Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
One of the most characteristic features of human embryonic development is the intimate relationship between the embryo and the mother. The fertilized egg brings little with it except genetic material. To survive and grow during intrauterine life, the embryo must maintain an essentially parasitic relationship with the body of the mother for acquiring oxygen and nutrients and eliminating wastes. It must also avoid rejection as a foreign body by the immune system of its maternal host. These exacting requirements are met by the placenta and extraembryonic membranes that surround the embryo and serve as the interface between the embryo and the mother.
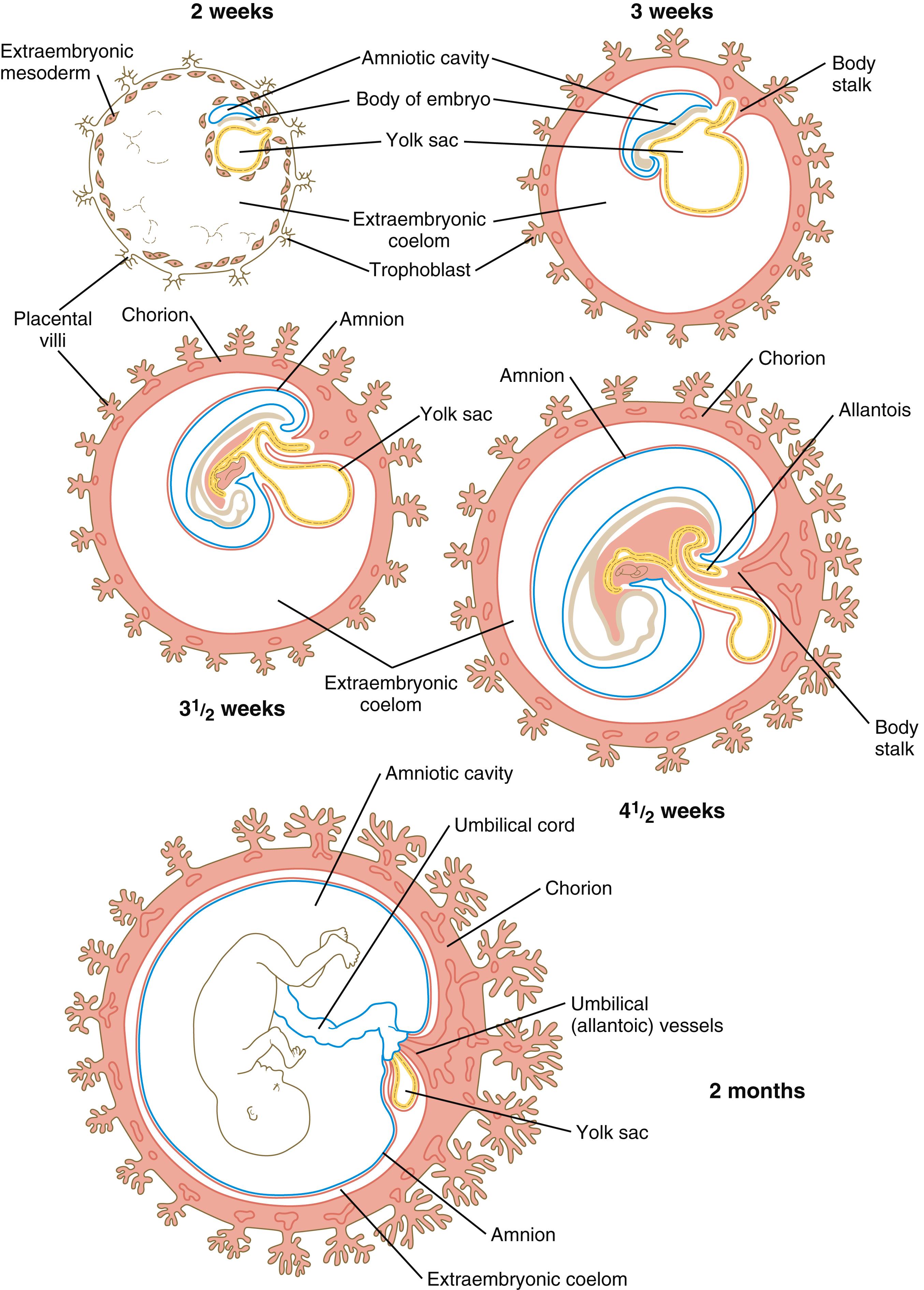
The tissues that compose the fetal–maternal interface ( placenta and chorion ) are derivatives of the trophoblast , which separates from the inner cell mass and surrounds the cellular precursors of the embryo proper even while the cleaving zygote travels down the uterine tube on its way to implanting into the uterine wall (see Figure 4.20 ). Other extraembryonic tissues are derived from the inner cell mass. These include the following: the amnion (an ectodermal derivative), which forms a protective fluid-filled capsule around the embryo; the yolk sac (an endodermal derivative), which in mammalian embryos no longer serves a primary nutritive function; the allantois (an endodermal derivative), which is associated with the removal of embryonic wastes; and much of the extraembryonic mesoderm , which forms the bulk of the umbilical cord, the connective tissue backing of the extraembryonic membranes, and the blood vessels that supply them.
The origin of the amniotic cavity within the ectoderm of the inner cell mass in the implanting embryo is described in Chapter 5 (see Chapter 4, Chapter 5 ). While the early embryo undergoes cephalocaudal and lateral folding, the amniotic membrane surrounds the body of the embryo like a fluid-filled balloon ( Figure 7.1 ), thus allowing the embryo to be suspended in a liquid environment for the duration of pregnancy. The amniotic fluid serves as a buffer against mechanical injury to the fetus; in addition, it accommodates growth, allows normal fetal movements, and protects the fetus from adhesions.
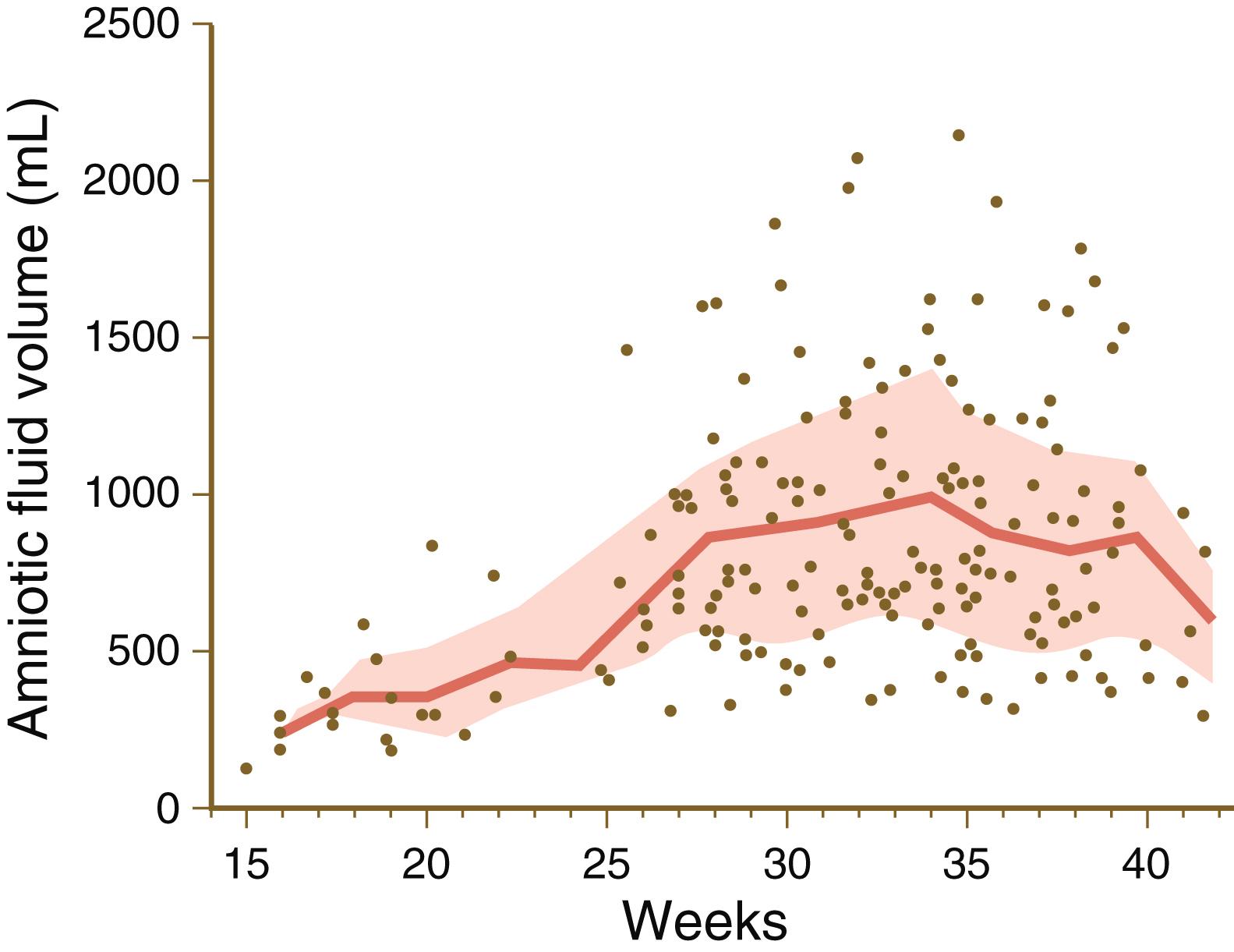
The thin transparent amniotic membrane consists of a single layer of extraembryonic ectodermal cells lined by a nonvascularized layer of extraembryonic mesoderm. A basal lamina lies between these two layers. Keeping pace with fetal growth, the amniotic cavity steadily expands until its fluid content reaches a maximum of nearly 1 L by weeks 33 to 34 of pregnancy ( Figure 7.2 ).
