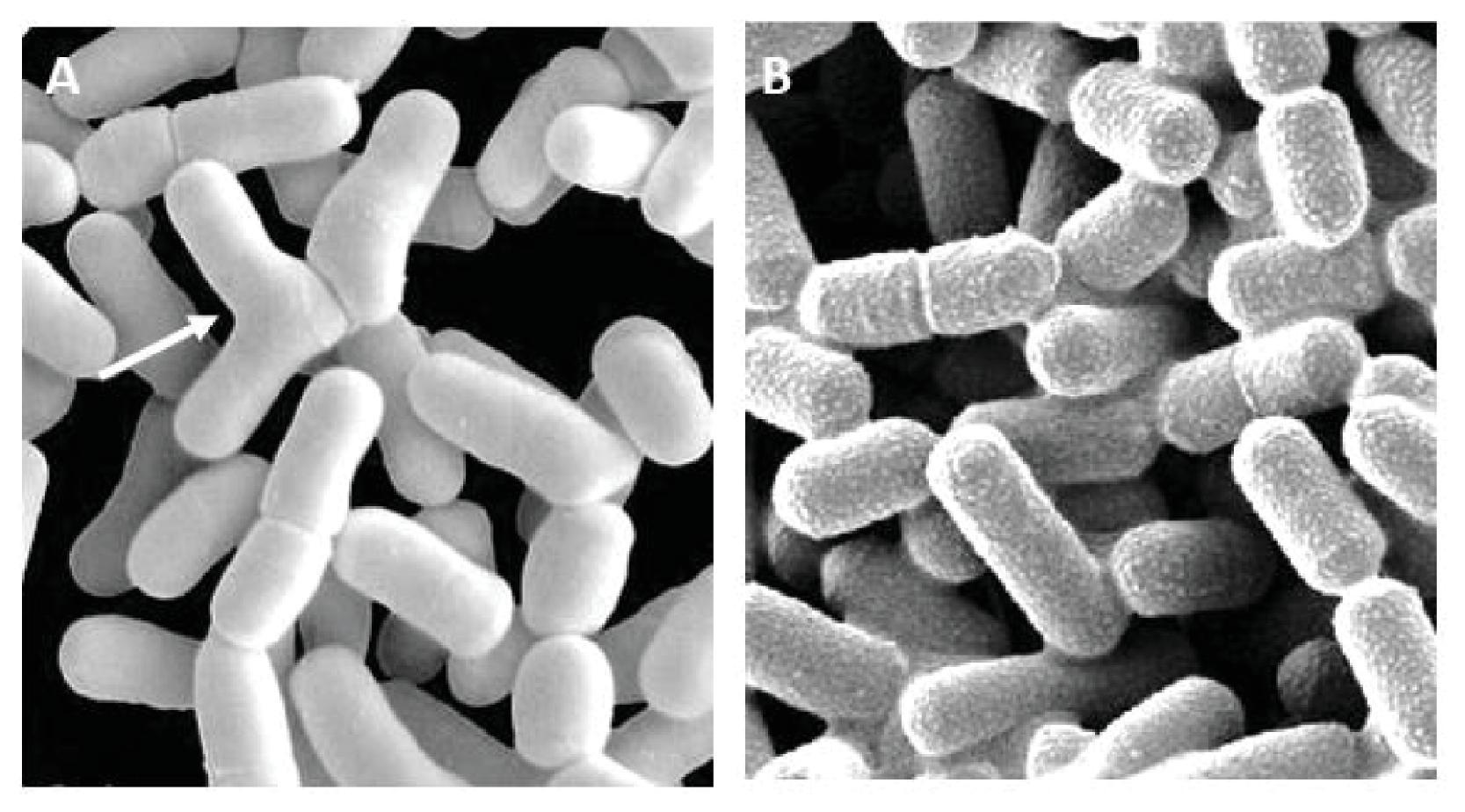
The best studied probiotic species are Bifidobacteria and Lactobacilli ( Fig. 18.1 ). A list of commercially available probiotic products can be easily found with a Google search using the search phrases “infant probiotics,” “probiotics for infants,” “commercially available infant probiotics,” and “commercially available probiotics infant.” The availability of specific products may differ by geographic region and the variety used in trials and observational studies to date, and no product(s) can be specifically recommended yet ( https://clinicaltrials.gov/ct2/show/NCT02472769 ; http://ibtherapeutics.com/the-phase-3-study-protocol-is-modified-after-ibts-meeting-with-the-fda/ ). Clinicians need to evaluate specific products for safety and efficacy.
