Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pulmonary edema is defined as an excess of fluid in the extravascular compartment of the lung and is classified into four categories based on pathophysiology: hydrostatic edema, permeability edema with diffuse alveolar damage, permeability edema without diffuse alveolar damage, and mixed edema resulting from hydrostatic and permeability edema. Permeability pulmonary edema is almost always a manifestation of capillary endothelial injury or alveolar epithelial damage with resultant loss of fluid and protein into the airspaces or interstitium. Less commonly, permeability edema may occur in the absence of diffuse alveolar damage, such as in patients with the hantavirus pulmonary syndrome or after interleukin therapy. Patients who have permeability edema were originally classified clinically into two groups: those with acute lung injury and those with acute respiratory distress syndrome (ARDS). However, this definition, which was recommended by the American-European Consensus Conference in 1994, was refined in 2011, with the new outline being referred to as the Berlin definition . That updated definition removes the term acute lung injury and includes four clinical criteria for a diagnosis of ARDS. Those criteria focus on (1) timing (acute onset within 1 week of clinical insult or onset of respiratory symptoms), (2) chest imaging (bilateral opacities representing an airspace process on chest radiography or computed tomography [CT]), (3) origin of edema (respiratory failure not fully explained by cardiac failure or fluid overload), (4) oxygenation (now based on PaO 2 /FiO 2 [partial pressure of oxygen in arterial blood/forced inspiratory oxygen] ratio while on 5 cm of continuous positive airway pressure [CPAP]). The three categories of oxygenation are mild (PaO 2 /FiO 2 of 201–300), moderate (PaO 2 /FiO 2 of 101–200), and severe (PaO 2 /FiO 2 of ≤100).
The majority of patients who are at increased risk for the development of ARDS can be classified into two categories: pulmonary (or direct injury) and extrapulmonary (or indirect injury). The main causes of direct lung injury are pneumonia and aspiration; the main causes of indirect lung injury are sepsis, major trauma, and multiple transfusions. A large cohort study reported that the most common risk factor is severe sepsis with a suspected pulmonary source, followed by severe sepsis with a suspected extrapulmonary source. In some series, sepsis (pulmonary or extrapulmonary), pneumonia, aspiration of gastric contents, and major trauma account for more than 85% of causes of ARDS. Other more rare causes include burns, drug overdose, near drowning, postperfusion injury after cardiopulmonary bypass, pancreatitis, fat embolism, and high-altitude pulmonary edema.
An accurate estimate of the incidence of ARDS has been hampered by the lack of a uniform definition and the heterogeneity of the causes and clinical manifestations. An early estimate by the National Institutes of Health (NIH) suggested that the annual incidence in the United States was 75 per 100,000 population, and a more recent study from 2005 demonstrated an incidence of 86 per 100,000. It is currently estimated that there are approximately 190,000 case annually in the United States, resulting in 75,000 deaths.
Patients with permeability edema typically present with acute onset of shortness of breath (generally <72 hours after initial onset or inciting event), bilateral parenchymal opacities on imaging, and refractory hypoxemia and no significant evidence of left-sided heart failure.
ARDS is often associated with other organ failure. Patients who die early (within the first 72 hours of ARDS onset [26%–44%]) usually die of the presenting injury or illness that resulted in ARDS. Patients whose deaths occur late (>72 hours after ARDS onset [56%–74%]) most often die of complications (i.e., new organ failures) that arose during the course of ARDS. Although the mortality rate for patients with ARDS has declined from 50% to 70% in the 1980s to 35% to 46% in 2014, the distribution of causes of death has not changed. Sepsis with multiorgan failure is the most common cause of death (30%–50%), whereas respiratory failure results in a smaller percentage of deaths (13%–19%). The increased survival during the past 2 decades is due largely to advances in supportive care, such as dialysis, and a decrease in extrapulmonary organ failure. Nevertheless, survival for those patients who have sepsis syndrome has not changed appreciably.