In many respects, amniotic fluid can be viewed as a dilute transudate of maternal plasma, but the origins and exchange dynamics of amniotic fluid are complex and not completely understood. There are two phases in amniotic fluid production. The first phase encompasses the first 20 weeks of pregnancy, during which the composition of amniotic fluid is quite similar to that of fetal fluids. During this period, the fetal skin is unkeratinized, and there is evidence that fluid and electrolytes are able to diffuse freely through the embryonic ectoderm of the skin. In addition, the amniotic membrane itself secretes fluid, and components of maternal serum pass through the amniotic membrane.
As pregnancy advances (especially after week 20, when the fetal epidermis begins to keratinize), changes occur in the source of amniotic fluid. During the fetal period, the major contributors to the formation of amniotic fluid are fetal urine and secretions from the lungs, with urine accounting for almost three quarters of the total volume. The near-term period is marked by high production of fetal urine—as much as 25% of total body weight (approximately 1000 mL) per day. A close balance exists between the inflow and outflow of amniotic fluid to maintain a state of equilibrium ( Figure 7.3 ). Fetal swallowing accounts for a considerable percentage of fluid removal, but the most important factor appears to be absorption by the amniotic membrane, which accounts for more than half of the amount of fluid removed and can be adjusted to compensate for excess or deficient amounts of amniotic fluid. Other sources of fluid inflow or outflow are of almost negligible amounts.
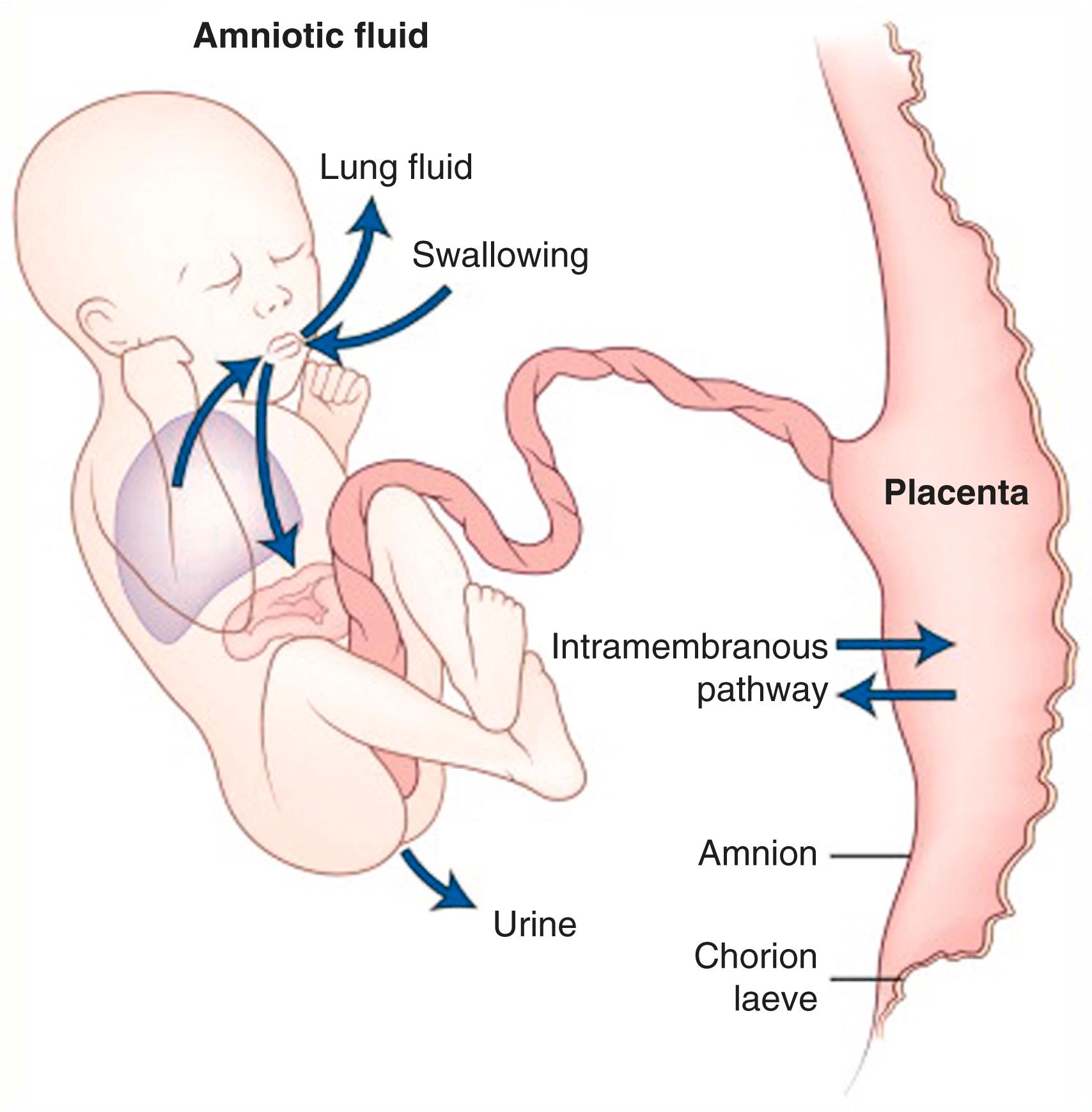
In the third trimester of pregnancy, the amniotic fluid turns over completely every 3 hours and at term, the fluid exchange rate may approach 500 mL/h. Although much of the amniotic fluid is exchanged across the amniotic membrane, fetal swallowing is an important mechanism in late pregnancy, with approximately 20 mL/h of fluid swallowed by the fetus. Swallowed amniotic fluid ultimately enters the fetal bloodstream after absorption through the gut wall. The ingested water can leave the fetal circulation through the placenta. During the fetal period, excreted urine from the fetus contributes to amniotic fluid. Clinical Correlation 7.1 discusses conditions related to the amount of amniotic fluid or substance concentrations in the fluid.
Traditionally, the amniotic membrane has been discarded along with the placenta and other extraembryonic tissues after the child has been born. In more recent years, however, important medical uses have been found for amniotic membranes. Because of the antiinflammatory and antiangiogenic properties of amnion, sheets of amnion have been used to cover a variety of wounds or burn surfaces, especially in ophthalmic surgery. The amnion, amniotic fluid, and other placental tissues have proven to be a major source of stem cells, which have the capability of differentiating into cell types from each of the three germ layers.
The yolk sac, which is lined by extraembryonic endoderm, is formed ventral to the bilayered embryo when the amnion appears dorsal to the embryonic disk (see Figure 5.2 ). In contrast to birds and reptiles, the yolk sac of mammals is small and devoid of yolk. Although vestigial in terms of its original function as a major source of nutrition, the yolk sac remains vital to the embryo because of other functions that have become associated with it. Three vital functions are (1) nutrition of the early embryo, (2) involvement in primary germ cell migration, and (3) early hematopoiesis.
When it first appears, the yolk sac is in the form of a hemisphere bounded at the equatorial region by the dorsal wall of the primitive gut (see Figure 7.1 ). As the embryo grows and undergoes lateral folding and curvature along the craniocaudal axis, the connection between the yolk sac and the forming gut becomes attenuated in the shape of a progressively narrowing stalk attached to a more spherical yolk sac proper at its distal end. In succeeding weeks, the yolk stalk becomes very long and attenuated as it is incorporated into the body of the umbilical cord. The yolk sac itself moves nearer the chorionic plate of the placenta ( Figure 7.4 ). The endoderm of the yolk sac is lined on the outside by well-vascularized extraembryonic mesoderm. The vasculature of the yolk sac is necessary for both nutrition and blood formation in the early embryo.

The human yolk sac does not actually contain yolk and for years it was considered to be unimportant in the nutrition of the embryo. More recently, however, the vasculature of the yolk sac has been shown to facilitate the histiotrophic nutrition of the embryo. Before the vasculature of the placenta becomes established, the early embryo receives its nutrition by the absorption of uterine fluids through the trophoblastic tissues. These nutrients then enter the extraembryonic coelom and are subsequently absorbed through the walls of the blood vessels lining the yolk sac. Through the vitelline circulation, the nutrients are then brought to the body of the embryo.
