Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A 58-year-old Asian-American male with no other significant past medical history presents to the clinic with acute herpes zoster in the left T4 dermatome. The patient endorsed severe localized pain and tactile allodynia associated with a vesicular eruption. After three months, the rash resolves, but he complains of severe burning pain, allodynia, and hyperalgesia in the left T4 dermatomal region, suggesting that he has developed post-herpetic neuralgia (PHN). Nortriptyline 10 mg was prescribed, but shortly after starting the medication, he developed severe sedation, orthostatic hypotension, and xerostomia. Nortriptyline was then discontinued, and tramadol was initiated. However, the patient did not tolerate tramadol either. A third medication was then trialed hydrocodone/acetaminophen, but yet again, the patient responded poorly. Lastly, gabapentin 300 mg nightly was prescribed and titrated over several weeks to a target dose of 1800 mg/day in three divided doses. This medication slightly alleviated the neuropathic pain, but it was still not well-controlled, and the patient return for further assessment and treatment. It took over six weeks to select and titrate a medication that achieved any notable pain reduction in this specific patient.
This patient was treated according to available evidence-based guidelines, yet he did not obtain adequate analgesia from the prescribed medications. Clinicians recognize that each individual patient responds differently to pain itself, and in the same fashion, response to medications varies from person to person. Advances in pharmacogenomics can help providers understand how genetic variations affect drug metabolism and response, thus offering clinicians the opportunity to identify the most appropriate pharmacotherapy before prescribed and improve patient-specific outcomes. Appropriate knowledge and utilization of pharmacogenomics can allow for the individualization of medication selection.
In the case described, the patient’s inadequate pain relief requires a careful evaluation of the potential reasons rendering the medication ineffective. For example, nonadherence, drug interactions, pain mechanism, or a combination of these could be factors limiting medication efficacy. It is also important to consider the patient’s genetic makeup affecting medication metabolism, thus impacting efficacy and toxicity. This is where pharmacogenomics can play a crucial role in pain management. The case illustrates the variable response and adverse event profile that might be observed when analgesics are prescribed. As noted, clinicians are keenly aware of how often individuals may not obtain the expected therapeutic benefit from analgesic medications across several pharmacologic medication classes.
The response rates in well-designed studies of various analgesic therapies are approximately 55%. This “treatment success” rate is muddled by favorable analgesia to placebo. A large number of patients will not respond to initial therapy. Many key areas of medicine are similarly affected by poor responder rates in clinical trials of diverse drug types. A clear understanding of how pharmacogenomic factors influence the effect of a prescribed analgesic could allow clinicians enhanced analgesic treatment outcomes.
Pharmacogenomics is the study of the impact of genetics on pharmacotherapeutic responses and tolerability. It is used to improve drug safety and efficacy through genetically guided, individualized treatments. As previously noted, the same drug can be associated with different clinical responses among various populations. This is because each individual’s unique genetic composition (i.e. genotype) provides the blueprint for the generation of singular protein expression profiles (i.e. phenotype), which subsequently leads to functional variations observed as clinical responses. Considering such genetic predisposition and receptor subtype expression can result in improved outcomes or resolution of disease. This approach is undoubtedly at the core of personalized medicine. When the clinician is aware of a patient’s genetic predisposition and receptor subtype expression, this knowledge may lead to more individually focused prescribing with improved efficacy and safety for the patient. Key terms used in pharmacogenomics can be viewed in Table 13.1 .