A large number of probiotic preparations that are currently being marketed need more standardization. At least 30% of these formulations show discrepancies between the stated and actual number of viable organisms, the concentrations of the organisms, and/or the types of organisms compared with the product labeling. There is a need for a set of minimal manufacturing standards with clear guidelines for efficacy ( Table 18.2 ).
| Inadequate labeling about taxonomic classification of microbial names |
| Inadequate information about numbers of viable probiotic organisms |
| Inadequate information on shelf life of products |
| Inadequate guidelines for storage conditions needed to maintain probiotic viability |
| Inadequate information on labeling about dosing or toxicity |
In the United States, probiotics are classified as dietary supplements and are not subject to stringent regulatory processes, similar to therapeutic medicines. The production of probiotics is required to comply with Good Manufacturing Practice guidelines but not with testing standards for quality or efficacy. Similarly, in Europe, probiotics are regulated by the European Food Standards Agency at levels that are lower than those for medicines. Lewis et al. found that the contents of most bifidobacterial probiotic products differed from the ingredients list. Another observation is that most probiotic products contain a mixture of live bacteria with dead bacteria and their fragments. Hence the labeling information is not always accurate; dead bacteria and bacterial components can trigger immune responses. Many products may also contain contaminating pathogenic organisms, which is an important consideration in premature infants. There has been one death from mucormycosis associated with a contaminated probiotic product, and there have some reports of probiotic-associated sepsis. , , , There are some uncertainties as to which strain and dose is optimal in patients, owing to the heterogeneity in both clinical trials and implementation cohort studies. Until high-quality pharmaceutical-grade probiotic preparations (single-dose packaging, stable strains, and cross-tested against contaminants) are available, consideration must be given to analyzing each new batch of probiotics to quantify probiotic organisms by polymerase chain reaction and microbiological techniques.
Van den Akker identified 25 single-strain or combination products used in randomized clinical trials (RCTs) or studies that reported mortality, necrotizing enterocolitis (NEC), late-onset sepsis (LOS), or time to full enteral feeds. Three combination products reduced mortality, seven products (three single, four combination) reduced NEC, and two combination products reduced LOS. One combination product (L. acidophilus, B. longum, B. bifidum, B. infantis) used in two studies showed efficacy across all three outcomes. Earlier studies have compared single- and multiple-strain products, showing better results with multiple-strain products. It is not clear whether the effects are specific to strains, subspecies, species, or the genera. Some observational studies and national databases with varying products still show benefit, , suggesting that at least some of the clinical benefits are not likely to be strain specific. ,
Although the current definition of probiotics emphasizes that the bacteria are alive when administered to the host, nonviable organisms may also elicit beneficial immune responses. The term “paraprobiotic” or “ghost probiotic” is used for intact but nonviable cells or cell extracts. Bifidobacterium breve M-16 V, currently available and used by some units, has demonstrated suppression of proinflammatory responses from a heat-killed form in a mouse model. A systematic review in 2017 identified 19 pediatric trials of “modified” probiotics, none targeted at NEC or LOS and only one in neonates (targeting atopic dermatitis), but showed no improvement in the safety profile compared with live probiotics. However, given the anxiety caused by the administration of live bacteria in preterm infants, this line of study merits further exploration.
Probiotic microbes have been historically identified as food stabilizers. The microbial genera were associated with good health and have included Lactobacillus , Bifidobacterium, Escherichia, Lactococcus, Streptococcus, and Saccharomyces. These have shown resistance to gastric acid, bile acids, and intestinal enzymes. In neonates, the earliest studies examined probiotics for prevention of NEC. In one of these, all infants admitted to a NICU in Bogota, Colombia, were provided feedings supplemented with Lactobacillus acidophilus and Bifidobacterium infantis until discharge. Compared with historical controls, the incidence of NEC dropped from 6.6% to 3%. Since then, a large number of systematic reviews and randomized controlled studies have been completed to examine the impact of probiotics in neonates.