Groups of extraembryonic mesodermal cells in the wall of the yolk sac become organized into blood islands (see Figure 6.24 ), and many of the cells differentiate into primitive blood cells. Extraembryonic hematopoiesis continues in the yolk sac until approximately the sixth week, when blood-forming activity transfers to intraembryonic sites, especially the liver. The yolk sac has recently been shown to be the site of origin of a lineage of lymphoid cells that gives rise to microglia in the brain, Langerhans cells in several types of epithelia, populations of tissue macrophages, and mast cells. Previously these cells were considered to be descendants of a stem cell population residing in the bone marrow. Some of these precursor cells migrate from the yolk sac to the liver when hepatic hematopoiesis has begun.
The normal amount of amniotic fluid at term is typically 500 to 1000 mL. An excessive amount (>2000 mL) is hydramnios . This condition is frequently associated with multiple pregnancies and esophageal atresia or anencephaly (a congenital anomaly characterized by gross defects of the head and often the inability to swallow [see Figure 8.5 ]). Such circumstantial evidence supports the important role of fetal swallowing in the overall balance of amniotic fluid exchange. Too little amniotic fluid (<500 mL) is oligohydramnios . This condition is often associated with bilateral renal agenesis (absence of kidneys) and points to the role of fetal urinary excretion in amniotic fluid dynamics. Oligohydramnios can also be a consequence of preterm rupture of the amniotic membrane, which occurs in approximately 10% of pregnancies.
There are many components, both fetal and maternal, in amniotic fluid; more than 200 proteins of maternal and fetal origin have been detected in amniotic fluid. With the analytical tools available, much can be learned about the condition of the fetus by examining the composition of amniotic fluid. Amniocentesis involves removing a small amount of amniotic fluid by inserting a needle through the mother’s abdomen and into the amniotic cavity. Because of the small amount of amniotic fluid in early embryos, amniocentesis is usually not performed until the thirteenth or fourteenth week of pregnancy. Amniotic fluid has bacteriostatic properties, which may account for the low incidence of infections after amniocentesis is performed.
Fetal cells present in the amniotic fluid can be cultured and examined for various chromosomal and metabolic defects. More recent techniques now permit the examination of chromosomes in the cells immediately obtained, instead of having to wait as long as 2 to 3 weeks for cultured amniotic cells to proliferate so they are suitable for genetic analysis. In addition to the detection of chromosomal defects (e.g., trisomies), it is possible to determine the sex of the fetus by direct chromosomal analysis. Many cells of the amniotic fluid have been shown to possess stem cell properties. Whether amniotic stem cells are able to differentiate into such a wide variety of mature cell types as embryonic stem cells remains to be established.
A high concentration of α- fetoprotein (a protein of the central nervous system) in amniotic fluid is a strong indicator of a neural tube defect. Fetal maturity can be assessed by determining the concentration of creatinine or the lecithin-to-sphingomyelin ratio (which reflects the maturity of the lungs). The severity of erythroblastosis fetalis (Rh disease) can also be assessed by examination of amniotic fluid.
The yolk sac is also a temporary residing place for primordial germ cells during their journey from the epiblast to the gonads (see Figure 1.1 ). According to one hypothesis, their residence outside the body proper during this active period of development provides them a respite from the many growth factors and other developmental signals that are involved in shaping the embryo. In this relatively protected environment, the germ cells are able to consolidate the programs necessary for maintaining their totipotency.
As the tubular gut forms, the attachment site of the yolk stalk becomes progressively less prominent, until by 6 weeks it has effectively lost contact with the gut. In a small percentage of adults, traces of the yolk duct persist as a fibrous cord or an outpouching of the small intestine known as Meckel’s diverticulum (see Figure 15.16A ). The yolk sac itself may persist throughout much of pregnancy, but it is not known to have a specific function in the fetal period. The proximal portions of the blood vessels of the yolk sac (the vitelline circulatory arc) persist as vessels that supply the midgut region.
The allantois arises as an endodermally lined ventral outpocketing of the hindgut (see Figure 7.1 ). In the human embryo, it is just a vestige of the large, saclike structure that is used by the embryos of many mammals, birds, and reptiles as a major respiratory organ and repository for urinary wastes. Similar to the yolk sac, the allantois in a human retains only a secondary function, which, like the yolk sac, is served by the blood vessels that differentiate from its mesodermal wall. In the allantois, the secondary function is respiration. The allantoic blood vessels form the umbilical circulatory arc, consisting of the arteries and veins that supply the placenta (see Figure 6.31 ). (The postnatal fate of these vessels is discussed in Chapter 18 .)
The allantois proper, which consists of little more than a cord of endodermal cells, is embedded in the umbilical cord. Later in development, the proximal part of the allantois (called the urachus ) is continuous with the forming urinary bladder (see Figure 16.21 ). After birth, it becomes transformed into a dense fibrous cord (median umbilical ligament), which runs from the urinary bladder to the umbilical region (see Figure 18.21 ).
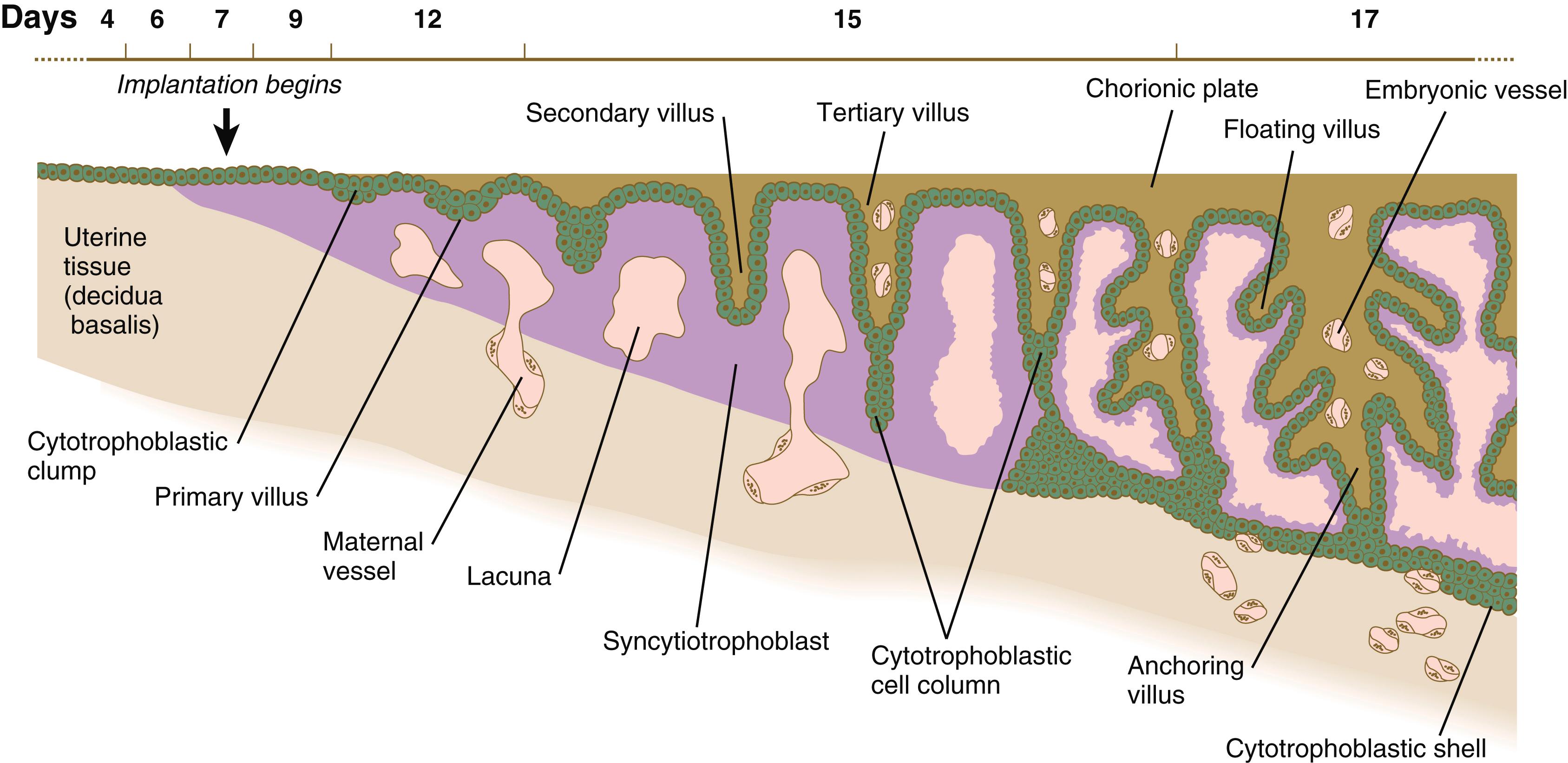
Formation of the placental complex represents a cooperative effort between the extraembryonic tissues of the embryo and the endometrial tissues of the mother. (Early stages of implantation of the embryo and the decidual reaction of the uterine lining are described in Chapter 4 .) After implantation is complete, the original trophoblast surrounding the embryo has undergone differentiation into two layers: the inner cytotrophoblast and the outer syncytiotrophoblast (see Figure 4.20D ). Lacunae in the rapidly expanding trophoblast have filled with maternal blood, and the connective tissue cells of the endometrium have undergone the decidual reaction (containing increased amounts of glycogen and lipids) in response to the trophoblastic invasion.