Results of multivariate regression analyses have shown an association of death due to ARDS with increasing age (>70 years), underlying liver cirrhosis, high McCabe score for prognosis of the underlying disease, high Acute Physiology and Chronic Health Evaluation II (APACHE II) score for general severity, and high Sequential Organ Failure Assessment (SOFA) score for associated multiorgan failure. Pulmonary factors independently associated with mortality are direct lung injury as the cause of ARDS and the extent of oxygenation impairment on day 3 after the onset of ARDS. Semiquantitative evaluation of fibroproliferative changes by high-resolution CT scan in patients with a clinically early stage of ARDS is also an independent predictor of survival and shows a significant inverse association with the number of ventilator-free days (i.e., days without mechanical ventilation).
The histologic features of ARDS are characterized by diffuse alveolar damage and represent a time-dependent, stereotypic response to acute lung injury. The changes can be viewed as evolving from epithelial and endothelial necrosis to alveolar collapse and eventually to fibroblast proliferation and fibrosis. Permeability edema is prominent in the early stages and heralds the onset of rapidly progressive fibroblast proliferation, which predominates in the late phase of disease. The microscopic appearance varies according to both the time interval between injury and biopsy and the extent and localization of the injury. Diffuse alveolar damage has traditionally been divided into three sequential and overlapping phases: the acute exudative phase of edema and hemorrhage, the subacute proliferative phase of organization and repair, and the fibrotic phase of collagen deposition and end-stage fibrosis. The last two phases are designated the fibroproliferative phase. It is of clinical importance that the histologic features of diffuse alveolar damage correlate with the duration of injury more than with its initiating cause.
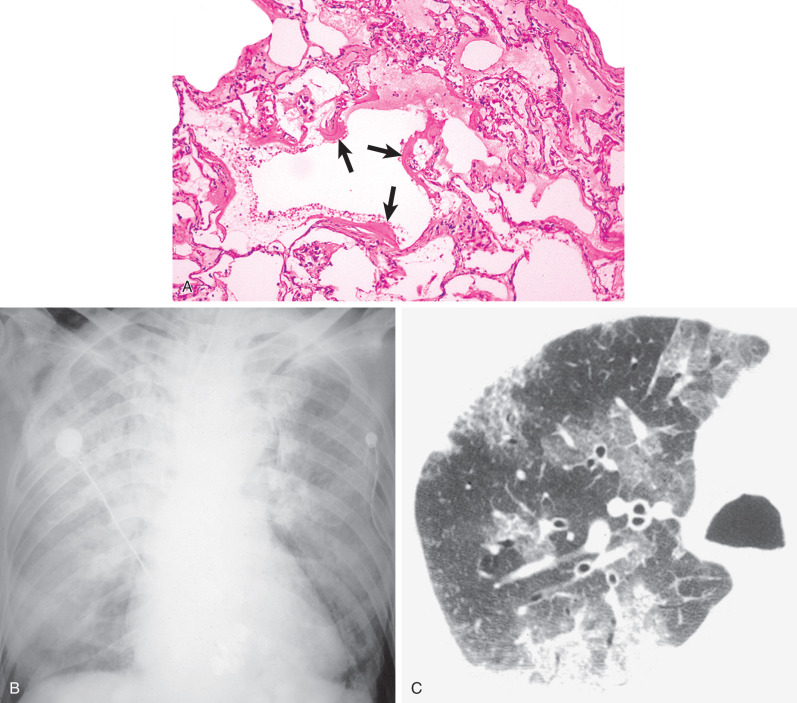
The acute exudative phase predominates within the first 7 days of injury and is characterized by edema, intraalveolar hemorrhage, and hyaline membrane formation ( Fig. 55.1 ). The histologic changes in the early exudative phase consist of capillary congestion, alveolar edema, and intraalveolar hemorrhage. Hyaline membranes, the histologic hallmark of this stage of the lesion, develop later and are most numerous 3 to 7 days after injury. Fibrin thrombi may be seen in the alveolar capillaries and pulmonary arterioles.