There are three possibilities regarding the future use of probiotics. Small clinical trials are currently being conducted, and there are believers and nonbelievers about potential benefit of these bacteria as a nutritional supplement. In one possibility, parents would be asked to make a choice, and the infants would be treated if the families agreed. In another possibility, probiotics would begin to be prepared with strict guidelines as a drug and be universally adopted as the standard of care. In the third, the products would still be prepared under strict oversight, and infants at high risk of conditions such as NEC or LOS would be treated. In this third possibility, infants in specific gestational age or birth weight ranges or those with high-risk conditions that are likely to benefit would continue to be identified and treated.
The outcomes of infants treated with probiotics may be reported with clinical end points such as all-cause mortality, chronic lung disease, NEC, LOS, retinopathy of prematurity, time to reach full feeds, and length of hospital stay. There may be some difficulty in separating these conditions, because infants with NEC may need respiratory support for longer periods and may be labeled as having chronic lung disease; may need central lines for parenteral nutrition, and consequently, may develop LOS; may need respiratory support with oxygen therapy that may increase the risk of retinopathy of prematurity; and with the higher severity of multisystem illness, may need a longer length of hospital stay and have a higher risk of mortality.
There is a need to evaluate composite outcomes such as all-cause mortality even in infants who develop NEC, because they are at risk of sepsis owing to the need for vascular catheters and also because of gastrointestinal injury and altered gut anatomy in the postoperative period. Many infants with secondary bacterial sepsis who remain culture-negative may be differentially labeled at various centers, and hence, this subgroup needs to be identified and evaluated. Table 18.3 shows a summary of the impact of probiotics in various clinical conditions.
| Authors | Design | Outcomes | Studies, No. | Patients, No. | Outcome (Range) | Other Conclusions |
|---|---|---|---|---|---|---|
| Deshmukh and Patole | Systematic review of non-RCTs; routine probiotic supplementation (RPS) | NEC ≥stage II, LOS, all-cause mortality, and feeding intolerance | 30 | 77,018 | Less NEC (30 studies, n = 77,018; OR, 0.60; 95% CI, 0.50–0.73); less LOS (21 studies, n = 65,858; OR, 0.85; 95% CI, 0.74–0.97); less all-cause mortality (27 studies, n = 70,977; OR, 0.77; 95% CI, 0.68–0.88). In ELBW infants, RPS reduced NEC (4.5% versus 7.9%), but not LOS and mortality. Multistrain RPS was more effective than single-strain. One study reported nonfatal probiotic sepsis in three infants. | Moderate- to low-quality evidence indicating that RPS was associated with significantly reduced NEC ≥stage II, LOS, and all-cause mortality in neonates <37 weeks of gestation and NEC ≥stage II in ELBW neonates. |
| Chi et al. | Network meta-analysis | NEC, mortality | 45 | 12,320 | Bifidobacterium plus prebiotic had the highest probability of decreasing the mortality (surface under the cumulative ranking curve, 83.94%), and Lactobacillus plus prebiotic had the highest probability of having the lowest rate of NEC (surface under the cumulative ranking curve, 95.62%). | |
| Bifidobacterium plus Lactobacillus | NEC 0.47 (0.27–0.79); mortality 0.56 (0.34–0.84) | |||||
| Lactobacillus plus prebiotic | NEC 0.06 (0.01–0.41) | |||||
| Morgan et al. | Network meta-analysis of RCTs | NEC, mortality | 63 | 15,712 | ||
