Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A plain abdominal radiograph must be read with a complete knowledge of the clinical situation. The patient's history and results of the physical examination and laboratory studies are always important to evaluate an acute abdomen, which may be caused by various different diseases. Obtaining plain films with the patient supine and erect and that include the diaphragm is the classic approach. Because chest abnormalities may produce an acute abdomen, a chest posteroanterior radiograph is sometimes ordered.
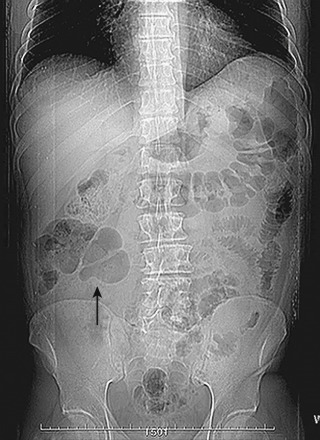
The standard abdominal radiograph is a supine projection: x-rays are passed from front to back (anteroposterior projection) in a patient lying on his or her back ( Figure 1-1 ). In some circumstances, an abdominal radiograph taken with the patient erect is requested; its advantage over a supine film is the visualization of air/fluid levels. A decubitus film (with the patient lying on his or her side) is also of use in certain situations, especially to visualize fluid levels in the large bowel.

It is important, as with any imaging technique, that the technical details of an abdominal radiograph are assessed. The date the film was taken and the name, age, and sex of the patient are all worth noting. This ensures you are reviewing the correct film with the correct clinical information, and it also may aid your interpretation. Unless the order is specifically labeled, the film is taken with the patient supine. The best way to appreciate normality is to look at as many films as possible, with an awareness of anatomy in mind. Although an abdominal radiograph is a plain radiograph, it has a radiation dose equivalent to 50 posteroanterior chest radiographs or 6 months of standard background radiation.
Many techniques may be used to acquire images of the abdomen, including ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI), but the plain abdominal radiograph is the technique that is most readily available in the emergency situation when a patient presents with acute abdominal pain.
Radiographs should never be requested without due consideration. They expend resources and expose the patient to ionizing radiation. They are an adjunct to a careful history and thorough physical examination.
The abdominal radiograph has the advantage of low cost. It is easy to perform and can be done on uncooperative patients, and, if correctly carried out and carefully interpreted, it can still be used with a dual purpose. It can be used to evaluate catheter placement; identify ingested, inhaled, or introduced foreign bodies or free air in patients with a gastrointestinal perforation (conditions for which the examination is often diagnostic); or assess a condition of intestinal occlusion or an abdomen in the postoperative phase. It also can be of use in documenting the intestinal morphodynamics, the findings of which at the direct examination of the abdomen depend on both the cause of the acute pathologic process and the time when the examination is performed with respect to the onset of the insult. In addition, plain abdominal radiographs are an accessible, relatively inexpensive, convenient, and accurate method of detecting retained surgical needles. They can be used effectively to locate needles over 10 mm in length retained in the abdomen, with a sensitivity of 92% in this size range. In this scenario, plain abdominal radiographs should continue to be used after incorrect needle counts. It is also recommended that the requesting physician provide the radiologist the size of the lost needle. However, for missing needles of 10 mm or less in length, the utility of plain abdominal radiographs is more debatable.
Conversely, criticisms of requests for abdominal films often quote a low number of cases in which the diagnosis or management was changed by the radiographic findings. The diagnostic value is questionable, and very often there is no clear indication. In the majority of cases, the results are negative or nonspecific. In fact, as reported in a recent article by Kellow and colleagues, the results of abdominal radiography are neither sensitive nor specific. Flak and Rowley suggested that there are only two clinical entities in which sensitivity of abdominal radiography approaches 100%: free intraperitoneal air and, to a lesser extent, bowel obstruction. For the latter indication, a prospective trial conducted by Frager and associates determined that clinical and radiographic evaluation was never precise enough to provide the exact location or cause of small bowel obstruction. Furthermore, Taourel and coworkers demonstrated that not only is CT valuable in making a more accurate diagnosis but also that clinical treatment was correctly modified in 21% of patients because of the additional information provided by using CT. Therefore, abdominal radiography appears of limited value in the initial diagnosis of obstruction. For the indication of free air, the diagnosis is better made by evaluation of a chest radiograph obtained with the patient erect. In addition, only a few physicians are aware of the relatively high radiation dose of an abdominal film, which is equal to 50 chest radiographs.
