Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pleurisy is the inflammation of the pleura; it may be accompanied by an effusion. The most common cause of pleural effusion in children is bacterial pneumonia (see Chapter 428 ); heart failure (see Chapter 469 ), rheumatologic causes, and metastatic intrathoracic malignancy are also common causes. A variety of other diseases account for the remaining cases, including tuberculosis (see Chapter 242 ), lupus erythematosus (see Chapter 183 ), aspiration pneumonitis (see Chapter 425 ), uremia, pancreatitis, subdiaphragmatic abscess, and rheumatoid arthritis.
Inflammatory processes in the pleura are usually divided into 3 types: dry pleurisy, serofibrinous or serosanguineous, and purulent pleurisy or empyema.
Dry pleurisy, formerly called plastic pleurisy, may be associated with acute bacterial or viral pulmonary infections or may develop during the course of an acute upper respiratory tract illness. The condition is also associated with tuberculosis and autoimmune diseases such as systemic lupus erythematosus.
The process is usually limited to the visceral pleura, with small amounts of yellow serous fluid and adhesions between the pleural surfaces. In tuberculosis, pleurisy can be caused by a severe delayed-type hypersensitivity reaction to Mycobacterium tuberculosis ; the adhesions develop rapidly, and the pleura are often thickened. Occasionally, fibrin deposition and adhesions are severe enough to produce a fibrothorax that markedly inhibits the excursions of the lung.
The primary disease often overshadows signs and symptoms of pleurisy. Pain, the principal symptom, is exaggerated by deep breathing, coughing, and straining. Occasionally, pleural pain is described as a dull ache, which is less likely to vary with breathing. The pain is often localized over the chest wall and is referred to the shoulder or the back. Pain with breathing is responsible for grunting and guarding of respirations, and the child often lies on