| 1 or more Lactobacillus spp. and 1 or more Bifidobacterium spp. | Combination of ≥1 Lactobacillus spp. and ≥1 Bifidobacterium spp. showed moderate- to high-quality evidence of reduced all-cause mortality (OR, 0.56; 95% CI, 0.39–0.80). Bifidobacterium animalis subsp. lactis , Lactobacillus reuteri , or Lactobacillus rhamnosus reduced severe NEC (OR 0.35 [95% CI, 0.20–0.59]; OR 0.31 [95% CI, 0.13–0.74]; OR, 0.55 [95% CI, 0.34–0.91]; and OR, 0.44 [95% CI, 0.21–0.90], respectively). | Moderate to high evidence for the superiority of combinations of 1 or more Lactobacillus spp. and 1 or more Bifidobacterium spp. versus single- and other multiple-strain probiotic treatments. The combinations of Bacillus spp. and Enterococcus spp. and 1 or more Bifidobacterium spp. and Streptococcus salivarius subsp. thermophilus might produce the largest reduction in the occurrence of NEC. | ||||
| Balasubramanian et al. | Systematic review of RCTs | Mortality, NEC, LOS | 9 | 1514 | Reduced risk of NEC ≥stage II (RR, 0.36; 95% CI 0.2–0.66), LOS in 7 studies (RR, 0.56; 95% CI, 0.45–0.71), and mortality in 8 RCTs (RR, 0.62; 95% CI, 0.41–0.95) | |
| Bi et al. | Network meta-analysis | Prevention strategies | 34 | 9161 | Significant advantage of probiotic mixture and Bifidobacterium to prevent the incidence of NEC in preterm infants; a probiotic mixture showed effectiveness in reducing mortality in preterm infants. | The results showed that Bifidobacteria and a mixture of probiotics were effective; the other probiotic genera (Saccharomyces, Bacillus, Lactobacilli) failed to show an obvious effect to reduce the incidence of NEC, sepsis, and all-cause death. |
| Zhu et al. | Meta-analysis of RCT | Mortality, NEC, sepsis | 24 | 6155 | ||
| Bifidobacterium groups | NEC (RR, 0.38; 95% CI, 0.25–0.58), mortality (RR, 0.74; 95% CI, 0.60–0.92) | No significant difference in the incidence of sepsis. | ||||
| Deshpande et al. | Meta-analysis of RCTs from 10 low- and middle-income countries | Mortality, NEC, LOS | 23 | 4783 | NEC ≥ stage II (RR, 0.46; 95% CI, 0.34–0.61), LOS (RR, 0.80; 95% CI, 0.71–0.91), and all-cause mortality (RR, 0.73; 95% CI, 0.59–0.90) | |
| Dermyshi et al. | Meta-analysis of 30 RCTs and 14 observational studies | Mortality, NEC, sepsis | 44 | Mortality: RCTs, RR, 0.77 (95% CI, 0.65–0.92), observational studies, RR, 0.71 (95% CI, 0.62–0.81); NEC: RCTs, RR, 0.57 (95% CI, 0.47–0.70), observational studies, RR, 0.51 (95% CI, 0.37–0.70) | A 12% reduction in the risk of sepsis in RCTs and a 19% reduction in observational studies. | |
| Chang et al. | Fixed effects analysis | NEC, mortality | 25 | 7345 | ||
| Multiple strains | NEC: OR, 0.36 (95% CI, 0.24–0.53); mortality: OR, 0.58 (95% CI, 0.43–0.79) | |||||
| Single strains | NEC: OR, 0.6; 95% CI, 0.36–1.0 | No reduction in mortality with single strains | ||||
| Olsen et al. | Meta-analysis | NEC, mortality, sepsis | 12 | 10,800 | NEC: RR, 0.55 (95% CI, 0.39–0.78); mortality: RR, 0.72 (95% CI, 0.61–0.85) | No significant reduction in sepsis |
| Samuels et al. | Cohort study using Infloran | NEC | 1 | 5000 | Surgical NEC: RR, 0.58; 95% CI, 0.37–0.91 | |
| Singh et al. | Cohort study | NEC, mortality | 1 | 3093 | NEC: OR, 0.64 (95% CI, 0.41–0.99); mortality: OR, 0.41 (95% CI, 0.26–0.63) |
In Table 18.3, we show a summary of the studies by Deshmukh and Patole, Chi et al., Morgan et al., Balasubramanian et al., Bi et al., Zhu et al., Deshpande et al., Dermyshi et al., Chang et al., and Olsen et al. A large implementation cohort study in Germany used Infloran, a probiotic preparation of L. acidophilus and Bifidobacterium bifidum , and included more than 5000 infants. Another cohort study of 3093 infants <29 weeks’ gestation in Canada showed prophylactic probiotic supplementation to lower the risk of NEC (odds ratio [OR], 0.64; 95% confidence interval [CI], 0.41–0.99) and death (adjusted OR, 0.41; 95% CI, 0.26–0.63). An earlier single-center cohort study in the United States and Canada had shown these formulations to be efficacious. Other implementation cohort studies from France, Australia, and Switzerland have also reported decreased NEC after routine use of probiotics. Additionally, the pooled treatment effects of probiotics on NEC, death, and LOS in observational studies are similar to those in clinical trials. These findings support the external validity of the pooled estimates of probiotic treatment effects from randomized trials and increase confidence in the findings from meta-analyses of randomized trials.