| Genome | The entire collection of genetic information (or genes) that an organism possesses |
| Genotype | The genetic constitution of an individual, either overall or at a specific gene |
| Heterozygous | The presence of two different alleles (one on the maternal chromosome and one on the paternal chromosome) at a gene location |
| Homozygous | The presence of two identical alleles at a gene location |
| Isoform | A variant in the amino acid sequence of a protein |
| Messenger RNA | An RNA-containing single-strand copy of a gene that migrates out of the cell nucleus to the ribosome, where it is translated into a protein |
| Mutation | A rare variant in a gene, occurring in less than 1% of a population |
| Pedigree | A diagram depicting heritable traits across two or more generations of a family |
| Phenotype | The observable characteristics of a cell or organism, usually resulting from the product coded by a gene (genotype) |
| Polymorphism | The existence of two or more variants of a gene in a population, with at least 1% frequency of the less common variant |
| Prodrug | A medication that is inactive until it is converted enzymatically to its active metabolite |
| Single nucleotide polymorphism (SNP) | A single base-pair change in a DNA sequence compared with the “common” or “wild-type” sequence |
| Variant allele | The allele at a particular SNP that is the least frequent in a population |
| Wild-type allele | The allele at a particular SNP that is most frequent in a population also called the “common” allele |
The utilization of genetic information in clinical practice has far-reaching implications. The benefit of utilizing information derived from pharmacogenomics in the future of clinical medicine may lead to improved success rates, decreased side effect burdens, and reduced healthcare costs. For example, the clinical integration of genetic information is routinely used in oncology to guide treatment. , Other areas of medicine are also beginning to tailor pharmacotherapies based on an individual’s genetic information, and certain biomarkers are now known that can help guide treatment in many areas of medicine, including pain management and rheumatologic diseases. Pharmacogenomic testing has benefited patients and clinical medicine in general by improving the ability to stratify the risks of various treatments for individual patients by identifying groups of patients with a higher potential for poor efficacy or for adverse treatment effects ( Table 13.1 ).
The most commonly observed DNA sequences of a gene are termed “wild-type,” and the less common alleles are “variants” if they occur in more than 1% of the population. The even less prevalent alleles have another name; DNA sequences in genes found in less than 1% of the population are called “mutations.”
Pharmacogenetics can allow clinicians to predict medication’s pharmacokinetics and pharmacodynamics and can also help identify patients who are more prone to certain genetically associated diseases. For example, within pain management, an autosomal dominantly inherited peripheral neuropathy, hereditary sensory, and autonomic neuropathy type I confers insensitivity to pain mediated through the progressive degeneration of the dorsal root ganglia and motor neurons as the result of mutations within a specific location in chromosome 9. , Individuals with this genetic background cannot perceive pain, making them particularly prone to painless but potentially severe injuries, with detrimental complications, such as chronic skin ulcers and distal amputations. Kirsh and colleagues studied the polymorphism of a population in Louisiana by administering pharmacogenomic testing to all new patients. Based on 388 tests conducted, 42.3% of individual tests were extensive metabolizers (normal), 25.5% were intermediate metabolizers, 7.2% were ultra-rapid metabolizers, and 7.0% were poor metabolizers; 18% exhibited indeterminate results from inadequate DNA samples or unknown polymorphism. The authors noted that the study yield abnormal pharmacogenetic testing in nearly 40% of patients. In contrast, some studies have found that 83% of patients have abnormal CYP450 defects compared to 20% to 30% of the general population and that other sources found results consistent with the population of Louisiana studied. The growing body of evidence indicates that polymorphism can vary even among subpopulations, thus limiting the generalizability to other pain clinic samples.