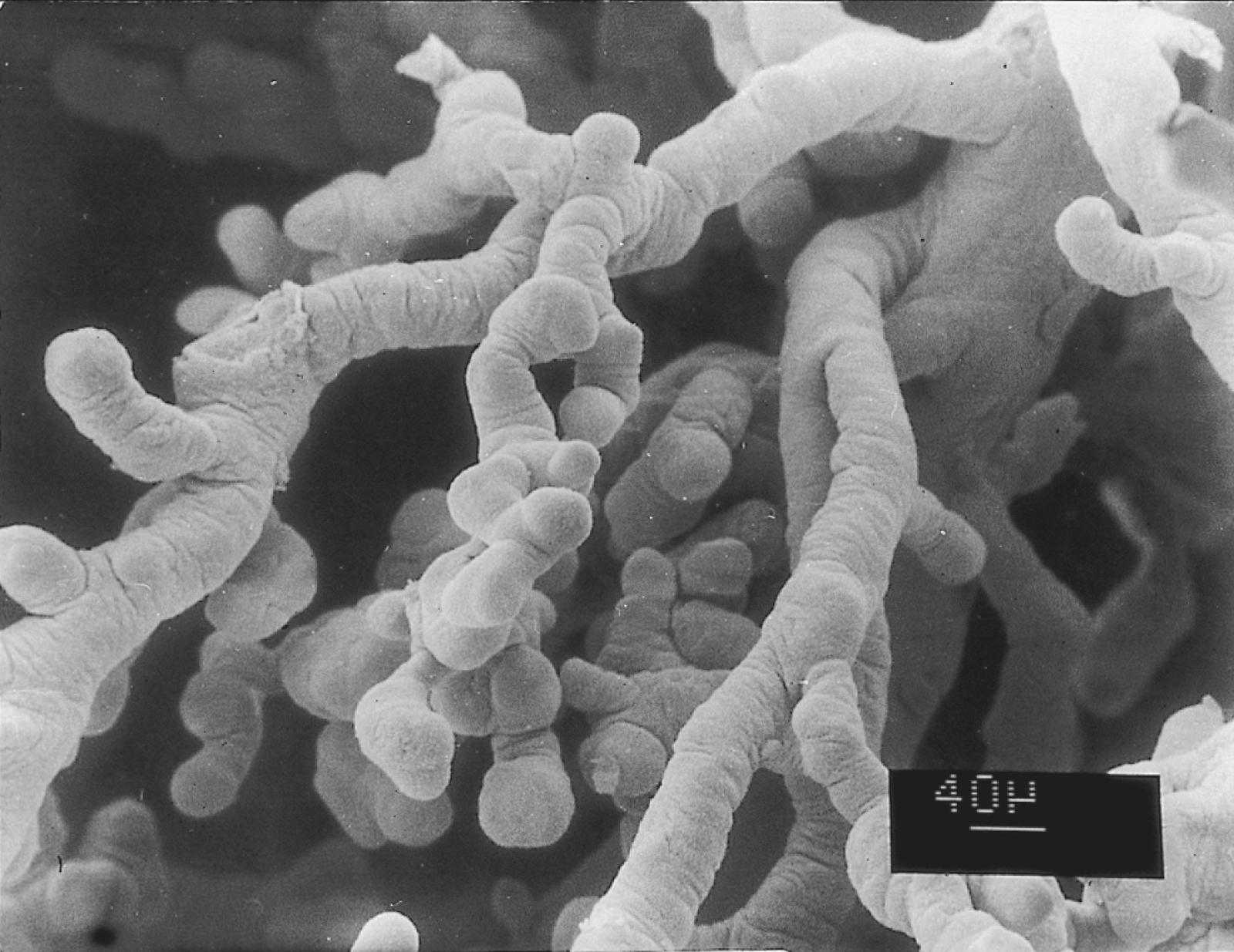
In the early implanting embryo, the trophoblastic tissues have no consistent gross morphological features; consequently, this is called the period of the previllous embryo . Late in the second week, defined cytotrophoblastic projections called primary villi begin to take shape (see Figure 5.2 ). Shortly thereafter, a mesenchymal core appears within an expanding villus, at which point it is properly called a secondary villus ( Figure 7.5 ). Surrounding the mesenchymal core of the secondary villus is a complete layer of cytotrophoblastic cells, and outside of that is the syncytiotrophoblast. By definition, the secondary villus becomes a tertiary villus when blood vessels penetrate its mesenchymal core and newly formed branches. This event occurs toward the end of the third week of pregnancy.
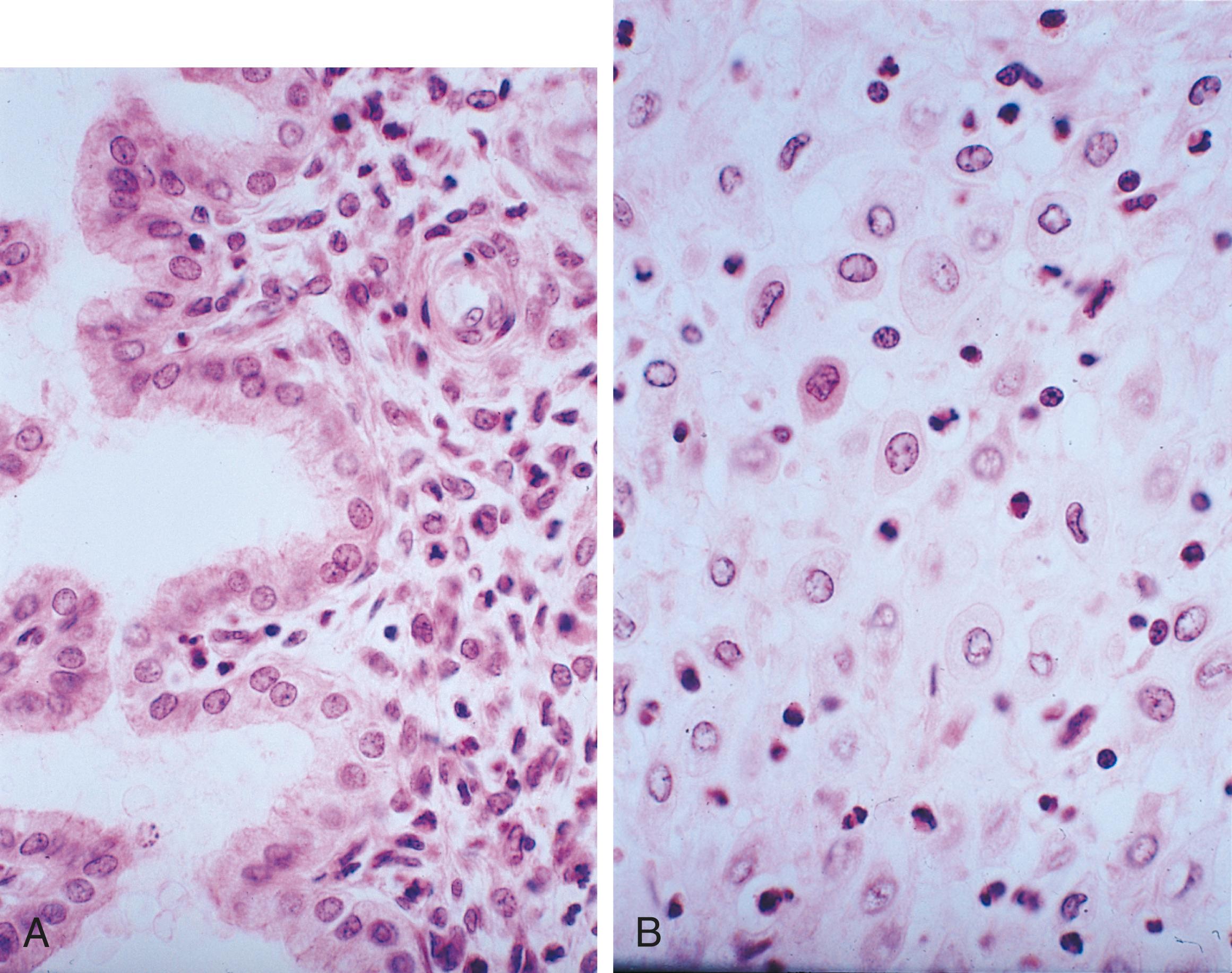
Over the course of pregnancy, the outer syncytiotrophoblastic covering must expand to accommodate the ever-increasing size of both the fetus and the placenta. This is accomplished by asymmetrical divisions of the cytotrophoblastic cells. Early in pregnancy, a solid continuous layer of cytotrophoblastic cells is highly active mitotically. When a cytotrophoblastic cell divides, one daughter cell becomes incorporated into the syncytiotrophoblast, and the other remains within the cytotrophoblast. Cytotrophoblast cells are able to fuse with the syntrophoblast because they begin expressing genes that produce cell fusion proteins that are very similar to those involved in the fusion of the cells that form skeletal muscle fibers (see p. 181). By the end of the tenth week, the uniform cytotrophoblastic sheet breaks up, with spaces between groups of cells. In reality, even though this layer seems discontinuous, the cells within it produce long cytoplasmic processes that through intercellular junctions connect the cells. After a cytotrophoblastic cell has been incorporated into the syncytiotrophoblast, its nucleus remains transcriptionally active and produces a number of cellular products. By approximately 3 weeks, however, these nuclei age and become condensed to form small aggregates called syncytial knots . These are shed into the maternal circulation surrounding the placenta and are carried to the maternal lungs, where they are disposed of by pulmonary macrophages.