Data from the studies by Sharif et al., Liu et al., Jiao et al., Hagen et al., and Lau et al. are summarized in Table 18.4. The table also shows the findings from the Probiotics in Preterm Infants (PiPS) trial, which did not find a difference in the risk of NEC between the probiotic and the placebo group.
| Authors | Design | Outcomes | Studies, No. | Patients, No. | Outcome (Range) | Other Conclusions |
|---|---|---|---|---|---|---|
| Sharif et al. | Meta-analysis | NEC, mortality, late onset infection | 56 | 10,812 | Total: NEC RR, 0.54; 95% CI, 0.45–0.65 (54 trials; 10,604 infants; I ² = 17%) Trials with low risk of bias: NEC RR, 0.70; 95% CI, 0.55–0.89 (16 trials, 4597 infants; I ² = 25%) Reduction in mortality (RR, 0.76; 95% CI, 0.65–0.89 (51 trials; 10,170 infants; I ² = 0%) and late-onset infection (RR, 0.89; 95% CI, 0.82–0.97 (47 trials, 9762 infants; I ² = 19%) |
Probiotics may have little or no effect on severe neurodevelopmental impairment |
| Liu et al. | Meta-analysis | NEC, mortality, sepsis | 23 | 4686 | NEC RR, 0.34; 95% CI, 0.25–0.46 Mortality RR, 0.48; 95% CI, 0.36–0.64 |
No significant difference in the incidence of sepsis |
| Jiao et al. | Meta-analysis | NEC | 16 | 4686 | ||
| Mixture of Bifidobacterium and Lactobacillus | NEC RR, 0.34; 95% CI, 0.25–0.46 | Single strain Lactobacillus or single strain Bifidobacterium did not show reduction in NEC | ||||
| Hagen et al. | Meta-analysis | NEC | 9 | Some benefit in infants <34 weeks’ GA with RR of 0.43 (95% CI, 0.21–0.87; P = .019) but not in neonates <28 weeks’ GA | ||
| Bifidobacterium lactis | NEC RR, 0.11; 95% CI, 0.03–0.47 | |||||
| Lau et al. | Meta-analysis | NEC, mortality, sepsis | 20 | 5982 | NEC RR, 0.509; 95% CI 0.385–0.672 Mortality RR, 0.731; 95% CI, 0.577–0.926 Sepsis RR, 0.919; 95% CI 0.823–1.027 |
|
| Probiotics in Preterm Infants (PiPS) trial | RCT | NEC | 1315 | |||
| Bifidobacterium breve BBG-001 or placebo | No benefit in NEC, no harm | 20% of infants in the placebo group were also colonized with the probiotic organism by 2 weeks of age and 49% by 36 weeks postmenstrual age, suggesting notable cross-contamination |
Most trials of probiotic supplementation have enrolled very low birth weight (VLBW) infants, but ELBW infants are underrepresented in many studies. A large German cohort study demonstrated beneficial effects of probiotics in ELBW infants. However, the subgroup analyses of the ProPrems trial did not find any significant differences in effects of probiotics on NEC between ELBW and other premature infants. The use of probiotics in more mature populations to prevent NEC may substantially increase the number needed to treat (NNT) to prevent NEC, because the baseline incidence would be lower in this population.
