Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fractures of the phalanges are common injuries, with reported rates of 340,000 per year. The majority occur following an accidental fall followed closely by injuries sustained after being struck by an object or person. While these are common injuries across all ages and demographics, there is a higher incidence in children and adolescents. They are commonly managed nonoperatively however, surgery plays an important role in the treatment algorithm.
The proximal phalanx is a tubular bone that consists of a base, a diaphysis, and a head. It tapers from proximal to distal and exhibits a slight convexity on the dorsum and a slight concavity on its volar surface. This shallow concavity palmarly supports the floor of the flexor sheath. Distally, the head consists of two condyles covered with hyaline cartilage for the proximal interphalangeal (PIP) joint. The radial and ulnar collateral ligaments of the metacarpophalangeal (MCP) joint insert at the base of the proximal phalanx. Distally, tubercles on the corresponding condyles serve as the origins of the radial and ulnar collateral ligaments of the PIP joint. The only tendinous insertion is a portion of the intrinsic muscles. With the exception of the third proximal phalanx, the superficial belly of the dorsal interossei inserts onto the lateral tubercle at the base of the proximal phalanx via the medial tendon.
The osteology of the middle phalanx is very similar to that of the proximal phalanx. It too is a tubular bone, although it demonstrates an hourglass shape in cross section. Distally, the condyles are covered with articular cartilage to form the base of the distal interphalangeal (DIP) joint. Radial and ulnar collateral ligaments arise from a tubercle just proximal to the articular surface on either condyle. The central slip of the extensor mechanism inserts proximally on the dorsum of the middle phalanx; palmarly, the flexor digitorum superficialis (FDS) inserts just distal to the insertion of the volar plate.
The distal phalanx can be divided into a base, a shaft, and the tuft distally. Dorsally, the terminal extensor tendon inserts onto a tubercle. The radial and ulnar collateral ligaments of the DIP joint insert on either side of this tubercle. Palmarly, there is another tubercle where the volar plate of the DIP inserts. The flexor digitorum profundus (FDP) inserts just distal to the insertion of the volar plate. Multiple fibrous septae anchor the palmar skin to the tuft of the distal phalanx, providing support to the pulp of the digit and minimizing displacement of underlying fractures. The germinal matrix of the nail originates just distal to the insertion of the terminal tendon; the sterile matrix supports and adheres to the overlying nail plate.
Proximal phalanx fractures typically present with apex volar angulation, commonly with comminution of the dorsal cortex. The primary deforming force is the central slip, which extends the distal fragment, and the intrinsic muscles, which flex the proximal fragment. The reduction maneuver for these fractures primarily involves flexion at the MCP joint, which decreases tension on the intrinsic muscles and corrects the apex volar angulation by flexing the distal fragment. Malunion of these fractures results in pseudoclawing, where shortening of the proximal phalanx leads to an extensor lag at the PIP joint.
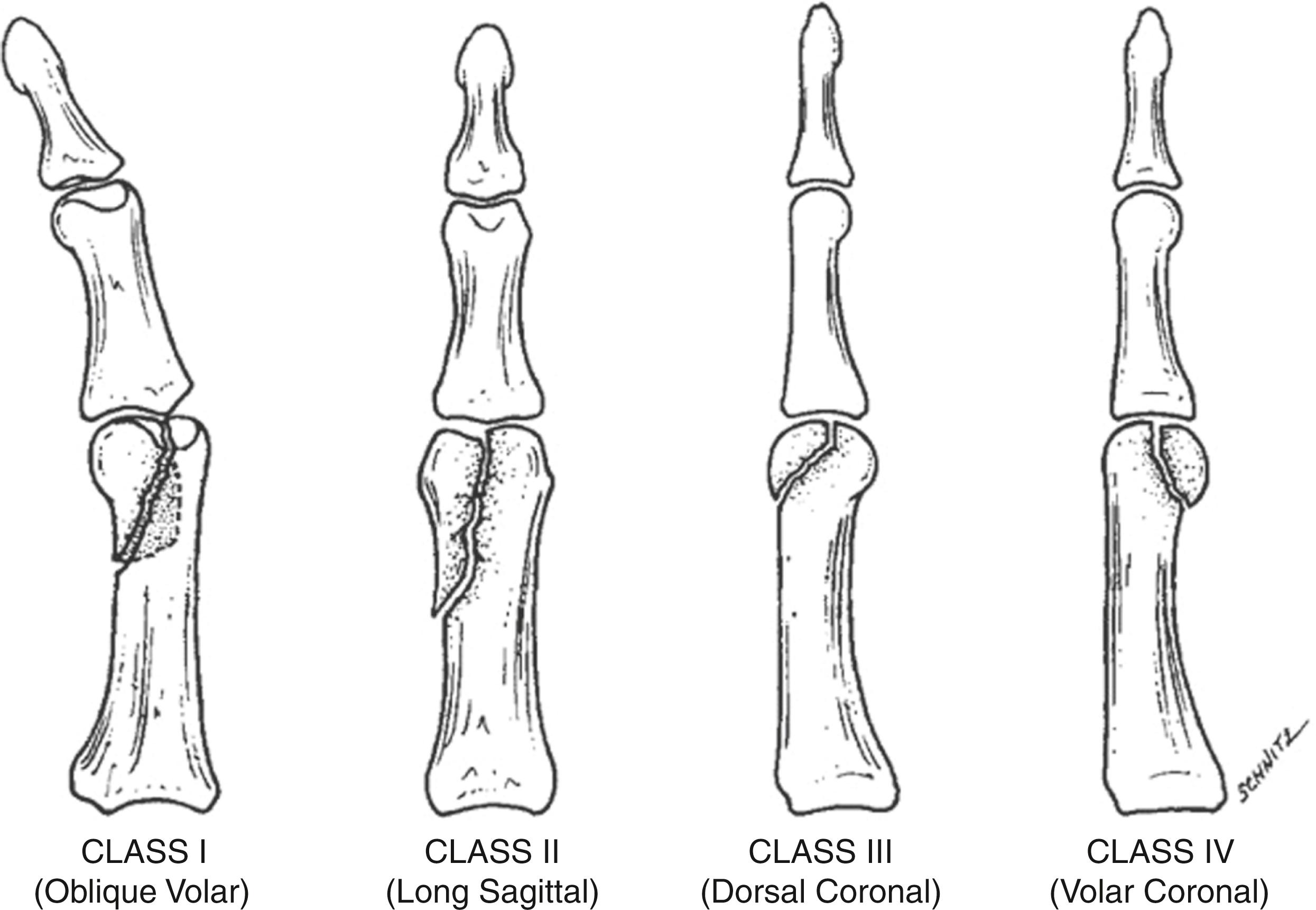
Condylar fractures of the proximal phalanx are relatively common injuries. Though the exact mechanism of injury can vary, they can occur following a combination of axial loading with a shear stress through the PIP joint. Given the typical oblique pattern of these fractures, they are inherently unstable which could lead to articular incongruity. London first classified these injuries: type 1 fractures are stable unicondylar injuries without displacement, type 2 fractures are unicondylar and unstable with any degree of displacement, and type 3 are bicondylar injuries ( Fig. 78.1 ). Weiss and Hastings recommend that unicondylar fractures undergo open reduction for any degree of displacement, owing to the inherent instability of this fracture pattern. They also commented that coronal plane injuries portend a poor prognosis, given disruption to the blood supply at the time of injury.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here