In the 1950s, gastrointestinal radiology consisted of plain abdominal films and single-contrast barium studies to assess gastrointestinal diseases. Today, the plain radiograph still may be the first step to evaluate acute abdominal diseases. However, with the advent of CT and ultrasonography, the importance of the plain abdominal film is decreasing. In past years, plain radiography was also used to help diagnose abdominal pathologic processes such as stones in the kidney, gallbladder, or bladder. Plain radiography is now limited to emergency radiology in the acute abdomen. However, despite the undoubted advantages of the speed of examination, the multiplanar capabilities, and the objectivity of interpretation, CT subjects the patient to a higher dose of ionizing radiation. The role of plain radiography of the abdomen in the diagnosis of acute abdomen needs to be reconsidered. According to some authors, plain radiography should be performed only in patients for whom there are known advantages, such as in the case of suspected gastrointestinal perforation, intestinal occlusion, ingestion of or the search for foreign bodies, and assessment of the postoperative abdomen ; in these cases, it is still the examination of choice, and only if it does not prove diagnostic should a CT examination be recommended. In addition to these situations, however, there is another indication: the ability of plain radiography to assess the evolution of intestinal morphodynamism, that is, the variations in the motility, shape, and position of the small bowel in acute pathologic conditions. Even though in the first instance assessing the cause or the precise site of the obstruction is advisable, differentiating at least a mechanical ileus from a paralytic ileus, and above all having an understanding of the seriousness and the extension of the cause and the time elapsed since its onset can prove clinically more useful. Few comparisons of plain abdominal radiographs and CT scans exist in the literature. Siewert and associates reported on 91 admitted patients with acute abdominal pain who eventually received CT because of continuing symptoms or failure to respond to therapy. In this series, treatment was changed after CT in 25 patients (27%), but the authors did not state the relative contribution of the plain abdominal radiographs to the pre-CT diagnosis. In particular, the percentage of patients who had abnormal plain abdominal radiographs was not given. A retrospective review of 23 patients with proved mesenteric infarction compared plain abdominal radiographs with CTs and showed that 6 patients (26%) had abnormal plain abdominal radiographs only, 8 patients (35%) had abnormal CTs only, and in only 1 patient (4%) were both tests abnormal. Both studies were normal or nonspecific in 8 patients (35%). That 26% of patients had signs of an acute abdominal syndrome shown only on plain abdominal radiographs and not on CT is in sharp contradiction to our findings, in which the plain abdominal radiographs provided minimal additional information in 2 of 74 patients (3%) and at the cost of 33 (57%) potentially misleading false-negative results. There are several possible explanations. Mesenteric infarction may represent one of a series of specific syndromes that have either relatively low CT sensitivity, high plain abdominal radiograph sensitivity, or both. In the review just cited, no patients were diagnosed on plain abdominal radiographs, CT, or clinical course with this syndrome. Other possibilities include individual or institutional variations in radiologic interpretations or improvement in the interpretation of CTs for this and other syndromes over the past decade. The increased imaging capabilities of this newer technology would most likely make the test characteristics of the newer CT scanners even more favorable. Despite these limitations, for emergency department patients with acute abdominal, flank, or back pain, in whom a CT is likely to be obtained, a preliminary plain abdominal radiograph adds almost no additional information and is potentially misleading. Given the utilization of resources required for plain abdominal radiographs as well as the time delay to obtain them, some authors believe that patients in whom the clinical suspicion of significant intra-abdominal pathology is high should go directly to CT.