The 2020 Cochrane Database of Systematic Reviews evaluated 56 trials with 10,812 infants. Most trials were small (median sample size, 149), and there were concerns about the possibility of bias in about half of the trials. Trials varied by the formulation of the probiotics; most preparations contained Bifidobacteria , Lactobacilli , Saccharomyces species (spp.), and Streptococcus spp. alone or in combinations. Meta-analysis showed that probiotics may reduce the risk of NEC: relative risk [RR], 0.54; 95% CI, 0.45–0.65 (54 trials; 10,604 infants; I ² = 17%); risk difference [RD], −0.03; 95% CI, −0.04 to −0.02; NNT for an additional beneficial outcome (NNTB), 33; 95% CI, 25–50. Evidence was assessed as low certainty because of the limitations in trials design and the presence of funnel plot asymmetry consistent with publication bias. Sensitivity meta-analysis of trials at low risk of bias showed a reduced risk of NEC: RR, 0.70; 95% CI, 0.55–0.89 (16 trials, 4597 infants; I ² = 25%); RD, −0.02; 95% CI; −0.03 to −0.01; NNTB, 50; 95% CI, 33–100. Meta-analyses showed that probiotics probably reduce mortality (RR, 0.76; 95% CI, 0.65–0.89 [51 trials, 10,170 infants; I ² = 0%]; RD, −0.02; 95% CI, −0.02 to −0.01; NNTB, 50; 95% CI, 50–100), and late-onset invasive infection (RR, 0.89; 95% CI, 0.82–0.97; [47 trials, 9762 infants; I ² = 19%]; RD, −0.02; 95% CI, −0.03 to −0.01; NNTB, 50; 95% CI 33–100). Sensitivity meta-analyses of 16 trials (4597 infants) at low risk of bias did not show an effect on mortality or infection. Meta-analysis showed that probiotics may have little or no effect on severe neurodevelopmental impairment (RR, 1.03; 95% CI, 0.84–1.26 (five trials, 1518 infants; I ² = 0%). The certainty of this evidence is low because of design limitations.
Rao et al. examined pooled results from 37 RCTs (N = 9416) of probiotics versus placebo/no probiotics using a fixed effects model. In meta-analysis, probiotics decreased the risk of LOS.
| Authors | Design | Outcomes | Studies, No. | Patients, No. | Outcome (Range) | Other Conclusions |
|---|---|---|---|---|---|---|
| Rao et al. | Meta-analysis with fixed effects model | Late-onset sepsis | 37 | 9416 | RR, 0.86 (95% CI, 0.78–0.94) | |
| Qamer et al. | Systematic review | Cow's milk protein allergy | 10 | 845 | Probiotics expedited the acquisition of tolerance to cow's milk protein at the end of 3 years compared with placebo (RR, 1.47; 95% CI, 1.17–1.84) | Not associated with earlier resolution of hematochezia; no adverse events reported |
| Ong et al. | Systematic review | Infantile colic—minutes of crying | 6 | 1886 | ||
| Lactobacillus reuteri | Reduction of 44.3 minutes in daily crying with a random-effects model (95% CI, −66.6 to −21.9; I 2 = 92%), favoring probiotics | No clear evidence that probiotics are more effective than placebo at preventing infantile colic | ||||
| Sung et al. | Meta-analysis | Infantile colic—minutes of crying | 4 | 345 | ||
| L. reuteri DSM17938 | Day 21 crying reduction of 25.4 (95% CI, −47.3 to −3.5) minutes | Intervention effects were dramatic in breastfed infants (number needed to treat for day 21 success, 2.6 [95% CI, 2.0–3.6]) but were insignificant in formula-fed infants | ||||
| Harb et al. | Subgroup meta-analysis | Infantile colic—minutes of crying | 6 | Day 21: −55.8 (95% CI, −64.4 to −47.3) min/day of crying | ||
| Deshmukh et al. | Meta-analysis | Hyperbilirubinemia—duration of phototherapy | 9 | 279 | Mean difference, −11.80 (95% CI, −17.47 to −6.13) TSB reduced at 96 h: mean difference, −1.74 (95% CI, −2.92 to −0.57) TSB reduced at 7 days: mean difference, −1.71 (95% CI, −2.25 to −1.17) |
There were no probiotic-related adverse effects; limited low-quality evidence indicates that probiotic supplementation may reduce the duration of phototherapy in neonates with jaundice |
| Chen et al. | Meta-analysis of RCTs | Serum bilirubin, duration of phototherapy, need for hospitalization | 12 | 1067 | 3 days: mean difference, −18.05 (95% CI, −25.51 to −10.58) 5 days: mean difference, -23.49 (95% CI, −32.80 to −14.18) 7 days: mean difference, −33.01 (95% CI, −37.31 to −28.70) Duration of phototherapy: mean difference, −0.64 (95% CI, −0.84 to −0.44) Hospitalization: mean difference, −2.68 (95% CI, −3.18 to −2.17) |
|
| Rao et al. | Meta-analysis | Difference in microbiomes in gastroschisis patients | 2 | 24 | In one study, overall microbial communities were not significantly different between groups; in another study there were significantly more Streptcoccaceae in the fecal samples in the probiotic group and significantly more Bifidobacteriaceae in the no-probiotic group | The role of probiotics in neonates with gastrointestinal surgical conditions is still unclear and needs further study |
| Hu et al. | Meta-analysis | Candida colonization, invasive fungal sepsis | 7 | 1371 | Candida colonization: RR, 0.43 (95% CI, 0.27–0.67) Invasive fungal sepsis: RR, 0.64 (95% CI, 0.46–0.88) |
Qamer et al. performed a systematic review of efficacy and safety of probiotics in the management of cow's milk protein allergy (CMPA). Primary outcomes were resolution of hematochezia and acquisition of tolerance to CMP, and the secondary outcomes included effects on allergic symptoms, growth, gut microbiota, and adverse effects. Ten RCTs (N = 845) were analyzed, but no significant benefits were seen. However, in confirmed CMPA, limited low-quality evidence showed that probiotics expedited the acquisition of tolerance to CMP at the end of 3 years.