Although individual villi undergo considerable branching, most of them retain the same basic structural plan throughout pregnancy. While the placental villi are becoming established, the homeobox-containing genes, Msx2 and Dlx4 ( distalless-4 ), are expressed near the interface between the trophoblast and underlying extraembryonic mesenchyme. These transcription factors are often seen at sites of epitheliomesenchymal interactions. The transcription factor Gem-1 , which promotes an exit from the cell cycle, is expressed at branching points on the villi. Cytotrophoblastic cells on either side of the region of Gem-1 expression continue to proliferate. These cells form the cellular basis of new villous buds.
The terminal portion of a villus remains trophoblastic, consisting of a solid mass of cytotrophoblast called a cytotrophoblastic cell column (see Figure 7.5 ) and a relatively thin covering of syncytiotrophoblast over that. The villus is bathed in maternal blood. A further development of the tip of the villus occurs when, under the influence of the local low-oxygen environment, the cytotrophoblastic cell column expands distally and penetrates the syncytiotrophoblastic layer ( Figure 7.6 ). These cytotrophoblastic cells abut directly on maternal decidual cells and spread over them to form a complete cellular layer known as the cytotrophoblastic shell , which surrounds the embryo complex. The villi that give off the cytotrophoblastic extensions are known as anchoring villi (see Figure 7.5 ) because they represent the real attachment points between the embryo complex and the maternal tissues.
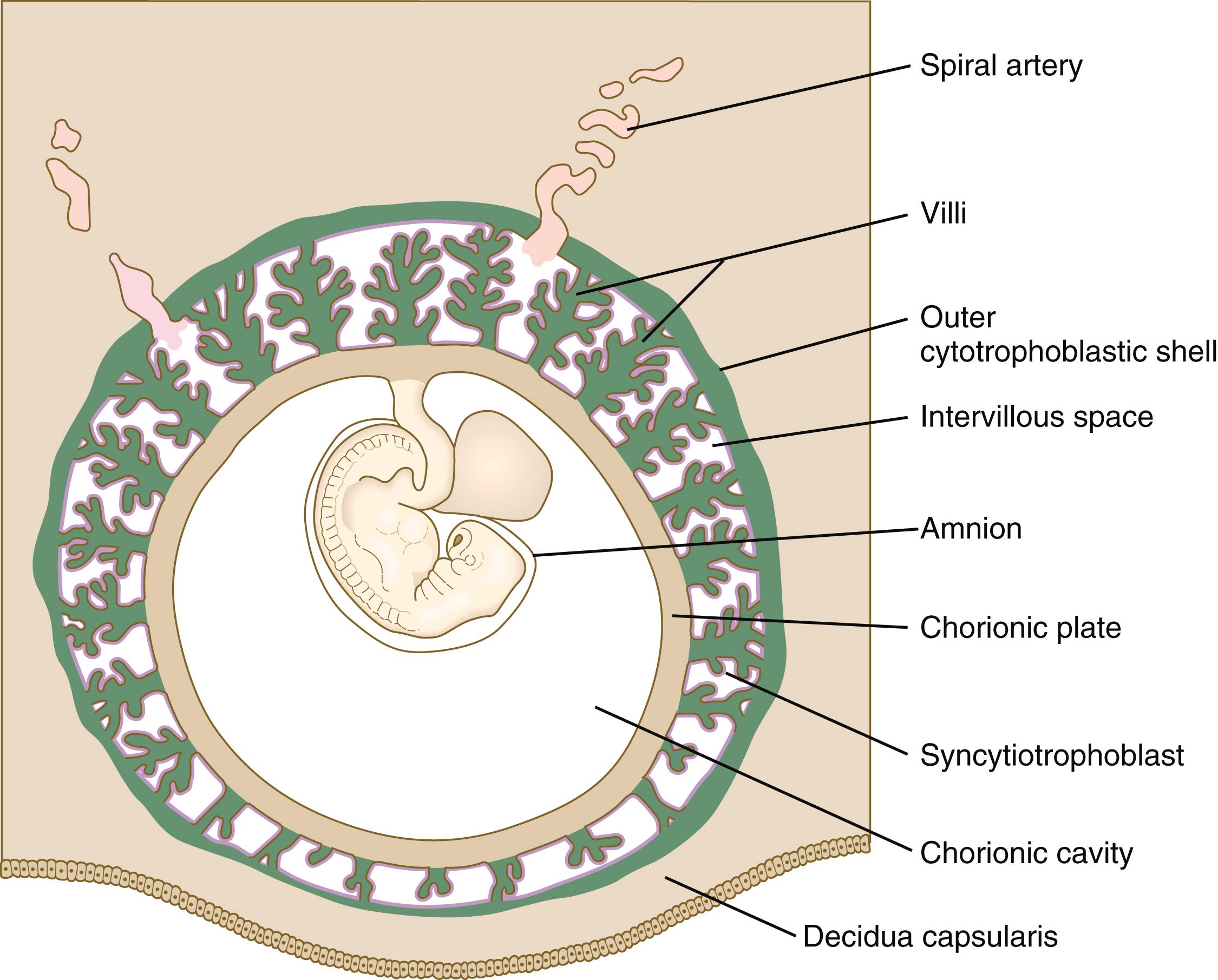
It is important to understand the overall relationships of the various embryonic and maternal tissues at this stage of development (see Figure 7.6 ). The embryo, attached by the body stalk , or umbilical cord , is effectively suspended in the chorionic cavity . The chorionic cavity is bounded by the chorionic plate , which consists of extraembryonic mesoderm overlain with trophoblast. The chorionic villi extend outward from the chorionic plate, and their trophoblastic covering is continuous with that of the chorionic plate. The villi and the outer surface of the chorionic plate are bathed in a sea of continually exchanging maternal blood. Because of this, the human placenta is designated the hemochorial type . ∗
∗ Other mammals have various arrangements of tissue layers through which materials must pass to be exchanged between mother and fetus. For example, in an epitheliochorial placenta, which is found in pigs, the fetal component of the placenta (chorion) rests on the uterine epithelium instead of being directly bathed in maternal blood.
Although chorionic villi are structurally very complicated, it is convenient to liken the basic structure of a villus complex to the root system of a plant. The anchoring villus is equivalent to the central tap root; by means of the cytotrophoblastic cell columns, it attaches the villus complex to the outer cytotrophoblastic shell. The unattached branches of the floating villi (see Figure 7.13 ) dangle freely in the maternal blood that fills the space between the chorionic plate and the outer cytotrophoblastic shell. All surfaces of the villi, chorionic plate, and cytotrophoblastic shell that are in contact with maternal blood are lined with a continuous layer of syncytiotrophoblast.