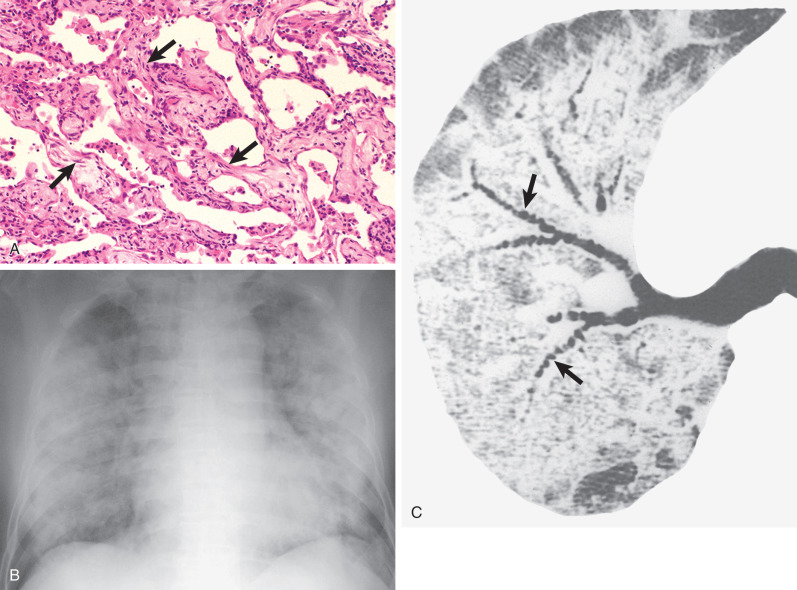
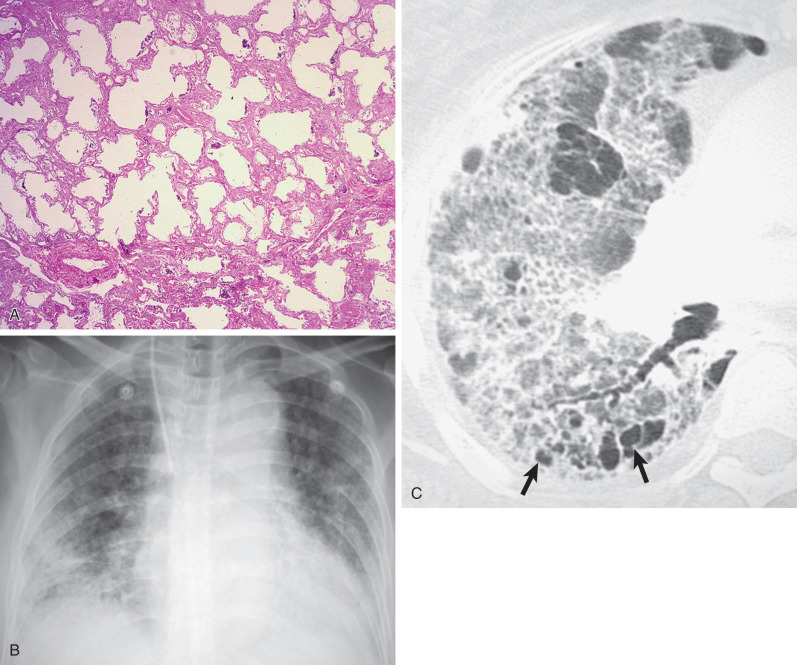
In the subacute proliferative phase of diffuse alveolar damage, fibroblast proliferation, mainly within the interstitium but also within airspaces, becomes prominent ( Fig. 55.2 ). The proliferation of alveolar type 2 pneumocytes, which is seen as early as 3 days after injury and is a reparative phenomenon, occurs in the early proliferative phase and persists throughout this phase. Within the interstitium, fibroblasts and myofibroblasts proliferate and subsequently migrate into fibrinous intraalveolar exudate and convert the exudate to cellular granulation tissue. With the proliferation of fibroblasts (subacute proliferative phase), there is remodeling of the parenchyma, resulting in dilatation of the bronchi (traction bronchiectasis) and bronchioles (traction bronchiolectasis). Subsequently, typically 2 weeks or more after the injury, there is progressive fibrosis with collagen deposition (chronic fibrotic phase; Fig. 55.3 ). Microcystic airspaces 1 mm or larger in diameter (microscopic honeycombing) and traction bronchiectasis and bronchiolectasis are most pronounced in the late fibrotic phase. Cyst-like spaces in end-stage ARDS may also result from chronic interstitial emphysema.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here