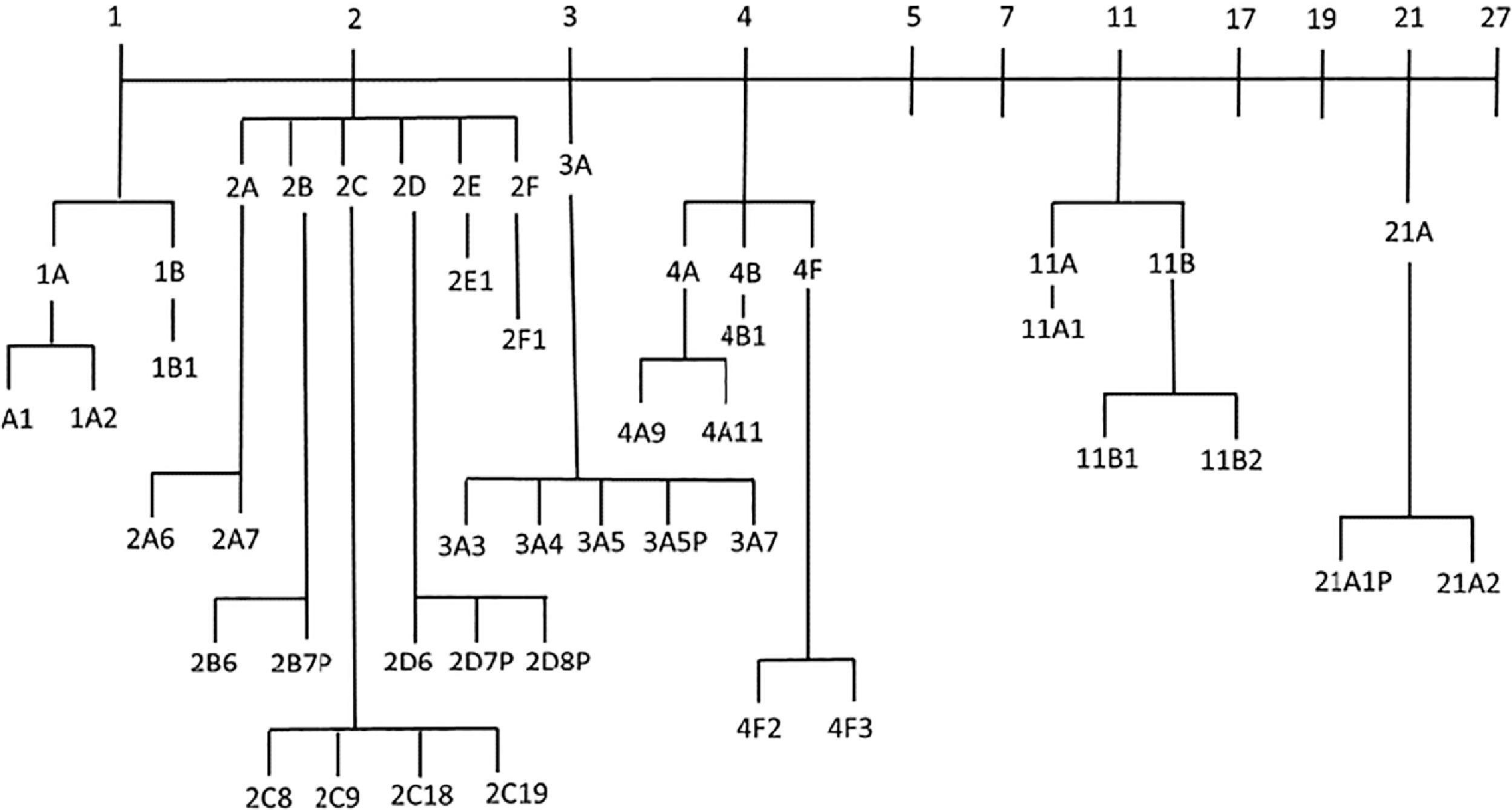
In terms of efficacy, toxicity, pharmacokinetics, metabolism, and drug transport, differences in clinical response to pain medications have been linked in part to genetic variations. To understand how pharmacogenomics can guide medication selection, it is important first to review how drugs are metabolized. Most medications are primarily metabolized in the liver. Hepatic metabolism occurs through phase I reactions, phase II reactions, or both. Phase I reactions are most commonly catalyzed by the cytochrome P450 (CYP450) system, whereas phase II conjugation enhances water solubility for excretion. The CYP450 genes encode enzymes responsible for the metabolism of approximately 75% of commonly prescribed medications. CYP450 is classified by gene sequencing, assigned a family number, a subfamily letter, and then a number for the individual enzyme based upon the order in which it was discovered and is outlined in Figure 13.1 . , Individual variations of CYP gene expression results in altered metabolism, impacting drug concentration and response. These CYP variations are dependent on the metabolizer phenotype. Pharmacogenetic testing for variant and wild-type alleles of CYP450 enzyme groups patients by their phenotype. Poor metabolizers who have two nonfunctional enzyme alleles resulting in an inability to metabolize; intermediate metabolizers, who have at least one reduced functional allele of an enzyme; extensive metabolizers, who have at least one functional allele; and ultra-rapid metabolizers, who have multiple copies of a functional allele or an allele with a promoter mutation that confers increased transcription of that gene. , Extensive metabolizers, the typical phenotype, obtain the expected therapeutic benefit and adverse effect profile from standard doses of a drug. In contrast, individuals who are poor metabolizers are at risk of poor efficacy or adverse effects if given a prodrug that is incompletely metabolized because of genetic differences in their liver enzyme systems. For example, a patient who is a poor metabolizer may not be able to convert the parent drug of an opioid into the active metabolite needed for analgesia (i.e. codeine to morphine, tramadol to o-desmethyltramadol). In contrast, ultra-rapid metabolizers can be prone to adverse effects because of higher than expected drug concentrations from enhanced metabolism (i.e. morphine toxicity from rapid metabolism from codeine).