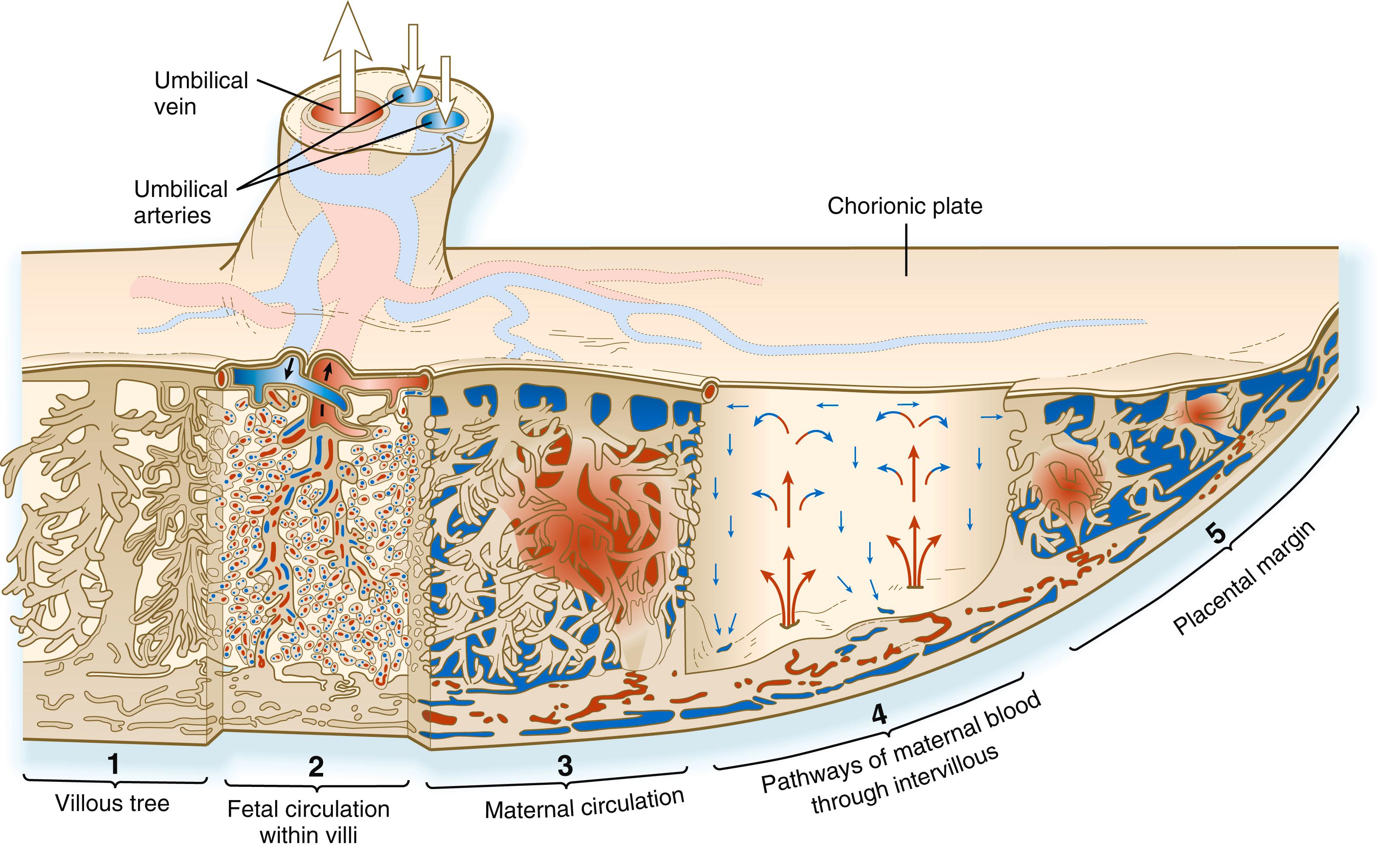
One of the critical features of the developing embryonic–maternal interface is the establishment of a uteroplacental circulation that serves as the medium for bringing food and oxygen to and removing wastes from the embryo. This is accomplished by erosion of the walls of the spiral arteries of the uterus and their modification so that, as the embryo grows, these arteries can provide an increasing flow of blood at low pressure to bathe the syncytiotrophoblastic surface of the placenta (see Figure 7.11 ). Specialized invasive cytotrophoblastic cells , migrating out from the anchoring villi, invade the spiral arteries (but not the veins) and cause major modifications of their walls by secreting a specialized extracellular matrix and displacing many of the normal cellular elements, such as the smooth muscle cells, of the spiral arteries. As a result, the arteries become wider, but the blood escaping from their open ends leaves at a much lower pressure than normal arterial pressure.
The placental circulation and the environment that it creates consist of two phases. For the first 2 months of pregnancy, the cytotrophoblastic cells that invade the spiral arteries essentially form plugs that restrict the flow of blood from the vessels. The first maternal fluid that bathes the embryonic trophoblast is not highly cellular, and the oxygen tension is low. As a result, during the first trimester the spiral arteries contribute relatively little blood to the maternal side of the placenta. This creates a low-oxygen environment ∗∗
∗∗ The partial pressure of oxygen within the placenta at 8 to 10 weeks is two to three times lower than it is after 10 weeks.
for the developing embryo and one in which much of the nutrition supporting embryonic growth comes from secretions of the uterine glands that bathe the outer surface of the placenta (histiotrophic nutrition). In early gestation, low oxygen and glucose levels are important for the development of the embryo. During this period, the placenta grows more rapidly than the embryo. Within the low-oxygen environment of the early placenta, vascular endothelial growth factor (VEGF) is a dominant growth factor, and it promotes angiogenesis within the placenta. Throughout this period, the fetal erythrocytes contain embryonic hemoglobin, which is adapted to bind oxygen under low tension. Starting at 9 to 10 weeks, maternal blood begins to flow through the intervillous spaces of the placenta, and the overall environment for the last two trimesters of pregnancy changes to one that is more highly oxygenated and richer in glucose. The increased oxygen levels downregulate VEGF, and through these and other influences, the fetus now grows faster than the placenta.
Low oxygen stimulates cytotrophoblastic cells to undergo mitosis. This may be one of the environmental conditions that underlies the rapid growth of the cytotrophoblast during the early embryonic period. After 12 weeks, when the maternal blood in the placental space contains large numbers of erythrocytes and is more highly oxygenated (from 2.5% to about 8%), the fetal erythrocytes, through an isoform switch, begin to produce fetal hemoglobin, which requires higher oxygen tension to bind oxygen efficiently. The maternal blood that leaves the spiral arteries freely percolates throughout the intervillous spaces and bathes the surfaces of the villi. The maternal blood is then picked up by the open ends of the uterine veins, which also penetrate the cytotrophoblastic shell (see Figure 7.11 ).
During implantation of the embryo, the stromal cells of the endometrium undergo a striking transformation called the decidual ∗
∗ The term “deciduum” refers to tissues that are shed at birth. These include the extraembryonic tissues in addition to the superficial layers of the endometrial connective tissue and epithelium.
reaction . After the stromal cells swell as the result of the accumulation of glycogen and lipid in their cytoplasm, they are known as decidual cells ( Figure 7.7 ). The decidual reaction spreads throughout stromal cells in the superficial layers of the endometrium. One of the functions of decidual cells is to produce a layer of extracellular matrix proteins that facilitate the inward progression of trophoblastic cells from the embryo. The maternal decidua are given topographic names based on where they are located in relation to the embryo.
The decidual tissue that overlies the embryo and its chorionic vesicle is the decidua capsularis, whereas the decidua that lies between the chorionic vesicle and the uterine wall is the decidua basalis ( Figure 7.8 ). With continued growth of the embryo, the decidua basalis is incorporated into the maternal component of the definitive placenta. The remaining decidua, which consists of the decidualized endometrial tissue on the sides of the uterus not occupied by the embryo, is the decidua parietalis .