Colic is defined as periods of inconsolable crying, fussing, or irritability that have no apparent cause and present in otherwise healthy infants. Simonson et al. performed a systematic review and showed that oral administration of probiotics to breastfed infants with colic resulted in at least a 50% reduction in crying time compared with placebo. Ong et al., Sung et al., and Harb et al. also showed benefit.
Probiotics seem to be efficacious in reducing the severity of neonatal hyperbilirubinemia. Deshmukh et al. analyzed 9 RCTs (prophylactic: 6 trials, N = 1761; therapeutic: 3 trials, N = 279). Total serum bilirubin (TSB) was significantly reduced at 96 hours. Chen et al. examined 13 RCTs involving 1067 neonates with jaundice in a meta-analysis and also noted efficacy.
In other gastrointestinal surgical conditions, probiotics may not be so effective. Rao et al. examined two RCTs; the first was conducted in 24 neonates with gastroschisis, the second in 8 with various surgical conditions. Based on these data, the role of probiotics in neonates with gastrointestinal surgical conditions is still unclear and needs further study.
Hu et al. examined 7 trials involving 1371 preterm neonates. Meta-analysis (fixed-effects model) showed that probiotic supplementation was associated with a lower risk of Candida colonization and invasive fungal sepsis. However, after excluding one study with a high baseline incidence of fungal sepsis, the effect of probiotics on invasive fungal sepsis became statistically insignificant. When using a random-effects model, the effect of probiotics remained favorable for Candida colonization but not for fungal sepsis.
The decision to start using probiotics in a NICU is a complex one ( Table 18.6 ). The proportion of infants receiving their mother's own or a banked human milk is important, and therefore, promotion of human milk feeding should be the major focus of efforts to decrease NEC. Additionally, human milk contains oligosaccharides that can promote the growth of probiotic bacteria such as B. infantis. Prebiotics can be useful in some instances, but further research is needed to determine the efficacy of prebiotics compared with live bacteria. Some randomized trials have combined the use of prebiotics with probiotics, but this strategy might still not adequately compensate for all the beneficial components of breast milk that may protect against NEC, including lowering gastric pH, enhancing intestinal motility, and decreasing epithelial permeability. ,
| Support Starting Routine Probiotic Supplementation | Do Not Support Starting Routine Probiotic Supplementation |
|---|---|
| Preclinical and human data support biologic plausibility | No regulator-approved drug formulation (in US or UK) |
| Numerous RCTs enrolling >10,000 infants show consistent benefit (low heterogeneity) in decreasing the risk of NEC | Concerns regarding product quality and contamination |
| Large magnitude of effect on NEC in meta-analysis (decreases RR by approximately one-half); lower risk of late-onset sepsis and all-cause mortality | Well-conducted, multicenter trial (PiPS) showed no benefit on NEC (of note, relatively high rate of cross-colonization with probiotic strain in control arm) |
| Multiple implementation cohort studies support effectiveness of probiotic supplementation in routine practice | Uncertainty regarding optimal product/strain, including dose and duration of supplementation |
| Meta-analysis for subgroup of infants with birth weight <1000 g infants show no increased risks of sepsis | Limited long-term follow-up data (Two studies showed no evidence of harm; one showed a lower risk of deafness) |
| Low relative cost of supplementation | High NNT for centers with low NEC incidence |
| NEC remains a major cause of death in preterm infants. | Other opportunities (such as increasing human milk feeding) to decrease the risk of NEC |
At each center, the baseline incidence of NEC is an important consideration for making decisions about the routine use of probiotics. This incidence will provide an idea about the estimated NNT to prevent one case of NEC. The center will also need to consider the case-fatality and morbidity rates. As the baseline risks decrease, the NNT to prevent one case of NEC increases ( Table 18.7 ). This table is based on the incidence of NEC reported in the literature and estimates of treatment effect on NEC from Sawh et al.