Genetic determinants beyond metabolic enzymes (such as the CYP450 family) also affect an individual’s response to opioid analgesics. These include drug transporters and drug targets such as the µ-opioid receptor gene OPRM1. A common polymorphism of OPRM1 is the substitution of a single nucleotide at position 118 with an adenine substitution by guanine. The reported allelic frequencies for this are estimated at 10% to 30% among Caucasians, lower among African Americans, and higher among Asians.
Polymorphism of the OPRM1 gene can result in reduced expression of µ-opioid receptors. There is great interest in this polymorphism because it has been associated with pharmacologic and physiologic consequences affecting not only experimental pain models but also neuraxial opioid use for labor analgesia, postoperative analgesia, and cancer-related pain. Studies have suggested that patients presenting with this genetic polymorphism may require higher doses of opioids for analgesic benefit. The different combinations of these single nucleotide polymorphisms (SNPs) within genes that code for the targets of opioid analgesics (e.g. OPRM1) may result in different clinical effects, and thus knowledge of these for a specific patient could one day allow for improved outcomes for opioid prescribing. In addition to the CYP450 family of enzymes, the µ-receptor gene (OPRM1, p.118A/G), and the catechol-O-methyltransferase (COMT Val158MET), several types of the adenosine triphosphate (ATP)-binding cassette, and subfamily B member one gene (ABCB1) have been extensively studied.
Methylenetetrahydrofolate reductase (MTHFR) and COMT are crucial in opioid and anti-depressant response. Patients with chronic pain often present with comorbid mental health disorders. COMT enzyme regulates the breakdown of serotonin, dopamine, norepinephrine, and putative neurotransmitters, while MTHFR is responsible for converting 5,10-Methylenetetrahydrofolate to 5-Methyltetrahydrofolate to its active, usable form of folate. The COMT Val158MET polymorphism is associated with low COMT activity, resulting in increased concentrations of dopamine and norepinephrine. High concentrations of dopamine are associated with upregulation of opioid receptor expression. Ultimately, patients with the Val158MET variant may require fewer opioids for pain relief. MTHFR polymorphism is associated with folate bioavailability impairment.
It has been determined that the interaction of several polymorphisms likely influences the pharmacokinetics and pharmacodynamics of medications—for example, inherited differences—in drug targets (receptors) and drug metabolism and drug transport. Recognizing that morphine and most clinically used opioids act via the µ-opioid receptor, the concept of µ-receptor multiplicity has been studied with the recognition that different splice variants of the MOR-1 gene exist with the potential to clinically affect the benefits or lack thereof of morphine and other opioid analgesics. This kind of information will likely affect the manner in which clinicians prescribe opioids in the future.
Research continues to demonstrate the necessity of genomic testing, as it can optimize medication efficacy, reduce adverse events, decrease hospitalizations, and even prevent deaths in select cases. Additionally, studies have also concluded cost effectiveness on clinical outcomes when genotyping is performed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here