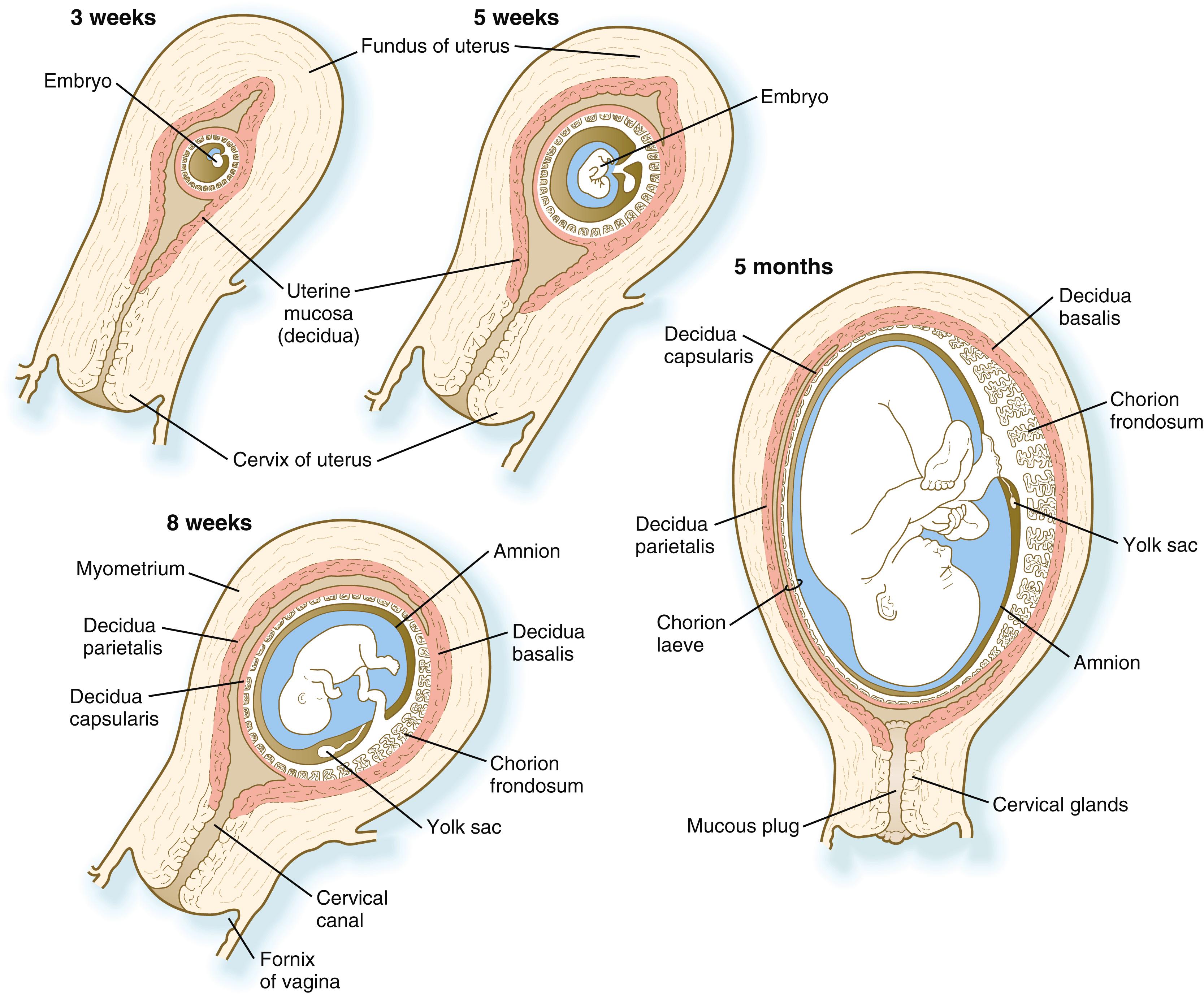
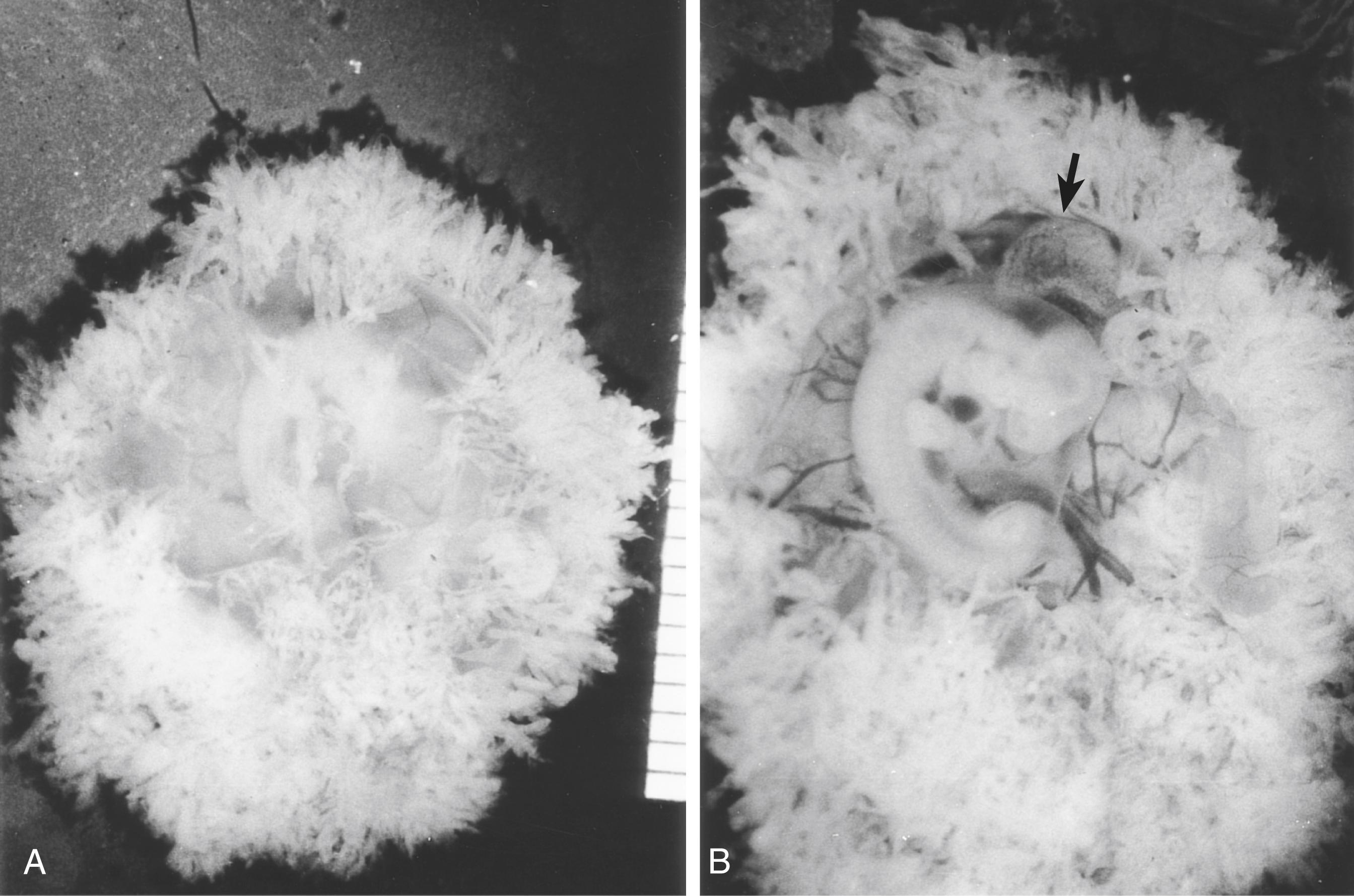
In human embryology, the chorion is defined as the layer consisting of the trophoblast and the underlying extraembryonic mesoderm (see Figure 7.1 ). The chorion forms a complete covering ( chorionic vesicle ) that surrounds the embryo, amnion, yolk sac, and body stalk. During the early period after implantation, primary and secondary villi project almost uniformly from the entire outer surface of the chorionic vesicle. The formation of tertiary villi is asymmetric, however, and the invasion of the cytotrophoblastic core of the primary villi by mesenchyme and embryonic blood vessels occurs preferentially in the primary villi located nearest the decidua basalis. While these villi continue to grow and branch, the villi located on the opposite side (the abembryonic pole) of the chorionic vesicle fail to keep up and eventually atrophy while the growing embryo complex bulges into the uterine cavity (see Figure 7.8 ). The region that contains the flourishing chorionic villi and that ultimately becomes the placenta is the chorion frondosum . The remainder of the chorion, which ultimately becomes smooth, is the chorion laeve ( Figure 7.9 ).
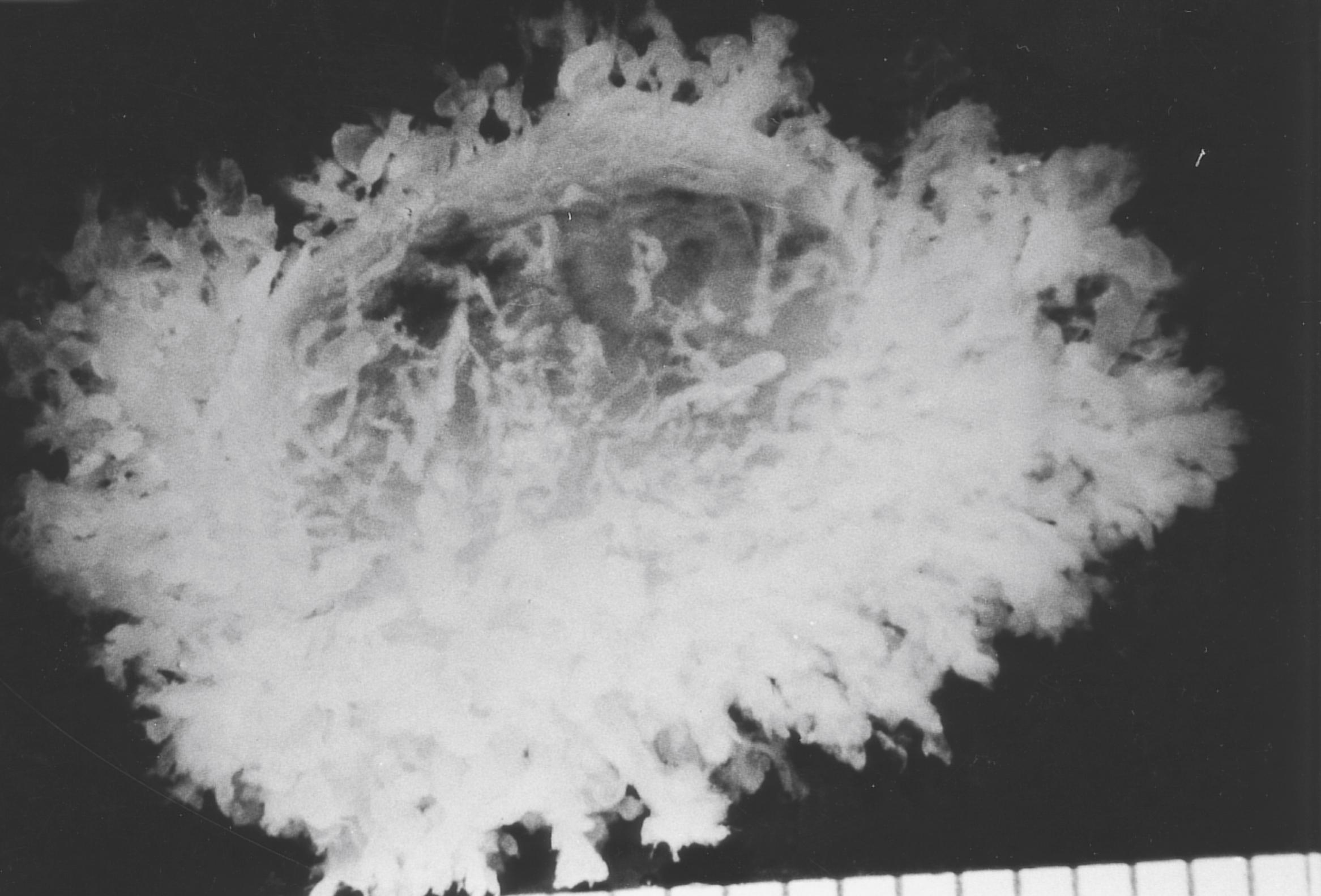
One suggested mechanism for the formation of the chorion laeve is based on oxidative stress. The normal early embryonic environment is roughly equivalent to 3% oxygen versus the normal 21% atmospheric oxygen level. The uterine spiral arteries in the region of the future chorion laeve are not as tightly sealed by cytotrophoblastic plugs as those under the area of the future placenta. This situation leads to a significant local increase in oxygen concentration, thus causing degeneration of the syncytiotrophoblast that covers the villi and the regression of the capillary circulation within them as a result of oxidative stress.