| Baseline NEC Incidence, % | Absolute Risk Reduction, % | NNT (95% CI) |
|---|---|---|
| 1.0 | 0.5 | 213 (172–294) |
| 2.0 | 0.9 | 106 (86–147) |
| 3.0 | 1.4 | 71 (57–98) |
| 4.0 | 1.9 | 53 (43–74) |
| 5.0 | 2.4 | 43 (34–59) |
| 7.5 | 3.5 | 28 (23–39) |
| 10.0 | 4.7 | 21 (17–29) |
| 12.5 | 5.9 | 17 (14–24) |
| 15.0 | 7.1 | 14 (11–20) |
| 20.0 | 9.4 | 11 (9–15) |
There are also several practical issues to consider. A team-based approach is important, including nursing leadership, pharmacy, infectious disease, and microbiology. Each stream of experts contributes to the program with expertise and infrastructure. Some authors have suggested that local evaluation of bacterial species of probiotics is an important quality-control measure, although such an approach for single-dose preparations may not always be feasible. The rationale for and approach to implementation should be documented.
Most large trials have used 10 8 to 10 9 probiotic bacteria per dose because stool bacterial counts seem to plateau beyond these counts. Further work is needed to optimize these doses because the numbers of bacteria in stool may be more an indicator of transit than of ecological establishment. Existing studies have focused either on the prevention or on the correction of already established dysbiosis with Enterobacteriaceae. The time to initiate administration of probiotics is harder to decide until further data are available; determining the time to stop supplementation may be simpler when the risk of maturity-related complications related to dysbiosis, such as NEC, becomes lower.
Vaginally delivered infants become colonized with microorganisms such as Enterobacteriaceae , Bacteroides, and Parabacteroides in the mother's vaginal tract, whereas those delivered by cesarean section become colonized with organisms such as Staphylococci and Streptococci from maternal skin and the oral cavity. However, exclusive breastfeeding in the first week can quickly introduce high levels of Bifidobacteria and Lactobacillus. This pattern may not always remain intact in premature infants, who are more frequently delivered by cesarean section and get colonized with skin-related organisms.
Social structure and family interactions also play a role in the early-life microbiome. Breastfeeding may link the microbiome between mothers and infants, including transmission of probiotic-like organisms such as Lactobacilli and Bifidobacteria , and may protect against many infectious diseases and at least early onset of atopy. Family contacts can also increase the risk for acquisition of bacteria such as methicillin-resistant Staphylococcus aureus. There may be differences in the oral microbiota among infants for whom the parents did versus did not use pacifiers. In rural settings, microbiome sharing may extend to livestock, household surfaces, and household members.
Toll-like receptor (TLR) 4 is a membrane-spanning protein that binds lipopolysaccharide and activates immune responses. Low-level TLR4 stimulation may promote immune homeostasis and gut maturation in utero , but high-level stimulation with dysbiosis may trigger inflammation and NEC. Neonatal enterocytes and leukocytes express higher levels of TLR4, MyD88, and NFκB than in adults. Probiotic-conditioned media from B. infantis (ATCC 15697) and L. acidophilus (ATCC 53103) suppress inflammatory responses in tissue explants and rodent models. Lactobacillus reuteri (DSM 17938 and ATCC PTA 4659) showed similar results. In porcine peripheral blood monocytes, L. acidophilus suppressed lipopolysaccharide-induced inflammatory responses. Lactobacilli and Propiniobacteria produce a surface-layer protein B (SlpB) that inhibits cytokine expression.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here