the affected side in an attempt to decrease respiratory excursions. Early in the illness, a leathery, rough, inspiratory and expiratory friction rub may be audible, but it usually disappears rapidly. If the layer of exudate is thick, increased dullness to percussion and decreased breath sounds may be heard. Pleurisy may be asymptomatic. Chronic pleurisy is occasionally encountered with conditions such as atelectasis, pulmonary abscess, connective tissue diseases, and tuberculosis.
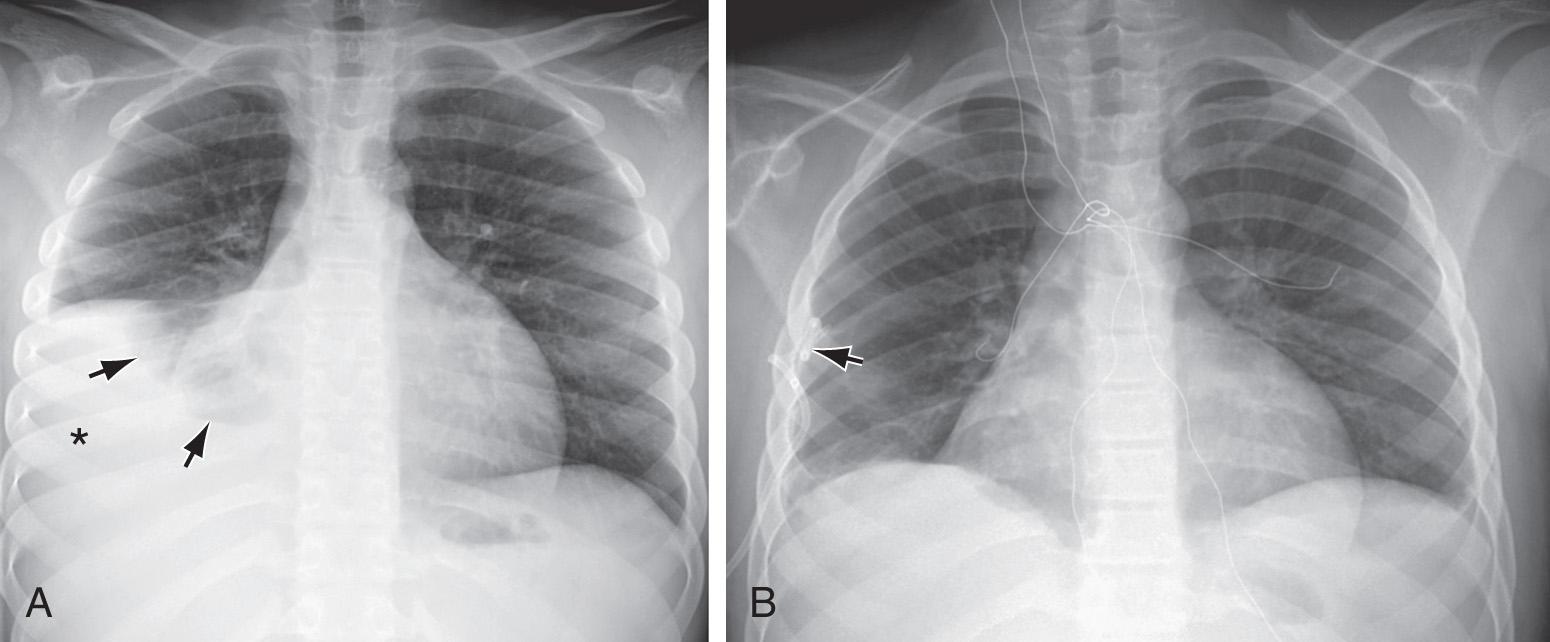
Dry pleurisy may be detected on radiographs as a diffuse haziness at the pleural surface or a dense, sharply demarcated shadow ( Figs. 429.1 and 429.2 ). The latter finding may be indistinguishable from small amounts of pleural exudate. Chest radiographic findings may be normal, but ultrasonography or CT findings will be positive.
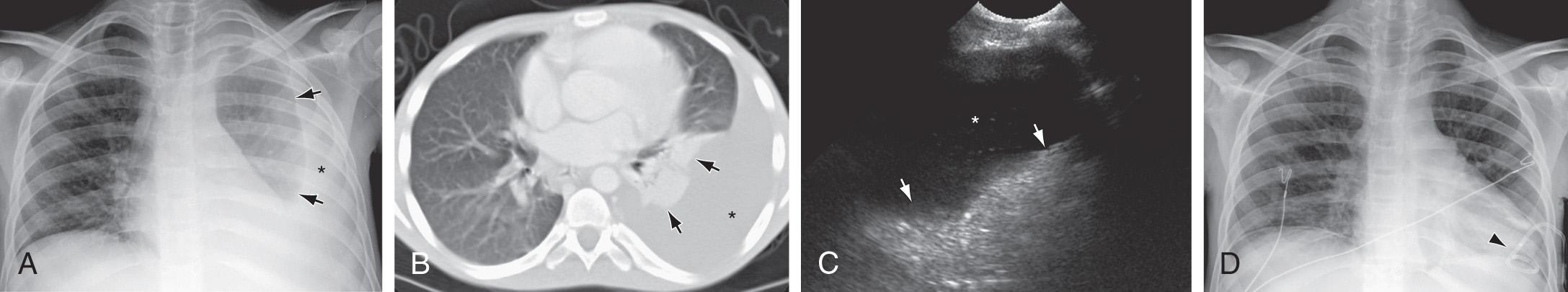
Pleurisy must be distinguished from other diseases, such as epidemic pleurodynia, trauma to the rib cage (rib fracture), lesions of the dorsal root ganglia, tumors of the spinal cord, herpes zoster, gallbladder disease, and trichinosis. Even if evidence of pleural fluid is not found on physical or radiographic examination, a CT- or ultrasound-guided pleural tap in suspected cases often results in the recovery of a small amount of exudate, which when cultured may reveal the underlying bacterial cause in patients with an acute pneumonia. Patients with pleurisy and pneumonia should always be screened for tuberculosis.
Therapy should be aimed at the underlying disease. When pneumonia is present, neither immobilization of the chest with adhesive plaster nor therapy with drugs capable of suppressing the cough reflex is indicated. If pneumonia is not present or is under good therapeutic control, strapping of the chest to restrict expansion may afford relief from pain. Analgesia with nonsteroidal antiinflammatory agents may be helpful.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here