As with any plain radiograph, only five main densities may be distinguished, four of which are natural: black for gas, white for calcified structures, gray representing a host of soft tissue, and a slightly darker gray for fat (because it absorbs slightly fewer x-rays). Metallic objects are seen as an intense bright white. The clarity of outlines of structures depends, therefore, on the differences among these densities. On the chest radiograph, this is easily shown by the contrast between lung and ribs as black air against the white calcium-containing bones. These differences are much less apparent on the abdominal radiograph because most structures are of similar density, mainly soft tissue. A systematic approach to plain abdominal radiographs will help avoid errors in interpretation. Interpretation of the abdominal radiograph depends on the assessment of the bowel gas pattern, solid organ outlines, a search for abnormal calcification, and a review of the skeleton. A search should be made for extraluminal gas. A bowel gas pattern distinguishing the colon from the small bowel may be difficult. The presence of solid feces and the distribution, caliber, and mucosal pattern of the bowel help in deciding whether a particular loop of bowel is stomach, small intestine, or colon. The presence of solid feces indicates the large bowel, which also may be recognized by the incomplete haustral band crossing the colonic gas shadow. Haustra are usually present in the ascending and transverse colon but may be absent from the splenic flexure and descending colon. The valvulae conniventes of the small bowel are closer together and cross the width of the bowel. The distal ileum when dilated can appear smooth, which makes differentiation more difficult. The small bowel when obstructed is generally centrally positioned with numerous loops of tighter curvature than the large bowel. Maximal small bowel caliber is 3.5 cm in the jejunum and 2.5 cm in the ileum. Maximal caliber of the transverse colon on plain films is taken to be 5.5 cm in diameter, and the maximal cecal diameter is 9 cm. Solid organs, the liver edge, renal outlines, and the splenic tip may all be demonstrated.
One should begin by looking at the amount and distribution of gas in the bowels (intraluminal gas). There is considerable normal variation in the distribution of bowel gas ( Figure 1-2 ). On the abdominal radiograph taken with the patient erect, the gastric gas bubble in the left upper quadrant of the film is a normal finding. Gas is also normally seen within the large bowel, most notably the transverse colon and rectum. Small and large bowel also can be distinguished, most easily when dilated, by their different mucosal markings. Small bowel has valvulae conniventes that traverse the full width of the bowel; large bowel has haustra that cross only part of the bowel wall. These features are important in the next part of this series, which considers abnormal intraluminal gas. Occasionally, fluid levels in the small bowel are a normal finding. Fecal matter in the bowel gives a “mottled” appearance. This is seen as a mixture of gray densities representing a gas/liquid/solid mixture.
Gas outside the bowel lumen is invariably abnormal ( Figure 1-3 ). The largest volume of gas one might see is likely to be under the right diaphragm; this occurs after a viscus has been perforated. This gas within the peritoneal cavity is termed pneumoperitoneum. Gas in the right upper quadrant within the biliary tree is a “normal” finding after sphincterotomy or biliary surgery, but it can indicate the presence of a fistula between the biliary tree and the gut. One must beware of gas in the portal vein, because this can look very similar to biliary air. Gas in the portal vein is always pathologic and frequently fatal. It occurs in ischemic states, such as toxic megacolon, and it may be accompanied by gas within the bowel wall (intramural gas) ( Box 1-1 ).

Under the diaphragm
In the biliary system
Within the bowel wall
Calcium is visible in a variety of structures, both normal and abnormal, and becomes more common with advancing age. Calcification should be identified and anatomically located. In some locations (e.g., vascular calcification), it is common and benign. Vascular calcification may be seen within the aorta, in the splenic artery in the left upper quadrant, or in the pelvis. Abdominal aortic aneurysms are usually below the second lumbar vertebra. Calcification can make them obvious and can give a rough indication of the internal diameter. Abdominal ultrasonography is required for accurate assessment and to determine the need for surgery or follow-up. Uterine fibroids can become calcified.
Calcified renal tract stones should be looked for around the renal outlines and down the line of the ureters. More rarely, calcified gallstones are seen in the right upper quadrant or a calcified (porcelain) gallbladder is present. The pancreas lies at the level of the T9 to T12 vertebrae. Calcification occurs in chronic pancreatitis and may show the whole outline of the gland.
In the pelvic region, bladder calculi may occasionally be seen. Bladder stones are usually quite large and often multiple. Calcification of a bladder tumor also may occur. Schistosomiasis may produce calcification of the bladder wall.
Other causes of pelvic calcification include phleboliths, calcified fibroids, and, rarely, calcification in ovarian dermoids, which may also contain teeth and hair.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here