The overall growth of the chorionic vesicle ( Figure 7.10 ), with its bulging into the uterine lumen, pushes the decidua capsularis progressively farther from the endometrial blood vessels. By the end of the first trimester, the decidua capsularis itself undergoes pronounced atrophy. Within the next month, portions of the atrophic decidua capsularis begin to disappear and leave the chorion laeve in direct contact with the decidua parietalis on the opposite side of the uterus (see Figure 7.8 ). By midpregnancy, the decidua capsularis has fused with the tissues of the decidua parietalis, thereby effectively obliterating the original uterine cavity. While the chorion laeve and decidua capsularis are undergoing progressive atrophy, the placenta takes shape in its definitive form and acts as the main site of exchange between the mother and embryo.
While the distinction between the chorion frondosum and chorion laeve becomes more prominent, the limits of the placenta proper can be defined. The placenta consists of a fetal and a maternal component ( Figure 7.11 ). The fetal component is the part of the chorionic vesicle represented by the chorion frondosum. It consists of the wall of the chorion, called the chorionic plate , and the chorionic villi that arise from that region. The maternal component is represented by the decidua basalis but covering the decidua basalis is the fetally derived outer cytotrophoblastic shell. The intervillous space between the fetal and maternal components of the placenta is occupied by freely circulating maternal blood. In keeping with its principal function as an organ-mediating exchange between the fetal and maternal circulatory systems, the overall structure of the placenta is organized to provide a very large surface area (>10 m 2 ) for that exchange.
The mature placenta is disklike in shape, 3-cm thick, and approximately 20 cm in diameter ( Table 7.1 ). A typical placenta weighs approximately 500 g. The fetal side of the placenta is shiny because of the apposed amniotic membrane (see Figure 7.16 ). From the fetal side, the attachment of the umbilical cord to the chorionic plate and the large placental branches of the umbilical arteries and vein radiating from it are evident.
| Age of Embryo (Weeks After Fertilization) | Placental Diameter (mm) | Placental Weight (g) | Placental Thickness (mm) | Length of Umbilical Cord (mm) | Embryo Weight (g)/ Placental Weight (g) | Villous Mass (g) | Total Villous Surface Area (cm 2 ) | Diffusion Distance From Maternal to Fetal Circulation (μm) | Mean Trophoblastic Thickness on Villi (μm) |
|---|---|---|---|---|---|---|---|---|---|
| 6 | — | 6 | — | — | 0.18 | 5 | 830 | 55.9 | 15.4 |
| 10 | — | 26 | — | — | 0.65 | 18 | 3020 | — | — |
| 14 | 70 | 65 | 12 | 180 | 0.92 | 28 | 5440 | 40.2 | 9.6 |
| 18 | 95 | 115 | 15 | 300 | 2.17 | 63 | 14,800 | 27.7 | 9.9 |
| 22 | 120 | 185 | 18 | 350 | 3.03 | 102 | 28,100 | 21.6 | 7.4 |
| 26 | 145 | 250 | 20 | 400 | 4.00 | 135 | 42,200 | — | — |
| 30 | 170 | 315 | 22 | 450 | 4.92 | 191 | 72,200 | 20.6 | 6.9 |
| 34 | 195 | 390 | 24 | 490 | 5.90 | 234 | 101,000 | 11.7 | 5.2 |
| 38 | 220 | 470 | 25 | 520 | 7.23 | 273 | 125,000 | .8 | 4.1 |
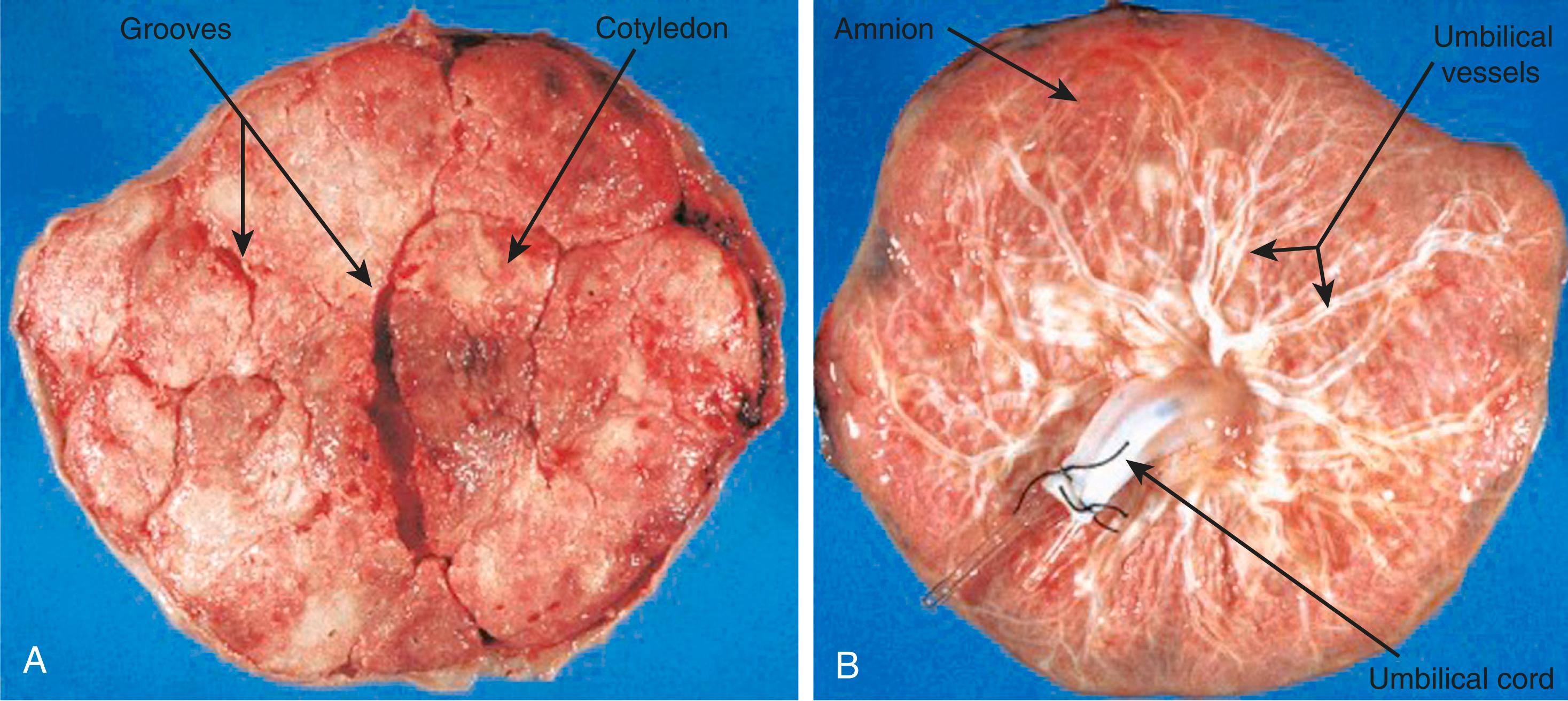
The maternal side of the placenta is dull and is subdivided into as many as 35 lobes. The grooves between lobes are occupied by placental septa, which arise from the decidua basalis and extend toward the basal plate. Within a placental lobe are several cotyledons, each of which consists of a main stem villus and all its branches. The intervillous space in each lobe represents a nearly isolated compartment of the maternal circulation to the placenta.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here